Conference Notes 7-23-2013 Another Great Conference Day!
If you can't see the pictures scroll to the bottom and click on "Read in Browser"
Please consider donating to our EM Foundation to benefit resident education/development. Thanks for your consideration/generosity.
/em-foundation/
Putman/Lovell Oral Boards
Case 1 5 day old infant with malrotation and midgut volvulus. Recognize bilious emesis in an infant. Malrotation with midgut volvulus usually presents in the first week of life. Duodenal atresia usually occurs in first day of life. Get a KUB then follow that with upper GI and emergent surgery consult. This is an ischemic condition that can evolve to death.
Case2 Jones fx of 5th MT.
This is a diaphyseal FX of the 5th MT that is distinct from an avulsion FX of the tuberosity of the 5th MT. Jones fractures occur in an area of relatively poor blood supply and are at risk of nonunion if the patient continues to weight bear on this Fx. One way to identify a Jone’s FX is to see if the FX line extends into the space between the 5th and 4th metatarsals.
Case3 Cryptococcal Meningoencephalitis Get a CT in HIV patients prior to doing an LP. Get Crypto AG of bood and CSF. Treat with amphotericin and flucytosine. High opening pressure carries a poor prognosis and requires hi volume taps and repeated LP’s to drain CSF fuid.
Elise was Gracious enough to give me all her notes:
Malrotation with midgut volvulus: In patients with midgut malrotation, the usual gut rotation ceases after the first 90 degrees, and the duodenum and ascending colon are juxtaposed around the superior mesenteric vessels, with the entire midgut suspended from this narrow axis. The malrotated bowel itself does not cause any significant problem. However, because of the narrow axis, the midgut can at any time twist around the axis. The tighter the twist, the more the midgut suffers from obstruction of the lumen, obstruction of venous and lymphatic return from the midgut, and obstruction of arterial inflow, thus threatening midgut viability. Unless it is treated in a timely manner, bowel strangulation results in an ischemic loss of extensive bowel, causing death if not treated.
In neonates, malrotation with midgut volvulus classically presents with bilious vomiting and high intestinal obstruction. While most neonates with bilious vomiting do not have midgut volvulus, this diagnosis must be ruled out. Older children with malrotation may manifest a failure to thrive, chronic recurrent abdominal pain, malabsorption, or other vague presentations.
Malrotation and volvulus should be suspected in all cases of proximal small-bowel obstruction, especially in infants. Most patients with midgut malrotation develop volvulus within the first week of life. Besides the cardinal clinical manifestation of bilious vomiting, clinical features may include pain (colicky at first, then steady), anorexia, blood and mucus in the stool, abdominal tenderness, and, eventually, shock.
In early cases, patients may appear well, and abdominal examination findings may be normal. In fact, normal findings on abdominal examination have been reported in as many as 50% of patients. Because the obstruction is very proximal, abdominal distention is not usually present.
An upper GI series is the preferred diagnostic test for malrotation with midgut volvulus and must be performed. Upper GI series sensitivity is 85-95%, with a higher specificity. In malrotation with midgut volvulus, upper GI à dilated, fluid-filled duodenum, a proximal small bowel obstruction, a "corkscrew" pattern of the jejunum. Malrotation without volvulus on upper GI seriesà duodenal jejunal junction is displaced downward and to the right on frontal view. KUB of malro without volvulus is often nml. KUB of malro with volvulusà classic finding is a partial duodenal obstruction (dilation of both the stomach and proximal duodenum, with a small amount of distal bowel gas).

Double bubble sign. S=stomach D=duodenum

UGI showing midgut volvulus
Ultrasonography and CT may suggest the diagnosis of malrotation; however, their sensitivities and specificities are low compared with those of an upper GI series.
Duodenal obstruction, seen in midgut volvulus and malrotation, is also seen with duodenal stenosis, duodenal web, annular pancreas, preduodenal portal vein, and duodenal atresia (atresia presents within first hours of life, double bubble, may delay surgery 24-48 hours, assoc. with Down’s).
Labs: may have initial hypochloremic metabolic alkalosis. As they get sicker, think metabolic acidosis, gut ischemia, necrosis, perforation/peritonitis, sepsis/death. Mortality up to 15%. Long term complication short gut syndrome.
