Kmetuk/Katiyar Oral Boards
Case1. 8yo male very uncomfortable on cart due to pain. On exam patient has tender abdomen with palpable muscle spasms. Patient also has priapism and painful muscle spasms of extremities. Evidence of a spider bite was also noted on the patient’s skin. Further history from grandmom brings out the fact that the child was playing in the woodshed prior to the onset of pain. Diagnosis was black widow spider bite. Patient was treated with narcotic pain medication and black widow spider antivenin. Also benzodiazepines are effective for muscle cramping. Patients should also receive local wound care and tetanus prophylaxis. Intravenous calcium is no longer recommended.
*Black widow spider
*Black widow spider bite
Teaching point is that BW spider bite victims will present more commonly with muscle cramps than with a complaint of a spider bite. Abdominal muscle cramps are the classic presentation. You can also get vital sign abnormalities and uncommonly priapism.
Case 2. Elderly woman was found unresponsive in her bed. Her apartment was noted to be very hot. Patient’s temperature was 40.5 C. CPK was very elevated. Diagnosis was environmental heat stroke with associated rhabdomyolysis. Critical action was to rapidly cool the patient. Also, hydration was indicated to treat rhabdomyolysis. The emergency physician should also rule out sepsis and toxins as the cause of altered mental status and fever. Rapid evaporative cooling can be achieved by spraying room temperature water on a disrobed patient and directing fans on patient. If you have a therapeutic hypothermia device such as the arctic sun device that is another effective means of rapidly cooling the patient.
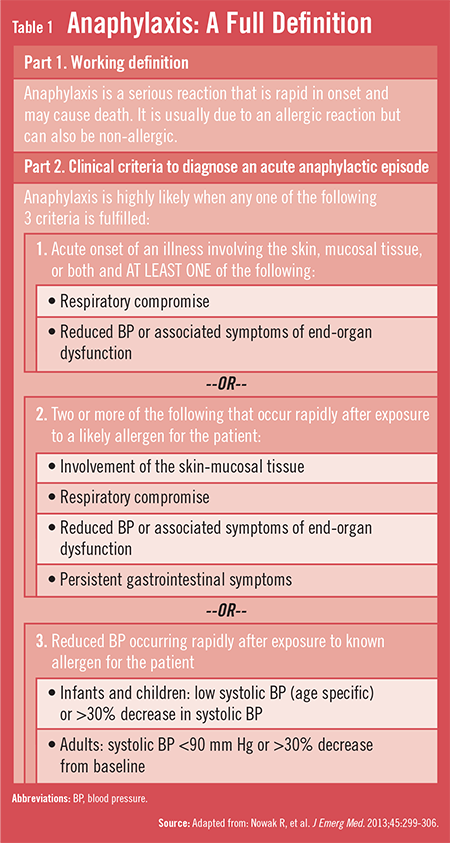
Case 3. 32 yo male with respiratory distress and rash after being stung by bees. Patient was diagnosed with anaphylaxis and was resuscitated with epinephrine, diphenhydramine, steroids and cricothyrotomy.
*Anaphylaxis criteria
Harwood comments: The arctic sun device was very effecting in cooling a hyperthermic patient we managed last week. Tylenol will not be effective in lowering the temperature in a hyperthermic patient. You will have to initiate active cooling measures like cooling device or evaporative cooling.
Burt Safety Lecture
Current clinical practice managing critically ill patients in the ED is not optimal. If patients have a delay of 6 hours to get an ICU bed it increases hospital length of stay and increases suboptimal outcomes.
EICU (critical care telemedicine) has been shown to improve mortality, decrease ICU complications, and shorten ICU length of stay.
We are going to trial a new process of caring for ICU boarders in the ED. These patients will have increased nurse staffing to the level of a typical ICU (2:1 nurse to patient ratio). ED physicians and EICU intensivists will be following the patients. Orders will be entered into Allegra and mesh with the in-hospital system while the patient is still in the ED. Communication will be improved/increased between the ED/ICU/EICU. There will be a 5 way phone call between the ED physician/ED nurse, ICU physician/ICU nurse, and EICU physician.
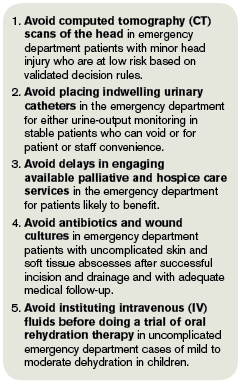
Febbo Society Recommendations for EM
*Choosing wisely campaign for EM
Oral Rehydration is preferred over IV Fluids in vomiting children.
Give the child 5 ml orally every 2 minutes. Pedialyte is the optimal solution. Goal is 100ml/kg over 4 hours. Can pretreat with Zofran if the child is vomiting. Vomiting is not a contraindication to oral rehydration.
