There are images in this document. If you don’t see them scroll to the bottom and click “read in browser”
Please consider donating to our EM Foundation to benefit resident education/development. Thanks for your consideration/generosity.
/em-foundation/
Conference Notes
Lovell/Cash Resident as Teacher Workshop
What makes a good clinical teacher: clinical knowledge, positive relationships, supportive learning environment, communication, enthusiasm. As you can see, most of these are non-cognitive traits/skills.
Good EM teaching principles: The teacher takes time to teach, gives appropriate feedback, tailors teaching to learner, using teachable moments effectively, positive attitude.
Barriers to teaching: time management, clinical load, interruptions, loud environment, personal motivation, interpersonal issues, dealing with “non-exciting cases”, some learners have very limited knowledge base and finding their knowledge gaps and working with their gaps can be difficult, and physical space limitations.
Research has shown that 70% of medical students feel their supervising residents had a significant role in their learning. They felt that about 30% of their learning came from resident teaching. So the teaching residents do with their students is very important.
Traditional teaching model: Teacher acts as an expert consultant, the model is centered around the teacher, teacher transmits what they know to the students. This model is mostly a one way street. Learners are passive. Learners are uncomfortable exposing their knowledge gaps.
Learner centered model: There is back and forth learning between teacher and student as well as between students. The teacher takes time to find knowledge gaps of learners. Learners demonstrate reasoning and problem solving to teacher. Teacher gives quick, relevant teaching points in a non-threatening manner. Focus is more on learners’ reasoning. Learners are encouraged to ask questions. Learners are active in this process.
One Minute Preceptor Technique: 6 steps (or microskills): 1.Get a commitment (teacher asks specific questions about a case to get the learner to invest themselves such as “ what do you think is going on with this patient?”),2. Ask learner for supporting evidence (teacher is looking for knowledge gaps by asking probing questions such as “What clinical findings suggest endocarditis?”), 3.teach a general principle (give the learner a short pearl or take home point), 4.reinforce what was done well (start with positive feedback on specific aspect of the students clinical reasoning or exam finding), 5.correct mistakes (give corrections in a positive manner) , identify the next learning steps (encourage specific further reading) . Ryan comment: Thinking out loud with the student is very useful. Even just talking about how your are deciding to see which patient first is teaching the student. Mistry comment: Some of the basic mundane tasks we do are still very interesting and novel for students.
SPIT Technique: Serious Probable Interesting Treatable. This is a quick method to develop a differential diagnosis. Have the student give diagnoses for each component of the SPIT acronym for a patient case. You can do it before you see the patient and after you see the patient. For example in a patient with chest pain: Serious would be aortic dissection or ACS, Probable would be chest wall pain or GERD, Interesting would be shingles or pneumothorax or pneumomediastinum, treatable would be ACS/aortic dissection/GERD/Chest wall pain/Pneumothorax.
Harwood comment: To give feedback, you can ask the learner what they think they can do better. That will usually start a useful discussion and give the teacher a non-confrontational way to discuss ways to improve. Always use the PNP sandwich. Positive-Negative-Positive. Tell the learner something positive about their performance, then the specific area of potential improvement, then another positive to build them back up. Mistry comment: Ask student what was the most interesting thing you saw/learned today and then follow up on that with some learning points or suggested reading. Elise comment: You can take that one step further by then telling the student to teach that learning point to someone else. Feedback is important and most students feel they don’t get enough of it. To improve this situation, the teacher should make an announcement to the learner “I am now going to give you some feedback”. Gottesman comment: I tell the student at the start of the shift that I am going to give you feedback at the end of the shift. This prepares the student for that feedback and also encourages them to be invested in the shift all day and to expect feedback. Elise comment: you can give feedback during the shift as well; it doesn’t have to be at the end of the shift. Harwood comment: The teacher’s self critique of their own teaching or clinical care is a very effective teaching technique to students. Harwood comment: If you want to teach on a “boring case,” you can ask questions about the case with one variable changed. Example: abdominal pain + pregnant or +gi bleeding or +afib or +previous surgery. You can ask the learner how they would manage the case with these variables.