Jones fracture:
The diaphyseal bone, where the fracture occurs, is an area of poor blood supply; a watershed area between two blood supplies. This makes healing difficult. In addition, there are various tendons, including the peroneus brevis and fibularis tertius, and two small muscles attached to the bone. These may pull the fracture apart and prevent healing.
If the fracture enters the intermetatarsal joint, it is a Jones fracture. If, however, it enters the tarsometarsal joint, then it is an avulsion fracture caused by pull from the peroneus brevis. An avulsion fracture is sometimes called a Pseudo-Jones fracture or a Dancer's fracture. Avulsion fracture can be treated with walking cast, Jones must be non-weight bearing.
Jones fx is located at least 1.5 cm distal to tuberosity of 5th metatarsal & should not be confused with the more common avulsion fracture of the fifth metatarsal styloid which is usually proximal to the metatarsal cuboid joint and treated with walking cast or cast shoe.

Jones FX Fracture line extends to 4-5 intermetatarsal space
Cryptococcosis is the most common fungal disease in HIV -infected persons, and it is the AIDS-defining illness for 60-70% of HIV-infected patients.
In addition to invading the lung and CNS, cryptococci also invade the skin, bone, and genitourinary tract, but meninges appear to be the preferred site.
Cryptococcal disease usually develops only when CD4+ lymphocyte counts fall below 100 cells/microL.
Disease onset is usually insidious; time from symptom onset to diagnosis is, on average, 30 days or more. The delay also may be due to the waxing-and-waning course and the nonspecificity of symptoms. Headache, fever, malaise, nonspecific mental status sx, uncommonly CN palsies, seizures, focal neuro sx. Also uncommon to see meningismus (no immune system).
CSF analysis may yield normal (ie, reference) results in 25% of patients and may be minimally abnormal in as many as 50%; therefore, identifying the organism via India Ink and serology is crucial.
Increased intracranial pressure (>200 mm H2 O) occurs in over half of all patients with AIDS who have cryptococcal CNS infection, probably because of obstruction of the basal meninges or impaired CSF absorption. Since increased intracranial pressure is a poor prognostic factor (increased mortality) whose correction leads to symptomatic improvement, this must be managed aggressively.
In the absence of obstructive hydrocephalus or risk of herniation, increased pressure (>250 mm H2 O) can be relieved by serial spinal taps or a lumbar-peritoneal shunt. Daily lumbar puncture removing approximately 30 mL of CSF until the pressure has decreased 50% is recommended.
Close to 100% of CSF culture results are positive for Cryptococcus neoformans, whereas 66-80% of blood culture results are positive. India ink stain is positive in 74-88% of infected patients.
CrAg in the serum usually is indicative of systemic disease and correlates with fungal burden. A localized cryptococcal infection, such as pulmonary cryptococcosis without lymph node involvement, usually is not associated with a positive serum CrAg; a positive result warrants a search for disseminated disease. Detection of CrAg in either serum or CSF has >95% sensitivity and specificity in the diagnosis of true invasive cryptococcal infection. Cryptococcal capsular polysaccharide antigen in spinal fluid is now the method of choice for diagnosing patients with cryptococcal meningitis.
Twenty to thirty percent of patients show meningeal enhancement, parenchymal solid mass lesion without hemorrhage (granuloma), atrophy, cerebral edema, or hydrocephalus on CT/MRI. If the imaging studies show a cryptococcal mass lesion (ie, cryptococcoma), toxoplasmosis and lymphoma must be considered in the differential diagnosis; brain biopsy may be indicated.
If left untreated, cryptococcal CNS infections are fatal. Mortality rate of 6%, despite aggressive therapy, has been reported.
Current guidelines from the Infectious Diseases Society of America (IDSA) for primary therapy of cryptococcal meningitis in HIV-infected patients recommend amphotericin B deoxycholate (0.7-1.0 mg/kg/day IV) plus flucytosine (100 mg/kg/day orally in 4 divided doses) for at least 2 weeks. This is followed by fluconazole (400 mg [6 mg/kg] per day orally) for a minimum of 8 weeks).
Lifelong secondary prevention may be required. Relapses occur if secondary prevention is stopped or becomes ineffectual. Relapse rates without prevention range from 15-27%; this drops to 0-7% with prophylactic antifungal agents.