Elise comment: If you are trying to rehydrate a pediatric patient you have to give them more than a popsicle.
Cirrone comment: Dr. Sawlani said the top diagnoses missed when managing vomiting kids was pyelonephritis, lower lobe pneumonia and brain tumor. So keep those in mind when caring for a child with vomiting and dehydration.
Avoid CT head in patients with syncope. They are unlikely to provide useful information for patients with syncope.
Avoid CT Chest for PE in patients with negative PERC rule and in those with a negative D-Dimer and Wells score less than 4. The risk in these patients is low enough that radiation risk exceeds the diagnostic yield. Harwood comment: You will miss some PE’s with this approach but it still is the right way to go.
Avoid lumbar spine imaging in atraumatic low back pain unless you have suspicion for serious underlying process.
Avoid antibiotics for treating sinusitis. Consider decongestants and nasal steroids. If you give antibiotics Augmentin should be your first line. Doxycycline and flouroquinolones are alternatives. Harwood comment: I recommend treatment with antbiotics for patients who have been ill for more than a week. In the first week of a sinusitis-type illness, I agree that antibiotics are not helpful
Avoid CT abdomen/pelvis for patients under age 50yo with history of renal colic and a presentation consistent with prior stone. You can use ultrasound in these patients to identify hydronephrosis. You need to also check a urine for infection. Probably should also check a creatinine.
Carefully consider obtaining a urine culture in older patients because there is a 50% rate of asymptomatic bactiuria. Don’t get a UA/culture unless they have symptoms suggesting a UTI. Make sure you are considering other causes of the patient’s symptoms and you aren’t just latching on to a false positive UA result.
Don’t rely on antihistamines to treat severe allergic reactions. You have to give epinephrine. Girzadas comment: I sometimes see hesitancy to give epinephrine. If the patient has criteria (see chart above) for anaphylaxis, give epinepherine subQ. After that you can give Benadryl, H2 blockers, and steroids.
Topical antibiotics are not indicated for surgical wounds. Harwwood comment: This really means don’t use neomycin on wounds. There is a high rate of contact dermatitis due to neomycin. When patients apply neomycin or triple antibiotic containing neomycin they get an erythematous skin reaction. This reaction is bothersome to the patient and can look like a wound infection.
Consider not prescribing antibiotics for otitis media in kids between 2-12 years old if they don’t have severe pain and don’t have high fever (>39C)
American Academy of Ophthalmology recommends no antibiotics for adenoviral conjunctivitis. All faculty agreed that this is a tough sell to parents and schools. Harwood comment: Not treating with antibiotics and having patient follow up with ophthalmology is probably a much more expensive and inconvenient option than just giving topical antibiotic.
No need to give FFP or Platelets to patients prior to paracentesis.
Avoid NSAID’s in patients with HTN, CHF, or CKD of any cause.
Carlson Antidiabetic and Hypoglycemic Agents
Consider hypoglycemia in every patient with altered mental status and/or any focal neurologic finding. Andrea discussed a patient who presented altered mental status and tonic eye deviation. The presumptive diagnosis was intracranial hemorrhage and the patient went to CT. The CT was normal but the glucose was 18. All faculty agreed the hypoglycemia will fool you.
If you suspect intentional insulin overdose: Examine skin for boggy and/or hemorrhagic area. High doses of subQ insulin will have a significant skin reaction. Check Insulin C Peptide level. Exogenous snsulin overdoses have high insulin levels and have low C-peptide levels. Endogenous insulin contains c-peptide. Exogenous insulin does not have c-peptide.
Intentional insulin overdose: 23 hour OBS if the patient is hypoglycemic at any point.
Sulfonylureas stimulate endogenous insulin release. C-peptide levels will be elevated because it is stimulating endogenous insulin release. A single tablet can make a pediatric patient hypoglycemic. Basic management recommendations for sulfonylurea overdoses: 23 hour observation, IV octreotide for recurrent hypoglycemia, IV dextrose for hypoglycemia but no prophylactic IV dextrose in the normoglycemic patient, early feeding, regular accuchecks, and observation of mental status. Meglitinide overdoses are managed similarly to sulfonylureas.
If patients need D25 infusions to maintain normal blood sugar, you will need to place a central line.
Octreotide is indicated for sulfonylurea overdoses if the patient drops their sugar a second time after initial dextrose therapy. Andrea said you could make a case to give octreotide after the first episode of hypoglycemia but she felt most toxicologists would wait for a second episode of hypoglycemia. With have fewer episodes of hypoglycemia and lower glucose requirements. It is given subQ or slow IV infusion.
Metformin inhibits gluconeogenesis and enhances peripheral glucose uptake. Hypoglycemia is rare with metformin overdose. Overdose with metformin can result in lactic acidosis (MALA). Metformin in high doses is a cellular poison and disrupts aerobic metabolism. In high doses it acts as a weak cyanide-like substance. If a patient develops lactic acidosis, dialysis is indicated.
