Farewell to the Class of 2014! You are an awesome class and we are going to miss you! (See pic below)
No conference notes for the next two weeks: Pig Lab next week and Intern Orientation starts the following week. We'll pick back up with conference on July 2nd.
Kmetuk/Bolton Oral Boards
Case 1. Infant presents with Jaundice. Total bili is 22 with indirect bili predominating. Diagnosis was breast feeding jaundice. Critical actions: Get rectal temp, order CBC/coombs/smear/fractionated bilirubin, administer IV fluids, initiate phototherapy. Most common jaundice is physiologic. Always be alert for sepsis causing jaundice in an infant(Look for fever, poor feeding, not well appearing). Infants can also have breast feeding or breast milk jaundice. Elise comment: I don’t routinely get a coombs test on jaundiced infants, unless there are signs of hemolysis on the CBC or the patient appears ill. Harwood comment: you gotta plot out the bilirubin level on the time graph.
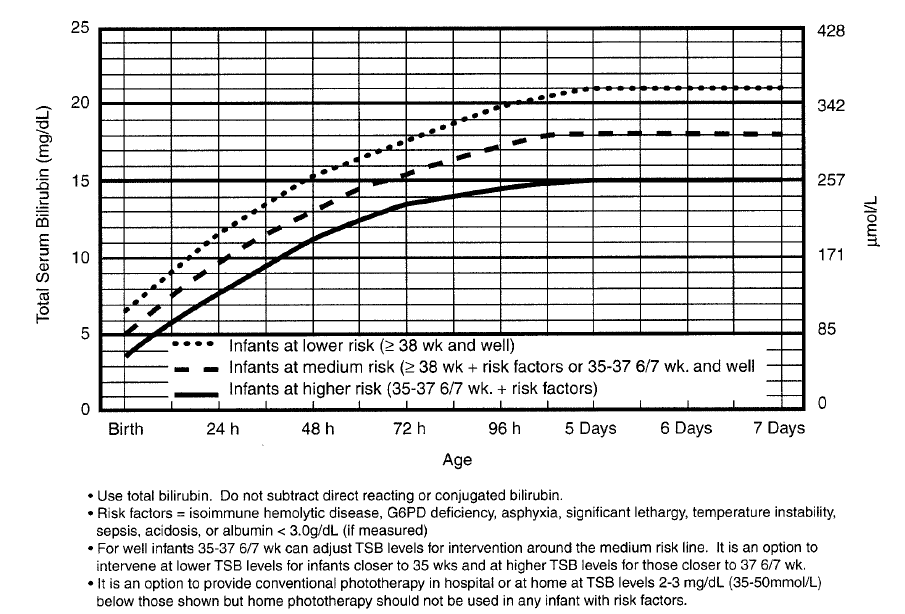
*Bilirubin/Time Chart for Phototherapy
Case 2. Patient presents with pulseless/painful leg. Pt was also found to have afib. Critical actions: Give pain medication, start IV heparin, consult vascular surgery. If you get an ABI to evaluate arterial flow in a limb, any measurement less than 0.9 is a concern. Less than 0.5 mandates urgent vascular consult. Girzadas comment: If you identify a pulseless extremity, think Afib, dissection, and endocarditis in addition to severe atherosclerosis. Harwwod comment: You have to check every pulse in the affected extremity to try to identify where the clot is.
Case 3. 18yo male with SOB. Patient was found to be cyanotic. Methemoglobin level was elevated to 55%. Pulse ox was 85%. Further history identified that the patient was using “poppers” Critical actions: Intubation, get ABG with co-ox/metHgb, administer IV methylene blue (1-2mg/kg). MetHGB can be measured on VBG. Patients with G6PD don’t respond to methylene blue. Poppers are amyl nitrate inhalers and are used for getting high and for sphincter relaxation. Girzadas comment: Andrea and Ted always make the point that if you see a pulse ox of 85% you gotta think methemoglobinemia. Andrea comment: Methemoglobin produces a light wavelength that gives you a pulse ox of 85%. Andrea comment: Don’t give narcan to an intubated patient. It’s just poor form. You have the airway managed so narcan will do nothing for the patient except possibly agitate them.
Elise comment: Check pupils and skin to identify a toxidrome in any tox case on oral boards.
Hemming Penetrating Neck Injuries
Zone 1 of the neck: Includes lungs, aorta, subclavian vessels, vertebral arteries, esophagus
Zone 2: cricoid to angle of mandible: Largest/Most commonly injured area
Zone 3: Angle of the mandible to base of the skull. Difficult surgical access.
Girzadas comment: To remember if zone 3 is at the top or the bottom, think 3rd ventricle. There is not 3 of anything in the chest . Humerous Elise comment: There are 4 ventricles though! Maletich comment: I think of an elevator going up to the third floor.
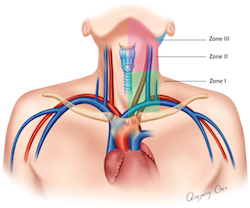
* Zones of neck with structures in each zone
Hard signs of significant neck injury: active external bleeding, bruit or thrill, expanding/pulsatile hematoma, oropharyngeal bleeding, sucking neck wound, neuro deficit. subQ air, blood in oropharynx, stridor.
