Lovell Pulmonary Study Guide
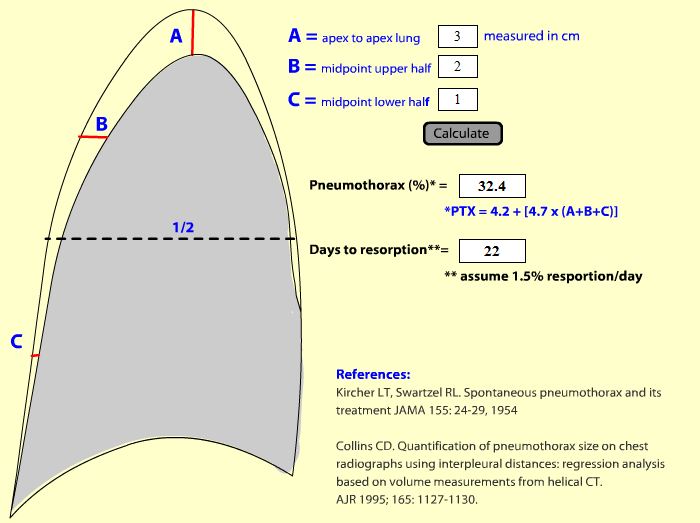
Placing a mini chest tube is the best answer for treating a large primary spontaneous pneumothorax. Small spontaneous pneumo’s (measured as 3cm or less from apex of the thorax to edge of lung) can be treated with observation and oxygen and re-xray at 6 hours. Oxygen helps a pneumothorax resolve more quickly. If pneumo is not increasing at 6 hours, pt can go home. Pneumo’s may take 2-3 weeks to resolve on their own.
Pneumothorax Calculator on chestx-ray.com
Pneumo’s in COPDr’s are different than primary spontaneous pneumo’s and probably should get a chest tube in the low 20’s French size. Trauma patients with pneumothorax should get a standard larger chest tube.
Gotta differentiate between blebs and pneumo's in COPDr's. Below are Blebs/bullae in a COPD patient


Blebs in COPDr’s can be easily confused for a pneumothorax. If in doubt, get a CT to clarify the diagnosis.
The definition of massive hemoptysis is >600ml over 24 hours. For quick estimation of hemoptysis volume in the ED: mild hemoptysis is blood streaked sputum, moderate hemoptysis is clots/fress blood, massive hemoptysis interferes with oxygenation. Remember that TB can be a cause of massive hemoptysis and wear personal protective gear when at the bedside of a patient with massive hemoptysis.
Tracheo-Innominte Artery Fistula: Happens within several days to 4 weeks of tracheostomy placement. Patient can have a relatively minor appearing sentinel bleed. But the next bleed is going to be catastrophic. Get a CT chest/neck and a bronchoscopy in the ED for sentinel bleed. If the patient is having massive bleeding, over-inflate the trach balloon. If that fails to stop the bleeding, intubate patient from above, remove the tracheostomy tube simultaneously and stick your finger into the tracheostomy site anterior to the trachea and use your finger to compress against the sternum. Teaching point: Recent tracheostomy and bleeding from tracheostomy site consider Tracheo-Innominate Artery Fistula.
Harwood comment: in NH patients with bleeding from trach site, if you see an obvious source from the skin then probably no danger. If you don’t see an obvious soft tissue source of blood, then you gotta CT and get a Bronchoscopy .
Tracheo-Innominate Artery Fistula Rescue Maneuver
Risk factors for lung cancer in a patient with hemoptysis: male, age >40, smoker, recurrent hemoptysis, and no bronchitis/infectious symptoms.
Most common bacterial cause of pneumonia in HIV patients: Strep Pneumo.
Also think about TB in HIV patients even if their CD4 counts are OK. Think about pneumocystis pneumonia in HIV patients with pneumothorax.