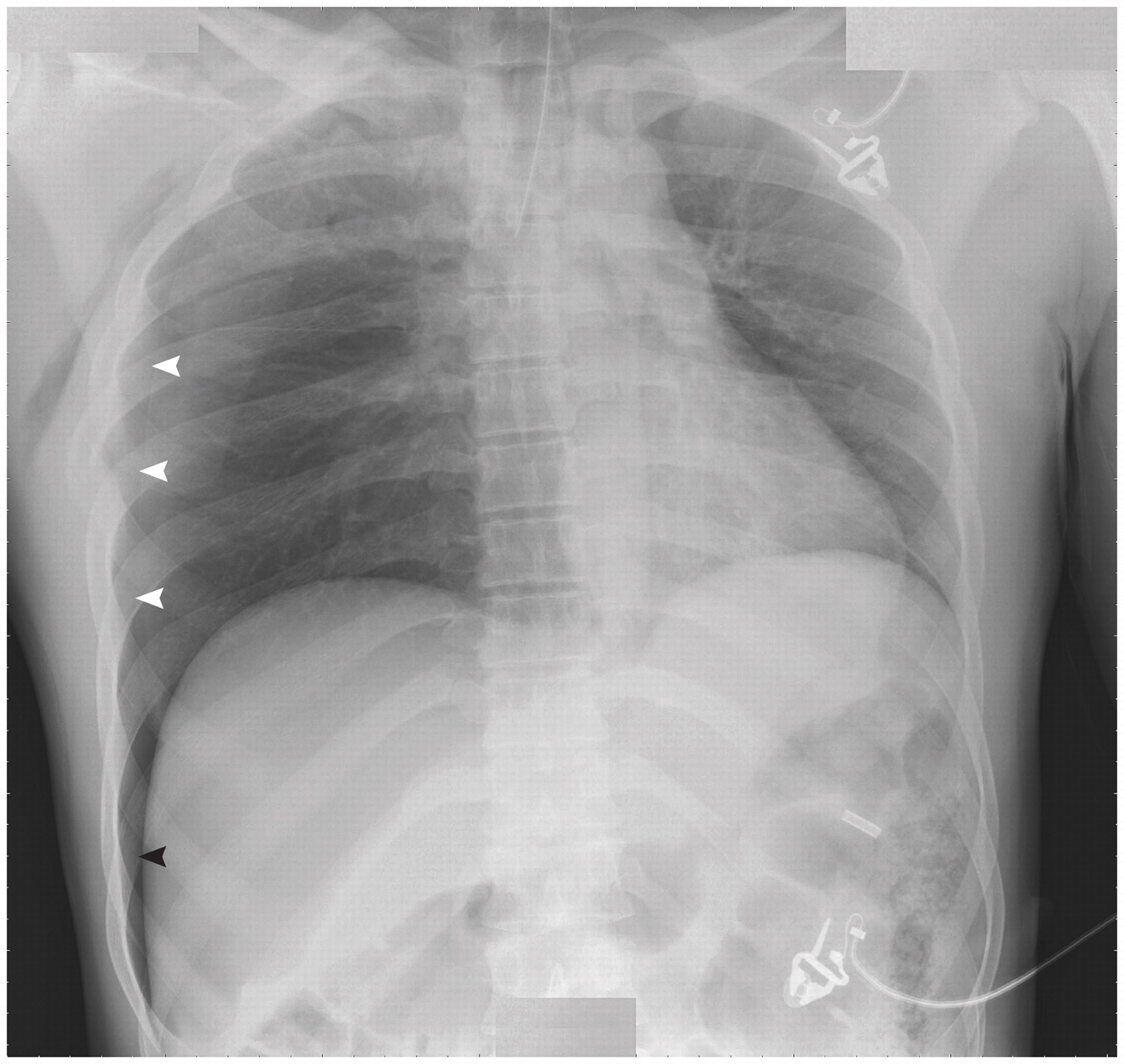
Permar Intro to Reading Chest Xrays
CXR Interpretation Mnemonic: Drs. ABCD
D= Data of patient (name, age, MR#)
R= Rotation/inspiration/exposure
S= Soft tissues and bones
A= Air, airway
B= Breathing (lung)
C= Circulation (cardiomediastinum)
D= Diaphragm
E= Extras (central line, NG tubes, ET tube, pacer, etc)
Trale took us through multiple chest xray examples.