Traditional approach: If there is physical sign of penetrating injury to neck:
zones 1&3 if the patient is stable, should get CT angiography/endoscopy/
bronchoscopy.
zone 2 should go to OR for exploration (stable or unstable).
There is a “no zone” approach: If penetration of any zone and stable, then patient gets a CT angio +/_ esophogoscopy/bronchoscopy. If significant injury found then patients goes to OR . Unstable patients go to OR without imagng.
Flexible endoscopy has very high sensitivity for esophageal injuries. CT can miss some esophageal injuries.
1/3 of vertebral artery injuries are asymptomatic. Most do not have neurologic sequelae.
Zone 2 injuries with physical findings require exploration.
RSI is considered safe
Physical exam is a powerful tool to identify significant neck injuries.
Elise comment: Is trauma taking all Zone 2 injuries to OR? Hemming response: If patient has no hard signs of injury and a non-threatening bullet trajectory, they will do CT/endoscopy.
Harwood comment: If I was working in a non-level 1 hospital and was confronted with a patient who had suffered a penetrating neck injury, my general approach would be to first intubate those who need it . Next, any Zone 2 injury gets trasnferred to the nearest Trauma Center. Zones1 & 3 with low risk signs symptoms can be managed selectively with CT Angio and possibly not get transferred. This raised a lively discussion about who to transfer. The majority of faculty would transfer all penetrating neck injuries and not try to manage any of them at a non-level 1 ED.
Carlson Toxicology Axioms
16 yo female with epigastric pain. There was family conflict preceding this episode of pain. Pt had prior history of cutting and overdose. Labs show hyperglycemia and acidosis. ASA is undetectable. On further lab investigation, Iron level was 800. If you see hyperglycemia and metabolic acidosis think ASA and Iron. Axiom: It’s not tox until you think of tox.
Tox Mimicry: It looks like Food poisoning: could be CO, digoxin, arsenic. You suspect SubArachnoid Hemorhage: think CO. You are considering Meningitis: Think ASA. Ibuprofen overdose can also give meningeal signs. Looks like Sepsis: think cyanide, calcium channel blockers, asa. You are pretty sure it is DKA: consider Iron, AKA, ASA, toxic alcohols, CCB’s, cyanide. Pt has Acute psychosis: consider hallucinogens, sympathomimetics, salicylates, digoxin, anticholinergics, alcohol/sedative withdrawl.
46 yo male with hx of MS and depression. Acutely confused. Family suspects baclofen overdose because they can’t find the baclofen bottle. Pt was febrile and hypertensive. Pt had abdominal pain and diarrhea. This is a classic picture of baclofen withdrawl not baclofen overdose. Pt had placed the plastic jar containing all his baclofen in his rectum for no logical reason. So he did indeed have baclofen withdrawl. All his baclofen was in the plastic bottle that was shoved in his rectum.
Male in respiratory distress after using “cocaine”. Patient clinically has SLUDGE syndrome. Cocaine does not normally cause a SLUDGE toxidrome, it causes a sympathomimetic toxidrome. The Cocaine was cut with malathion (organophosphate insecticide) causing SLUDGE. Axiom: Know your Toxidromes. Opioid, sympathomimetic, sedative-hypnotic, anticholinergic, cholinergic, opioid withdrawl. Kelly comment: we had a case recently of a patient with an opiod appearing toxidrome that turned out to be a pontine hemorrhage. Kind of a reverse tox mimic.
Axiom: Check your Ego at the door. Don’t be shy, call the poison center for help.
3yo male found with open bottle of Tylenol. PMD sent child to ED to get NG tube and activated charcoal. ED doc should always calculate the worse case scenario based on type of medication and the size of pill bottle. Check APAP level at 4 hours. No need for NG and charcoal. If 4 hour level is toxic, start NAC. If it is non-toxic, patient can be discharged. Axiom: Sometimes it is OK to do nothing. It is OK not to decontaminate. Just document that the risks of decontamination outweigh the benefit. Decontamination options are gastric lavage, activated charcoal, and whole bowel irrigation. The senior faculty had a chuckle about how times have changed when a quick survey showed that none of the current residents had ever done a gastric lavage on a patient. Old school faculty reminisced that we all did probably 3 lavages a weekend when we were residents. Definitely the emergency management of toxic ingestions has evolved significantly over the years. All faculty were glad that we don’t have to lavage patients hardly ever anymore.
44yo female who overdosed on INH. Antidote is pyridoxine gram for gram. Axiom: Don’t get caught with your scrubs down. As soon as you start to consider this diagnosis, call the pharmacy to start mobilizing enough pyridoxine. You might need to call other hospitals. Pyridoxine is usually only stocked in limited amounts. Atropine is also under-stocked in the hospital if you have to manage a cholinergic poisoning. Elise comment: In a pinch, you can have a patient with a cholinergic toxidrome drink atropine eye drops which actually has a large amount of bioavailable atropine.