Pneumocystis pneumonia and Pneumothorax
Pneumonia symptom complexes: Sudden onset, rust color sputum, rigors think strep pneumo. Post influenza think staph. Alcoholic think Klebsiella. Joint pain, bullae on TM, rash, sore throat think mycoplasma.
Aspiration pneumonia: Don’t use steroids. You need anaerobic coverage in addition to usual CAP coverage. Add clindamycin to usual CAP coverage. Moxifloxin is a second line option that can be used as single agen. For HAP with suspected aspiration, the Zosyn in our standard HAP regimen will adequately cover anaerobes.
IGRA blood test can be used in place of PPD to identify TB exposure. The result comes back within 24 hours. It is thought to have similar sensitivity and specificity to a PPD test. Consider for use in admitted patients to help identify more rapidly who needs to stay in isolation. Could also this test use in outpatients to avoid need to re-evaluate pt’s PPD site.
Primary TB infection is usually asymptomatic. Latent stage has positive PPD. 5% risk of progressing from latent stage to active TB in 2 years in immunocompetent patients. 5% chance of converting from latent to active TB during patient’s lifetime in immunocompetent patients. A patient is contagious only during active stage of TB.
Scrophula=painless lymphadenitis due to TB or other mycobacterium. In adults it is most commonly due to TB. In kids it is most commonly due to other non-TB mycobacterium

Scrofula
Negro/Doherty Trauma Lecture
60 yo male was pinned between a car and a brick wall. Pt arrived to ED with tachycardia and cool extremities (clinically in shock despite BP being still over 100systolic). Pt had open pelvic wounds including rectal wound that were bleeding. It turns out that patient was on Plavix to make matters worse.
Pelvic Xrays showed very wide diastasis of pubic symphisis
Only check the pelvis for instability once. Don’t repeat pelvic instability exam if you think the pelvis is unstable. Moving the boney fragments can increase bleeding.
Pelvic binders are still recommended by ATLS but there is no animal study data to support pelvic binding. Consensus by Trauma and EM at this conference was that pelvic binding was still helpful. Pelvic binding should be wrapped around the greater trochanters not the iliac crests. Binding will not have an effect on arterial bleeding. It is intended to tamponade venous bleeding. External pelvic fixation has no benefit over pelvic binding. Patients with hemodynamic instability from a pelvic fracture despite pelvic binding should go to IR for embolization.
Patient continue to receive IV fluids and O negative blood. Patient had an open rectal wound from sharp boney edge which was packed.
Patient became agitated and was intubated. Have to be careful about hemodynamic collapse in this type of patient when giving induction drugs. Give conservative doses of induction agents. Choose the most hemodynamically neutral induction agents and be prepared to give push dose of pressors for hemodynamic collapse.
Massive transfusion protocol was initiated.
Tranexamic Acid inhibits fibrinolysis by blocking lysine binding sites on plasminogen. CRASH-2 trial showed a decrease in mortality from all causes (14.5% vs. 16%). TXA was given.