*Deep sulcus sign for Pneumothorax
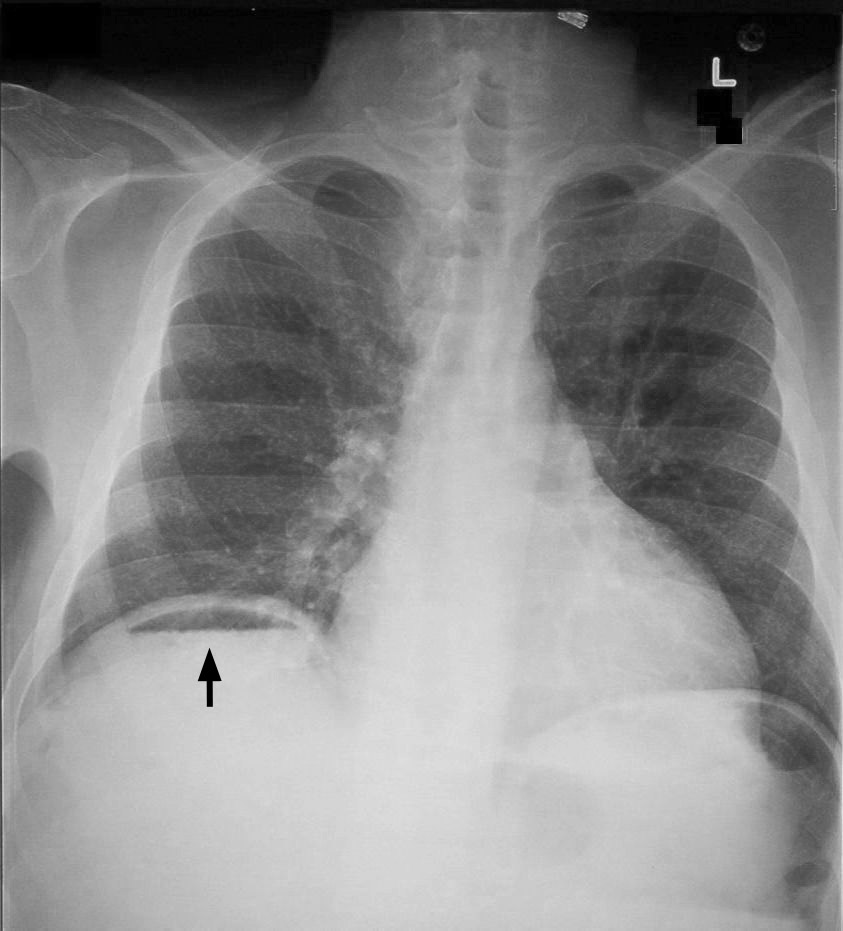
*Free air under the diaphragm
Beckemeyer Patient Satisfaction
On the interview trail Jen has found that employers are asking if our program has formal patient satisfaction training. Understanding of patient satisfaction principles is a big interest of employers.
Press Ganey surveys query patients about the physician: Friendliness, explanation of the diagnosis, shared decision making, clear instructions, clarity of medication information, amount of time the caregiver spent with you, the physician’s attention to the patient’s comfort, and the patient’s confidence in the provider.
Elise comment: Everything on this survey is about communication. It is not about how smart you are or whether you made the correct diagnosis. All of us can employ communication strategies to do better on the survey.
Easy things: Patient privacy, food, water, work note, school note, and clean environment.
If you have to take a phone call during your H&P, apologize to the patient for the interruption, tell them the call will be brief and step out of the room to take the call.
Treat pain early and aggressively.
Body language: It is best that the physician sits. If you must stand, avoid crossing your arms as that seems to indicate you are closed off or hostile. Make eye contact. Introduce yourself to everyone in the room. Avoid interrupting the patient when they are speaking . Check on the patient frequently.
Elise comment: If patients are using medical terms, ask them if they are in the medical profession. If they are, their knowledge helps you a lot. Be sure to smile. Smiling is a simple strategy that is extremely effective.
Kelly comment: If you are the second doc to see the patient in the ED, try to preface your conversation with the patient that you spoke with the first doctor and you just want to go over the key points of the history. You want to have the patient understand that you and the other physician discussed their case and management. You don’t want the patient to feel they are starting from scratch all over again with another doc.
Demonstrate empathy. Try to find out what patients are most concerned about.
Navarette comment: Apologize to the patient for their wait and thank them for waiting. Harwood comment: Apologizing to patients for their wait time or any other issue that has impacted their visit is a very effective strategy.
Give the patient a plan. Let them know what you are thinking and what the expected course of the ED visit will be. This really helps the patient understand what is going on while they are in the ED.
Conclude the visit with discharge instructions and thank them. Make sure they know all the testing and critical thinking that you did for them at this visit. You want them to understand that you put in a lot of attention and thought to their care.
Christine comment: Doing these things make your patients happier and in turn make you happier and make the shift better. There is a definite payoff to the physician for paying attention to patient satisfaction.
Harwood comment: It is ok to negotiate with patients about what tests they want and how long they are willing to wait for a specific test. It gets back to shared decision making.