Please consider giving to the ED “Adopt a Family Fund” by 12-17
Thanks to Christine Kulstad for her help with this week’s Conference Notes. She better watch out or she’s going to become a regular contributor!
Fakhouri Elbow Injuries
Pediatric ossification centers of the elbow- use the mnemonic CRITOE (capitellum, radial heal, internal [medial] epicondyle, trochlea, olecranon, lateral epicondyle) ossify at ages 1-3-5-7-9-11 in girls, add a year in boys.
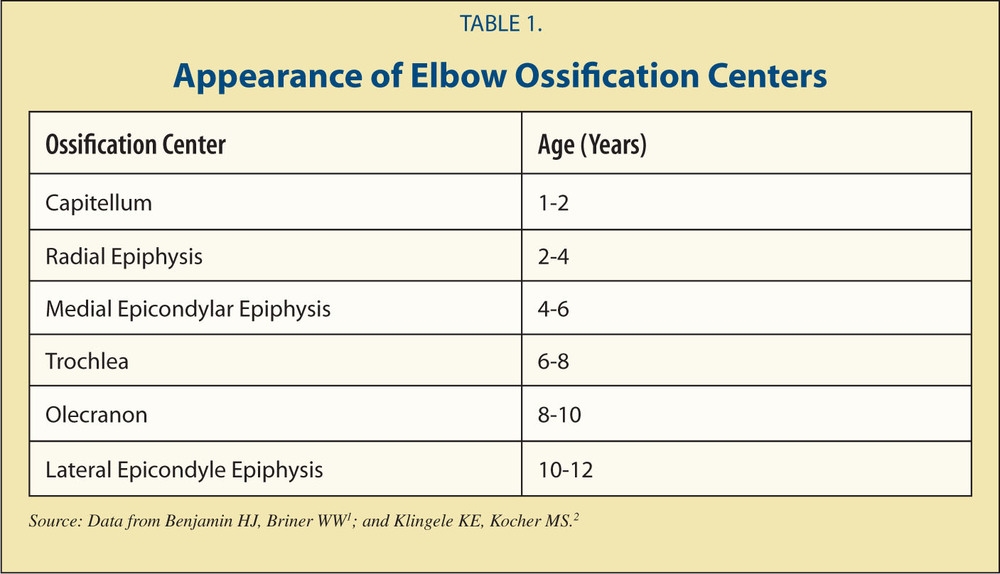
CRITOE
Posterior fat pad is always abnormal. The posterior fat pad is part of the elbow joint, it exists within the deep olecranon fossa normally. When fluid accumulates in the joint, it pushes it out and shows up on xray. Anteriorly, the fossa is much more shallow so the fat sometimes shows up on xray in a normal joint.

Posterior fat pad=fracture
Distal humerus fractures- supracondylar, medial epicondyle, lateral condyle.
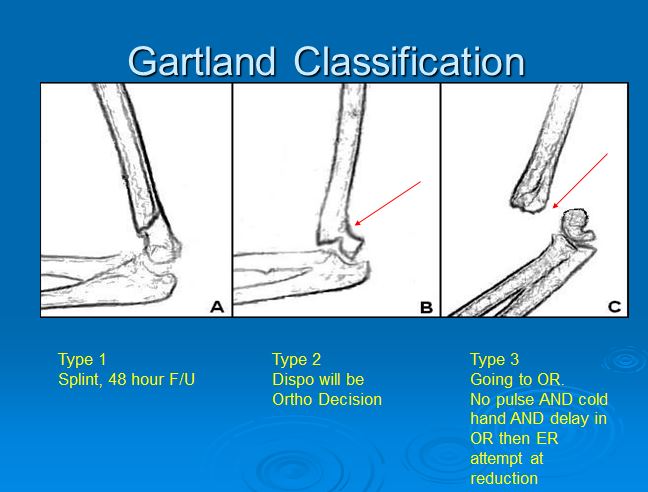
Supracondylar fractures- if non-displaced can be splinted at 90 degrees of flexion and discharged IF you arrange ortho f/u in 2 days and have a reliable patient/family. Any displaced fracture needs surgical intervention. Generally not a good idea to reduce in the ED- should be done by ortho in the OR or with fluoroscopy (c-arm).