Predicting CD4 count by absolute lymph count. If ALC < 1,000, CD4 likely < 200.
Acad Emerg Med. 2011 Apr;18(4):385-9.
Absolute lymphocyte count in the emergency department predicts a low CD4 count in admitted HIV-positive patients.
Napoli AM, Fischer CM, Pines JM, Soe-lin H, Goyal M, Milzman D.
866 patients known to be HIV+ and admitted from the ED, who had an ALC measured in the ED and a CD4 count measured within 24 hours of admission. An ALC of <950 × 10(6) cells/μL has a sensitivity of 76% (95% CI = 73% to 79%), specificity of 93% (95% CI = 87% to 96%), and positive likelihood ratio of 10.1 (95% CI = 8.2 to 14) for a CD4 count of <200 × 10(6) cells/μL.
Prophylaxis (another way to guess CD4 count, based on antibiotics patient is taking)
PCP CD4 <200, bactrim
Toxo CD4 < 100, bactrim
MAC CD4 < 50, Zithromax
Erik comment: When doing an opening pressure during an LP, the patient has to be laying down in the lateral decubitus position. Measuring the opening pressure with the patient sitting up will be inaccurate.
Harwood comments: HIV patients with headaches should get CT brain with IV contrast. You can get a closing pressure instead of an opening pressure. So if you want to not risk your ability to get CSF from an LP, you can get the fluid first and then lay them down and measure the pressure. Removing 8ml of CSF will not completely resolve the increased pressure.
Kettaneh M and M Case F/U’s
Case 1 Missed distal femur buckle fx in a young child. Elise comment: Gotta carefully palpate the entire extremity. If the child won’t bear weight you have to xray the entire extremity if you can’t find palpable tenderness.
Case 2 55 yo female with exertional near syncope and blurry vision. In hospital, it was found patient had central retinal artery occlusion. Nick felt that he could have communicated with the consultants better in the ED because in their note the mentioned possible CRAO but he did not speak with them.
Nick recommends that you follow up the hospital course on most of his patients. You learn a lot of stuff by doing this. Elise comment: I call some patients, especially the one’s I am worried about. Patients invariably really appreciate this.
Case 3 49yo male bunt trauma to face and amnestic to events. HGB noted to be 8.7. Pt was observed in ER. Pt developed epistaxis in the ED. Nick asked the nurse to put some packing in the patient’s nose. Pt was not re-assessed for hours. Pt became unresponsive. He was successfully resuscitated. Repeat labs and multiple CT’s after pt was resuscitated showed no clear cut etiology of what happened to patient. The suspected etiology was that nasal packing stimulated the nasopulmonary reflex causing apnea/bradycardia/hypoxia/bronchoconstriction. At Dr. Lovell’s suggestion, pt was cooled using our therapeutic hypothermia protocol. Pt gradually improved over weeks.
Consider the risk of nasopulmonary reflex whenever you a pack pt’s nose.
Girzadas comment: this patient’s risk of the nasopulmonary reflex may have been higher because the patient was head injured, had elevated ammonia level, was older and had pulmonary comorbidities. Lovell comment: I am more conscious of this potential complication and really think about sending home a patient who is elderly or has multiple comorbidites with a nasal pack. McKean comment: You will never regret personally going to re-assess a patient. You may regret not going to re-assess a patient. Chastain comment: When you are on an off-service, don’t forget you are an ER doc. Think globally about your patients. Harwood comment: Is there a bright line to decide which trauma patients would benefit from therapeutic hypothermia? Nick, if it is a non-traumatic arrest with no active bleeding and no brain bleed then therapeutic hypothermia is indicated.
Girzadas Neuro Study Guide
I was giving the lecture so couldn't take the notes.
Gore Safety Lecture
Case 1 40 yo Pt presented with multiple physical complaints related to severe hypothyroidism.
Case 2 35yo female presented with headache similar to previous migraines.
Kasia ordered migraine cocktail accidentally on patient 1. She did not switch out of the electronic record of patient 1 prior to ordering what she intended for patient 2.
Safety strategies: Limiting distraction, EMR blocks to ordering on the wrong patient, Doing time outs prior to placing orders. Easiest to rapidly implement: Do a mental checklist or “safety check” while waiting for orders tab to load. Check patient, allergies, and intended orders.