Walchuck Trauma Myths
Myth 1.Resuscitate your patient to normal vitals: Truth: In penetrating trauma keep MAP around 65/heart rate in range of 60-100. Barounis comment: This is tough, it your instinct to give a lot of saline to get MAP higher. Resuscitate with blood and plasma. Use lower dose of sedative (avoids worsening hypotension) and higher dose of paralytic (poor perfusion in hypotensive patient). Ketamine can be used. It doesn’t increase ICP. Always Be prepared for patient to arrest during intubation. These hypotensive patients are very unstable. In blunt trauma and closed head injuries, keep MAP up to 105. In non-hemorrhaging injured patients, the brain does better at a higher MAP
Myth 2. In the setting of pelvic trauma, blood at meatus is absolute contraindication to foley placement. Truth: It is reasonable to attempt one gentle pass of a foley catheter. Steve noted there was data to support this approach and that he spoke with the Trauma attendings who have anecdotal success with this method. Girzadas comment: I was hesitant to accept the approach of placing a foley through a bloody meatus without a retrograde urethrogram, but there is a statement from the European Urologic Society 2013 Trauma Guidelines supporting 1 gentle attempt at foley placement prior to urethrogram although they do hedge a bit:
Blood at the meatus is present in 37-93% of patients with posterior urethral injury, and in at least 75% of patients with anterior urethral trauma (31,32). When urethral trauma is suspected an attempt of urethral catheterisation should be carried out by experienced hands and the balloon of the Foley catheter should only be inflated if clear urine flows out. It is extremely unlikely that gentle passage of a urethral catheter will do any additional damage (33,34). Although it has been suggested that passing a catheter may convert a partial tear into one that is complete (35), there are no convincing data indicating that there is a higher rate of infection or urethral stricture after a single attempt at catheterisation (1). However, the most prudent approach is to carry out urethrography prior to an attempted catheterisation. In an unstable patient, an attempt to pass a urethral catheter should be performed, but if there is any difficulty, a suprapubic catheter should be placed using ultrasound guidance and a retrograde urethrogram must be performed once the patient has been stabilised.
Myth 3. Pulse exam rules out extremity vascular injury. Truth: You have to look for hard signs of vascular injury in penetrating trauma: hemorrhage/pulsatile hematoma/bruit or thrill/absent pulse/signs of ischemia. If any hard sign is present in association with a penetrating injury, the positive predictive value is virtually 100%, so patient goes to OR. Hard signs are less reliable in blunt extremity trauma. In patients with a penetrating extremity injury and soft signs only such as a pulse difference, do an ABI. A normal ABI is >0.9. If the ABI is normal then there is no need to image and patient can be observed and have serial ABI’s. If <0.9 then further imaging like a CTA is indicated.
Myth 4. Pelvic exam not necessary in trauma. Truth: Speculum exam can be very important in pelvic fractures to be sure there is no vaginal laceration. Also water skiing or jet skiing injuries can cause serious vaginal tears including intra-peritoneal free air.
Carlson Electrocardiography in Overdose
QRS is affected by na channel blockers like tricyclic antidepressants/cocaine/tegretal/Benadryl
QT interval prolonged by K channel blockers like methadone/macrolides/antipsychotics/ibutilide and amiodarone
ST segment is affected by cocaine/sympathomimetics/ergotamine/cellular asphyxiants like cyanide or CO. This is probably most common in CO poisoning and the recommendation is to go to hyperbaric not cath lab. Most patients who go to cath lab for CO related ST elevation have clean coronary arteries .
U waves are caused by Lithium/methylxanthines/hypokalemia/hypomagnesemia
Case 1. 60yo female, dizzy with ekg showing a lot of deep t wave inversions diffusely looking like subendocardial ischemia. Rhythm looks like afib. Pt had digoxin toxicity. Ekg with dig can have “hockey stick shaped” st changes. Dogoxin inhibits na pump with increases intracellular calcium which in turn increases contractility force. Digoxin also has vagotonic/anti-adrenergic actions.
Case 2. 70yo female who is somnolent. EKG is aflutter and ventricular bradycardia. Pt has classic ekg (atrial tachycardia with block) for digoxin toxicity.
Virtually every dysrythmia has been reported with digoxin toxicity. Bi-directional V-tach is considered pathognomonic for digoxin toxicity.