Gartland Types of Supracondylar Fractures
Splint the displaced supracondylar fracture in the position of comfort for the patient. Do not force the patient’s elbow into 90 degrees of flexion.
In subtle supracondylar fractures, the anterior humeral line will bisect the anterior 1/3 o the capitellum instead of where it normally bisects the junction of the anterior and middle 1/3’s of the capitellum.

Normal alignment of the anerior humeral line

Supracondylar fracture with posterior fat pad and abnormal anterior humeral line
Heterotopic bone formation can develop around the elbow following supracondylar fractures.
Lateral condyle fractures usually occur when a patient falls on the arm and the arm is in varus position. The tendon can avulse the lateral condyle off the distal humerus. If these injuries are not repaired you develop a valgus deformity and the patient can develop an ulnar neuropathy
There was a discussion of the terms varus and valgus. Varus deformity describes the distal forearm pointing medially toward the midline. Valgus deformity describes the distal forearm pointing lateral from the midline. Mnemonic is to remember the L in valgus reminds you that the distal forearm is pointing laterally from the midline of the patient’s body.

Varus and Valgus
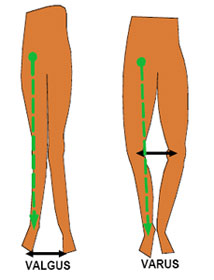
Varus and Valgus
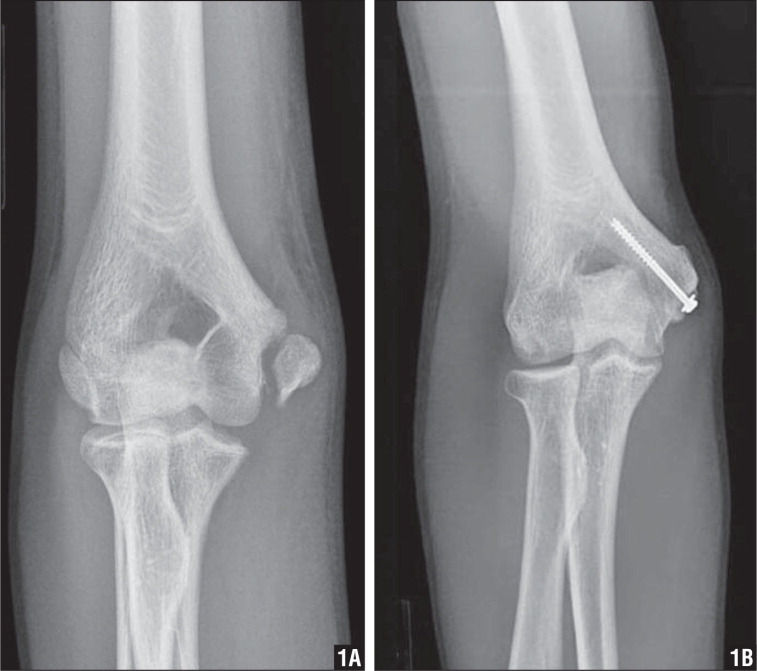
Medial condyle fractures
Normally the medial condyle should be just below the Shenton’s line. If it is not in that location you have to be suspicious for medial condylar fx.
Medial Condyle fracture
Radial head fractures
Splint these injuries initially. Ortho will mobilize them early if non-displaced. 2mm or more of step off or separation of radial head fractures requires surgery.
Olecranon fractures
Any step off or separation of more than 2mm requires surgery.
Elise comment: Of all the above fractures, supracondylar fracture is the most high risk injury that can result in deformity, compartment syndrome, or neurovascular injury. Dr. Fakhouri agreed.
Elbow dislocation
Multiple attempts at joint reduction injures the cartilage. Dr. Fakhouri prefers the prone position technique. If you see an elbow dislocation in kids look for an associated fx.