Multiple persons commented that they have made this same mistake. Multiple people asked that chief complaint be added to the top bar. Robbie suggested that you can place orders while you are in the patient’s note. It keeps you from accidentally placing orders into the wrong chart.
Collander Meningitis/Encephalitis
Bacterial Meningitis: Strep pneumo 61%, Neiseria 16%, others are less common.
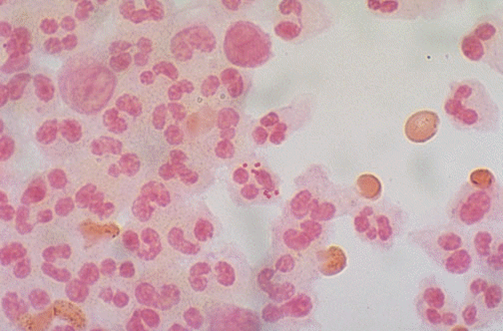
Gram negative intracellular diplococci N. Meningitidis
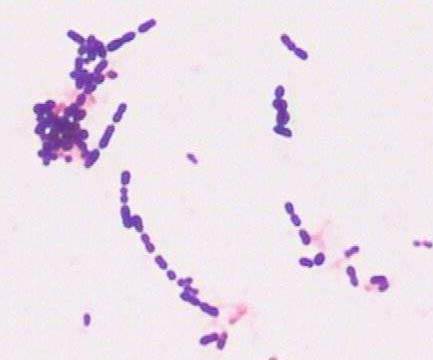
Gram positive rods in chains Strep pneumo
Just a reminder for Boards what the gram stain colors are in case they give you a slide on the test
Purple= positive Red=negative
Predisposing factors: otitis media, immunosupression, etohism, dm, endocarditis, extremes of age, liver disease, many more.
Brudzinski: Neck flexion by examiner causes pt to flex hip and knees
Kernig’s sign: With patient’s hip flexed, examiner cannot extend knee fully due to pain in posterior leg.
Criteria for doing a CT prior to LP: altered mental status, focal neuro deficit, papilledema, seizure within the last week, immunocompromised state, history of CNS disease, age over 60, malignancy, concern for a CNS mass lesion. If patient has none of these, you an do an LP without a prior CT.
Steroids: Give before or at the time of first antibiotics. Reduces morbidity in H flu and S Pneum inkids. 50% reduction of M & M in adults with S. Pneumo. Equivocal results in adults with N. Meningitidis. Dose is 0.15mg/kg Q 6 hours or 10mg Q6 hours for adults. Lovell: Reason to not start steroids after antibiotics is that it doesn’t work. Harwood comment: The reason steroids don’t work after antibiotics is that the bacteria have already started to be killed and the steroids are less effective in halting the inflammatory cascade at that point . I give steroids if I have a strong suspicion of meningitis or abnormal csf on visual inspection. Elise comment: Steroid work best for strep pneumo but because you won’t know the gram stain or culture results at the time of first antibiotics, base your decision to give steroids on visual inspection of csf during tap.
Normal opening pressure is <170 mm of H2O. Bacterial meningitis is usually >300 mm of H2O. Viral between 170 and 300 mm of H2O. Girzadas comment: As a practical point the manometer in our LP kits measures the column of CSF in centimeters. So 17 cm =170mm of H2O, and 30cm=300mm of H2O.
Antibiotics:
0-1 month Ampicillin and Cefotaxime, or Ampicillin and Gentamycin
1-3 months Amp and Ceftriaxine
3mo-50 year Cetriaxone and Vanco
>50yr Ceftiraxone, Vanco, and Ampicillin
Chemoprophylaxis: Rifampin 600mg Q12 for 4 doses. Single 500mg Cipro dose is another option. Single dose of IM ceftriaxone is another option.
Viral meningitis: If CSF study not clearly bacterial or viral, cover with antibiotics and do CSF viral studies. CMV,EBV,VZV,HSV are in the standard panel. West nile is a separate IGM study. If you have suspicion for HSV give acyclovir 10mg/kg in the ED.
*Great teaching point*Andrea comment: Most common drug induced cause of aseptic meningitis is NSAID’s. Ibuprofen is the most common. NSAID induced aseptic meningitis can look exactly like viral meningitis. It is an idiosyncratic reaction to an NSAID.