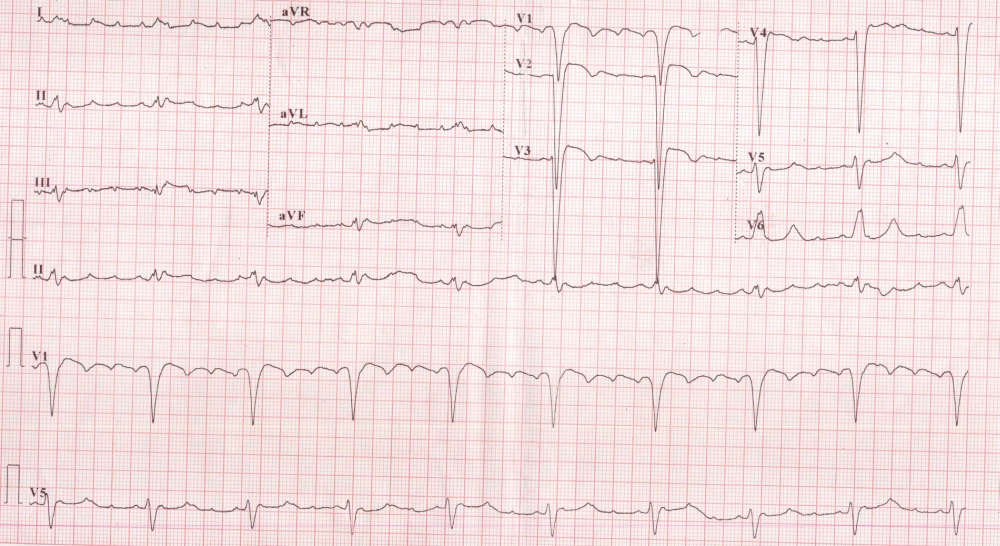
Bidirectional Ventricular Tachycardia
Digoxin also has GI/mental status/vision effects. Increasing potassium levels are an indicator of the severity of digoxin overdose. For patients with V-tach or V-fib. Follow normal ACLS guidelines. The fear of giving calcium in the digoxin toxic patient is overblown. Don’t wait to get digoxin level if patient needs calcium for severe hyperkalemia. Give digibind for K>5.5/ventricular dysrhythmias/slow rate not responding to atropine/combo digoxin and CCC overdose/Digoxin level>10 or ingestion >10mg. Harwood comment: give digibind in hypotensive patients. Digibind takes 20 minutes to work. Renal dysfunction is a common factor in digoxin toxicity.
Case 3. 30yo male with syncope at work. Hx of bipolar dz. EKG with long QT. Pt later went into torsades. Pt was on ziprasidone and was put on erythromycin. This drug combo caused prolonged QT. Elise comment: be careful when considering ibutilide in alcoholic patients. Alcoholic patients tend to be hypomagnesemic and may have prolonged QT interval. Don’t give ibutilide in patients with a long QT. Discussion about zithromax and risk of prolonged QT among attendings: General consensus was that zithromax was safer than other macrolides and was not a risk to patients. Harwood comment: Original study on this issue was a population based study in medicare patients showing some increased risk of death. Later study in Europe of younger patients showed no increased risk of death due to Zithromax.
Case 4. SVT due to caffeine. Methylxanthines include caffeine and theophylline. Methylxanthines will counteract the effects of adenosine. You may have to use higher doses of adenosine. Sympathomimetics and herbal supplements (bitter orange) can cause SVT. Weight loss supplements commonly contain caffeine like substances
Case 5. 19 yo patient took clonazepam and propranolol. EKG showed sinus brady with brugada pattern. Brugada pattern can develop from various toxins. If brugada pattern develops from toxin, the patient does not need an AICD. The patient does not have a chronic cardiac conduction abnormality, they are suffering from a transient toxic effect. TCA’s and cocaine can do this.
Case 6. TCA overdose. EKG shows TCA pattern is prolonged QRS, Tall terminal R wave in AVR.
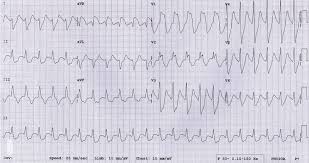
TCA EKG
TCA’s are dirty drugs with multiple pathophysiologic mechanisms. These mechanisms include Antihistamine/alpha blocker/na channel blocker/k channel blocker/GABA blocker. Treat seizures with benzos. Second line anti-seizure med is phenobarb. Avoid phenytoin in TCA overdose. Avoid 1a and 1c class antiarrythmics and beta and calcium blockers. Main antidote for cardiac effects is sodium bicarb. Sodium bicarb doesn’t really work on neuro effects like seizures. Shoot for a serum ph of 7.5-7.55. Give bicarb for QRS>100/severe acidosis/hypotension/cardiac arrest. 6 hour observation period will declare the “sick” vs “not sick “ patient. Harwood comment: TCA’s can have a “ Catastrophic demise”.
Case 7. 19yo took overdose of valium. EKG shows complete heart block. You can google the imprint code on a pill to identify what drug it is. The ER docs found that the patient didn’t actually take valium but mistakenly took verapamil. Treat CCB’s with calcium/atropine/glucagon/high dose insulin/intralipid