Distal biceps tendon ruptures always require surgery. Pt will feel a pop or a snap of a rubber band. These occur mostly in patients around 30-40 yrs of age. Older patients will have a proximal tendon ruptures. Proximal tendon injuries don’t need surgery. Both types cause a popeye deformity of the biceps muscle. In proximal ruptures, the muscle will bunch up distally. In distal ruptures, the muscle will bunch up proximally. Treat with a sling in the ED and refer to ortho for surgery. Harwood comment: why not surgically repair proximal ruptures. Fakhouri response: The outcome is the same with non-operative management . Patients actually get back to work more quickly without surgery for proximal injuries. To be clear, distal ruptures all require surgery.
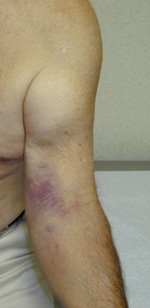
Distal biceps tendon rupture
Erickson M&M
Elderly female with history of DM, HTN, COPD presented with fever, cough, and SOB. Lung exam demonstrated bilat wheezing. Heart was irregular and tachycardic.
At outside clinic patient received med neb and steroids. CXR showed possible pneumonia.
In ED patient received med nebs and IV antibiotics. Labs showed mildly elevated Troponin and minimal bump in creatinine. EKG showed new onset afib. Heart rate was controlled with diltiazem. Heparin was started. Patient was admitted to floor.
While in hospital, pt developed a left rectus sheath hematoma. With that finding, heparin and warfarin were discontinued. Pt coded on day 2 of hospitalization. She was resuscitated. By Day 3 her abdomen was severely distended and had intra-abdominal fluid. It was hypothesized that pt may have had further bleeding in her abdomen.
Anti-thrombotic therapy for AFIb: Use CHADS2 score for risk stratification

CHADS2
Linsey identified a potential system based error with the heparin order set.
Harwood comment: The higher bolus given in the ED is very unlikely to have caused this patient’s outcome. There was generally faculty agreement that the initial heparin bolus was not the cause of the patients death. The decision to anticoagulate is appropriate based on the CHADS2 score. Maggie comment: Unfortunately a high risk CHADS2 score also carries a high risk for bleeding from warfarin.
Take home point: Double check your orders. Verify the patient, the dose. Discussion strayed into other examples of medication errors in kids and adults. One further point, be careful to not be duplicating someone else’s order.
Elise comment: Strong plug for PediStat App for your smartphone. It is a great App for getting ped’s resuscitation drugs right. Harwood comment: We should probably change the Order Set wording for heparin to “Cardiac” and “Non-Cardiac” dosing. Elise comment: Be sure to know dosing of common drugs so you have some reference point to identify incorrect dosing. Harwood comment: This is an elderly woman with influenza who had an nstemi and afib. She then develops a rectus sheath hematoma from coughing and/or heparin. If is totally unclear what was the cause of death.
Lambert Study Guide Resuscitation
Best predictor of survival in setting of cardiac arrest is time prior to resuscitation.
In setting of hyperkalemia, get EKG first to identify cardiac effects of hyperkalemia.
Why use cuffed ET tubes in kids: higher probability to correctly size the ET tube at first intubation attempt. New technology cuffs are also less likely to produce pressure injury.
Mnemonic for sizing peds tubes 1-2-3-4
1x= Et tube size is (age/4) + 4 , 2X =NG size, 3X = Depth of ET tube, 4X =chest tube size.
Atropine is no longer indicated for PEA
Antiarrythmic drugs are not supported in the literature for ventricular arrhythmias in the setting of hypothermia.
Child pulled out of a lake with weak, slow pulse. What is initial management? CPR and ventilation.
Avoid adenosine in pediatric patients with irregular wide QRS tachycardia. Gotta suspect WPW in this patient and procainamide is a better choice.
Bradycardia- maximum dose of atropine is 3 mg
In witnessed VF, the first treatment is CPR. Defibrillation should be done as soon as is available.
Monophasic defibrillators provide more energy than biphasic. Biphasic ones deliver the energy more effectively, so can use less.
After treating paroxysmal SVT with adenosine, the recurrence rate is 50-60%. This is based on one small study and attending experience is that the rate is not this high.
Cuffed pediatric ETT are recommended because the seal is better so airway protection is better. It can be harder to pass the tube through the cords.
Disposable end-tidal CO2 monitors are very (reported at 100%) sensitive in non-arrest patients, and can detect CO2 >2%.