TXA competitively inhibits fibrinolysis
Next decision is whether to go to OR or IR.
Doherty comment: This decision is more complicated than the algorithms make it seem. The right answer for boards is go to IR. However, if there is a delay to get IR mobilized, there are arguments to take a very unstable patient to the OR. The goal of management for both IR and OR is to occlude the internal iliac artery on the side of fracture.
FAST scan can help with this decision. If you can get patient to IR rapidly and there is no intra-peritoneal blood on FAST then patient should go to IR. If FAST shows intra-peritoneal blood the patient should go to OR. Doherty comment: This situation is one of the most critical indications for FAST scanning. It’s a binary test: If blood on FAST go to OR. If no blood on FAST, go to IR. Prior to FAST, old school approach was an open supra-umbilical DPL to identify intra-peritoneal blood.
Doherty comment: If patient’s BP bumps up during IR procedure it is a sign of successful embolization of the internal iliac or branch vessel.
Beckemeyer/Katiyar Oral Boards
Case 1. Young boy presents with vomiting and passed out. Family members from Viet Nam were visiting. One family member was taking medication for “lung problem”. Patient began seizing in ED. Diagnosis was INH poisoning. Critical actions were to manage seizures initially with lorazepam and to give pyridoxine as an antidote to INH induced seizures.
Case 2. 14 yo female passed out twice at school. Pt had palpitations at gym class and passed out . EKG shows long QT interval. Patient arrests in ED. Monitor shows torsades. Critical actions: Defibrillate and give IV magnesium. Could also overdrive pace to shorten QT interval.
Case 3. 42 y/o female with worsening headaches, 4 weeks post-partum. Has seizure in ED, treated with magnesium. Diagnosed with eclampsia. Critical actions- CT/MRI, control BP, magnesium.
Knight Hemoptysis
Unfortunately, I missed the majority of this excellent lecture.
Brisk hemoptysis is more deadly than exsanguination.
Herrmann comment: When attempting to intubate the hemoptysis patient, suction the airway and place the yankaur suction catheter through the cords and then pass a bougie right next to the yankaur through the cords. You can then pass an ET tube over the bougie
Hemming CHF and Pulmonary Edema
2 most Common causes of readmission for CHF: diet, medication non compliance.
Best history components for diagnosing CHF: CHF, MI, CAD
Best symptom components for diagnosing CHF: PND, Orthopnea, Edema
Best PE components for diagnosing CHF: S3, HJR, JVD
High level discussion between Elise, Erik, Christine, and Harwood about the utility of LR’s on the above items. There was no clear consensus to report.
Sonographic B lines correlate well with Curley B lines and Lung water scores. It can reliably diagnose CHF. 3 or more comet tails is suggestive of wet lungs. Girzadas comment: U/S is very reliable for diagnosis CHF.
BNP can diagnose and prognosticate CHF. Other causes of elevated bnp: age, renal failure, ACS, chronic lung disease, large PE, high output cardiac state.
Treatment of CHF: NTG is first line. IV furosemide is second line but efficacy is unclear . Ace inhibitor is third line; some caution because it can cause hypotension. Morphine is ineffective and may result in respiratory depression and worsened outcome. Morphine may be indicated in diastolic dysfunction with elevated BP. O2 and Bipap/Intubation should be used as indicated. Balloon pump should be used for mechanical cardiac complications (wall rupture, valve dysfunction, papillary muscle rupture) causing CHF . Inotropes are not usually indicated for CHF management due to increased mortality.
Discussion of Furosemide in CHF: Erik’s comment was to take the middle road, give IV NTG and give small dose of IV Furosemide. Harwood comment: Give high dose IV NTG initially, titrate back to lower dose after first hour or two and also give conservative dose of IV Furosemide. Febbo comment: Research showed no difference between high dose IV Furosemide or an IV dose of Furosemide consistent with patient’s usual oral dose.
Harwood comment: If you have to intubate a CHF patient you are a failure as an ER doc. A good ER doc should be able to pull the vast majority of CHF patients back from the edge using Bipap and NTG and Furosemide. Andrea comment: There may be the rare patient you have to intubate and you shouldn’t feel bad about that. The faculty agreed that in the hypotensive CHF patient they have cardiogenic shock and these patients should be intubated and given an inotrope and should have emergent cardiology consultation .
Burt Patient Follow-Up
55yo female with abdominal pain. Hx of cholithiasis and HTN. No previous surgery. Exam showed RUQ tenderness. Initial work up focused on possible cholecystitis. Pt later told examiner that she had been “walking funny”. Repeat exam showed abnormal gait. Labs all normal. U/S of gb shows gall stones but no wall thickening. MRI of spine showed epidural spinal cord compression from tumor. Breast, prostate, lung, multiple myeloma, lymphoma, sarcoma, renal cell, melanoma are potential primary neoplasms that can cause epidural cord compression. Epidural neoplasm or abscess are very difficult diagnoses and are frequently missed on the initial ED visit.

Arrows point to lymphoma causing epidural compression
Htet Patient Follow-Up
60 yo male with altered mental status. Patient had unusual headache for week prior. Hx of HTN, CKD, cardiac aneurysm s/p repair on Coumadin. In ED atient was intubated and INR was 3.5. CT showed SAH with trans-tentorial herniation.

Colored arrows point to subarachnoid blood. Black and white arrows point to normal calcifications
Pt was given FEIBA in the ED. Neurosurgery placed ventriculostomy in ED. Dilantin was given. IV versed given for sedation. Patient was having seizures every 3 minutes in ED. IV Ativan was ineffective for stopping seizures. Second dose of Dilantin given. Keppra 500mg IV also not effective (could have given 1000mg). IV phenobarbital 20mg/kg was given and worked. Phenobarbital binds to GABA receptors. It reduces cerebral blood flow and reduces cerebral metabolic activity. Down side is patients can have @100 hours of sedation and also have hypotension.
Class 2B recommendation: Prophylactic anticonvulsants can be given in the immediate post-SAH period.
Status epilepticus: Class 1 recommendation=lorazepam and midazolam. Class 2 recommendations: Keppra, phenobarbital, phenytoin, propofol, and valproate.
Harwood comment: For a patient in status epilepticus start with aggressive benzo’s and then just start trying any other anti-epileptic. When you combine benzo’s and phenobarb, you will have to be prepared to intubate that patient if they become apneic.
Erik comment: In patients with refractory seizures who are getting hyperthermic, consider starting therapeutic hypothermia.