46yo male took 35 tabs of Verapamil SR. Atropine, Ca, glucgon, insulin/glucose all given with no significant improvement. The poison control center found that the emergency physician was under-dosing all the above meds. Axiom:It’s toxicology, not homeopathy. Give the patient enough antidote! Ingestions that need a lot of antidote: CCB’s, Beta blockers, organophosphates, botanical glycosides, flourides, clonidine, sodium channel blockers, INH, gyromitra.
Patient ingested OCP’s and Etoh in a suicide attempt. Pt was deeply comatose. ETOH level was 110. Initial APAP/ASA, ABG is normal. Repeat labs showed anion gap and metabolic acidosis. Toxic alcohols were drawn late and were negative. Pt still was dialyzed and found to have toxic alcohol ingestion. Toxic alcohols were low because they had been metabolized by the time the blood was drawn. Toxic alcohols are more intoxicating gram per gram than ETOH. Axiom: There are toxicologic hidden killers.
Hidden or delayed killers: APAP, Iron, MAO’s, methanol, amanita mushrooms, sustained release drugs, and illicit drug packets.
22yo female possibly took whole bottle of theophylline. Charcoal given. Theophylline level was therapeutic. Pt admitted to psych. 9 hours later pt had seizures due to a theophylline level that was toxic. Axiom: Sometimes you need to get serial drug levels. Serial levels advised for asa valproate (SR), lithium (SR), carbamazepine (SR), CO from methylene choloride, and theophylline.
16 yo male with a seizure at a party. Axiom: Most tox patients will do well with supportive care alone. The top 2 things show to improve mortality are managing the airway and controlling hyperthermia. Other important management items are treating hypotension, correct acid/base disorders, control seizures/agitation.
Negro Safety Lecture The Agitated Patient
50% of physical attacks that occur on healthcare workers happen in the ED.
Our main job is to gain control of the situation, protect staff, and rule out an organic cause for the agitation.
These cases have high physician medico-legal risk and have a high patient morbidity and mortality.
Agitation can be primary or secondary. Primary causes are due to patient’s psychological response to stressors such as police, family, financial stress. Secondary causes are drugs, psychiatric illness, intracranial hemorrhage, sepsis, etc.
Elise comment: Never let an agitated patient get between you and the door. Residents’ comment: Be aware of your safety in the quiet room. Do not let too many people into the quiet room when you have to give the family bad news. Make sure you can get out the door at all times.
Indications for restraint: prevent harm to patient, staff, or other patients.
Physical restraint: This is a team activity. You should have 5 staff members to physically restrain a patient. Never place the patient in prone position. The patient should be supine. Arms should be restrained one up and one down. Left leg restraint should be tied to right of cart and right leg restraint should be tied to left side of cart.
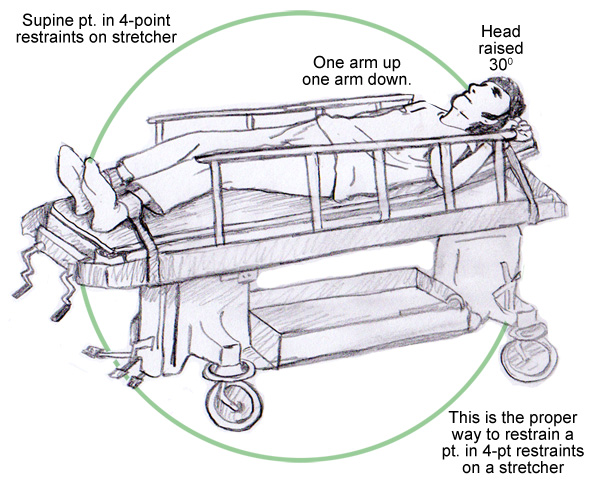
*patient physical restraint. Only quibble with this image is that leg restraint should be tied to opposite side of cart so patient can't kick out.
Chemical restraint: Using a drug to manage a patient’s behavior or limit their movement.
Start with a benzo. Long acting benzo (Ativan) usually preferred. Second drug is an atypical antipsychotic such as IM Geodon. Pharmacist comment: Geodon can prolong QT interval. Elise comment: If I have a suspicion of a risk of long QT, I would stick with higher dose benzos +/_ ketamine 5mg/kg IM or 2 mg/kg IV instead of using antipsychotics.
Typical psychotics that can be used are droperidol or Haldol. These also carry risks of QT prolongation.
Febbo comment: don’t mix zyprexa with benzo’s due to risk of increased respiratory depression.
Weingart suggestion (EMCrit): 5mg droperidol and 5 mg of versed IM.
Agitated or Excited Delerium: pt is completely out of control, pt is psychotic, vitals show tachycardia, tachypnea, htn. Pt has incredible strength. Many deaths have been reported. Taser-related deaths are commonly associated with this disorder. These patients require rapid chemical restraint. They are very dangerous to themselves and others.
Iannitelli comment: Be aware of personal risk when you approach a patient to examine them. Place your hand on the patient’s closest arm so you can push away rapidly if they reach for you.
EM-3 Farewell Lecture