A patient in persistent VF, consider doubling the energy for defibrillation (Lambert used 2 defibrillators at the same time [or 0.5 s after] to successfully get someone out of Vfib after 30 shocks. There was also an EP case series where it worked >50% of the time , in about 18 pts).
Adenosine is dosed 0.1 mg/kg initially, the second dose is 0.2 mg/kg. Remember, it should be pushed very quickly and followed with a saline bolus. The half-life is seconds.
Ventilator settings for a post-arrest patient should be tidal volume of 6-8 ml/kg and rate of 10-12 breaths per min. Use lower lung volumes for patients at risk of ARDS.
Atropine should be used with caution in a patient with Mobitz type II AV bloc with associated BBB due to a potential increased risk of converting to 3rd degree AV block.
The rhythm with the highest chance of survival for an out of hospital arrest is VF (other choices were PEA variants)
Epinephrine use in cardiac arrest is based on animal studies and anecdotal clinical evidence.
The most common adverse effect of IV amiodarone is hypotension- likely due to the diluent. Pulmonary fibrosis is a common long-term side effect.
Procainamide is dosed at 20-50 mg/min to a max of 17 mg/kg, QRS widening, conversion of rhythm, or hypotension.
Pediatric CPR should avoid excessive ventilation, compress the sternum 1.5 inches in infants and 2 inches in children, have a compression rate of 100/min
The most common cause of mortality in AMI patients is cardiogenic shock.
The objective of CPR in PEA/asystole is to delay tissue death until a reversible cause can be found.
In a choking victim, if they can speak one word and cough- you should only encourage spontaneous efforts. When they can’t breathe, you intervene.
When using the ETT for medication administration, increase the dose 2 to 2.5 times.
When you put your defibrillator to the SYNC mode, it delivers energy with the sensing of the QRS complex.
Respiratory distress in peds is best described as increased work of breathing. Signs of respiratory failure includes apnea, bradycardia, cyanosis.
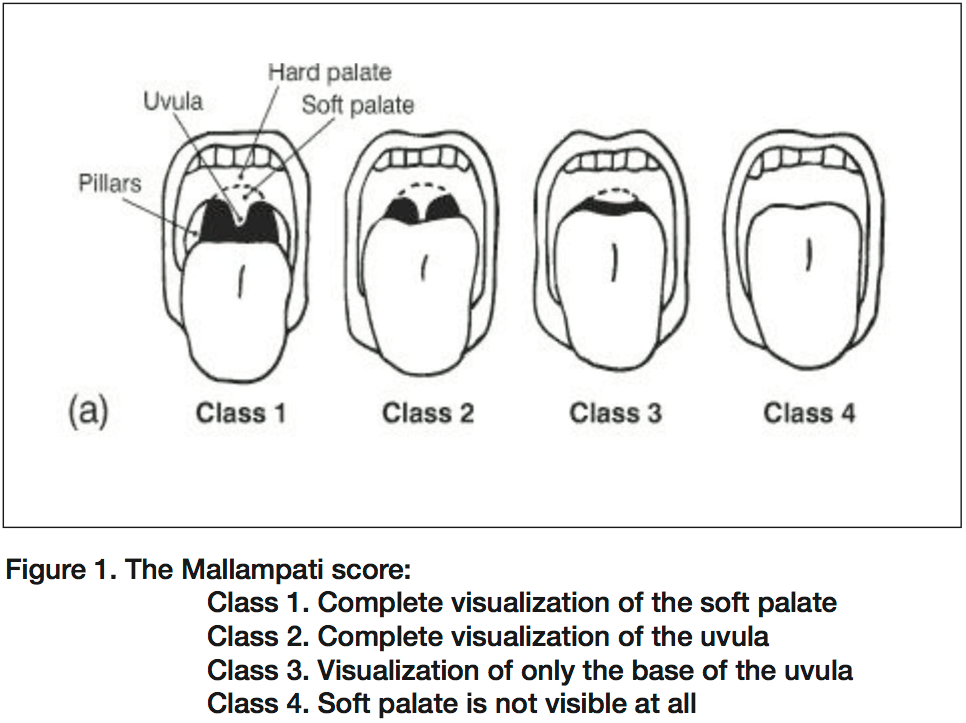
Mallampati score
Balogun Congenital Heart Disease
Cyanosis + Tachypnea + Shock + <1 month = left obstructive CHD until proven otherwise
50-60% of CHD diagnoses after hospital discharge, 30% present to ED in first month of life for 1) poor feeding, 2) cyanosis 3) tachypnea/tachycardia or 4) shock
Ductal dependent lesions present in the 1st month.
-Right heart lesions- pulmonary flow depends on DA- include Tetrology of Fallot, tricuspid atresia
-Left heart lesions- systemic flow depends on DA- include aortic stenosis, hypoplastic left heart,
The ductus arteriosos usually closes 12-15 hrs after birth due to increase O2 and decreased prostaglandin. It is permanently closed by about 3 wks. Delayed closure occurs due to decreased PaO2 in right sided lesions. Baseline O2 sats 75-85%, which drop as ductus closes. The ductus stays open in left sided lesions due to increased pressure. When it closes, kids present in shock, mild cyanosis
Left-right shunting lesions present between 2 and 6 months- VSD, truncus arteriosis. For the first 2-3 months, pulmonary and systemic vascular resistance are equal. At 2-3 months, the pulmonary resistance falls which triggers the shunting and symptoms.
Kids with CHD will also have problems with concurrent illness or metabolic derangements or during physiologic anemia of newborn period.
ED management for CHD kids- Intubate early, keep O2 sats at 80-90%, optimize systemic perfusion.
Airway- anticipate adverse events, Pretreat with atropine 0.01 mg/kg (min 0.1 mg).
-Ketamine- avoid as it can cause pulmonary HTN
-Benzodiazepines- avoid as it can cause hypotension
- Propofol- avoid as it can cause hypotension
-Etomidate- yes!
- Succinylcholine- avoid if possible
-Rocuronium is preferred 1 mg/kg, fast onset
Breathing- keep sats low (80-90%). There is a technical explanation involving Fink’s principle that has to do with balancing flow to pulmonary and systemic beds, but just remember the number
Ventilator settings- Assist control, tidal volume 6-8 ml/kg, rr 20-50, peep 5, FiO2 start low and titrate up
Give PGE1- life saving! Re-opens and maintains patency of ductus arteriosis. Start at 0.05 mc/kg/min and titrate up every 15-20 min until desired effect.
Circulation- Target MAP of at least 40. Bolus with 10 cc/kg. If fluid seems to make them worse, then add dopamine infusion at 5 mcg/kg/min and titrate up to a max of 10 mcg/kg/min. Second line is epinephrine infusion (vs all other situations we use pressors).
Work-up- ABG, CXR, EKG, blood cx, trop, bnp, tsh, cortisol, coags, T&S, CMP, CBC.
Start empiric antibiotic therapy. Give bicarb while trying to restore perfusion (1-2 mEq/kg).
Watch for hypoglycemia and hypocalcemia and treat if they occur.
Regulate the temperature to normal. NG, Foley to monitor UOP, arterial line if able
Resuscitation is critical for post-operative course. Patient must be transferred to center capable of correcting lesion with PICU/PSHU.
Tet spells- in kids with mild TOF. They present with Tet spells, cyanosis treat with COINSPIRES
C- comfort- parents hold child, knees to chest position
O-oxygen
IV fluids- 10 cc/kg
Narcotics- morphine 0.05 -0.1 mg/kg
Sedation- more morphine
Phenylephrine- 10-20 mcg/kg/dose
Intubate (last Resort)
Esmolol- 500 mcg/kg load over 1 min, then infuse 50-300 mcg/kg/min
Harwood comment: the pathophysiology/pharmacology of tetrology is hard to understand. I know I need knee-chest position, oxygen, morphine and a cardiologist. The rest, I don’t know.
Elise comment: If you are giving prostaglandin, be prepared to intubate. Prostaglandin can cause apnea. Pulse ox differentials in upper and lower extremities suggests coarctation.
Give prostaglandins for infant with cyanosis, murmur, weak pulses. (any two)