Follow Up from Last week's Conference Notes
Update from Val Merl (ACMC alumna now at University of New Mexico): Haunta virus is something I actually have seen and treated. If you are thinking about Haunta look at the platelet count. If it is above 200 it isn't Haunta. I don't know if this is from actual published articles but it is what we all do here. There is a specific test for Haunta but it won't become positive for days after the illness has set in. By then the pt is dead or improving. But the most important thing - if you think Haunta you have to admit them where there is an ECHMO team. They need to have the equipment and be standing by in the room. I've had a pt go from being on 2 liters of 02 and watching TV to being on ECHMO with a pressure of nothing in just a few hours. UNM has had good results with putting their pts on ECHMO. And they have probably treated more Haunta pts than anywhere.
Thinking of plague is a good thought but those pts look different than Haunta ( we have that here in NM also) Adults
With plague don't normally look SICK. They normally just have a high fever with no source. They aren't normally hypoxic and their plt count is normally > 200. The way we think of it here is - if it is summertime and the pt looks like they have the flu treat them for the plague (normally they are good enough to do this as out pts) We have had 2 cases already this year.
Editorial Note: Love the feedback from our Alumni. Feel free to send your Teaching Pearls related to conference and I will include them in the notes.
Marynowski Pediatric Study Guide
Unfortunately I missed this excellent lecture.
Carlson Toxic Alcohols (Thank You to Christine Kulstad for writing the notes for this lecture!)
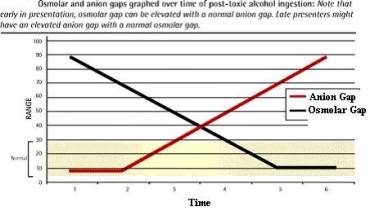
*Osmolar Gap
*Osmolar & Anion Gap Trends
Normal Range of osmolar gap is -14 to +12. This broad range make it an imperfect screening test. However if the gap is out of the normal range, it is specific for toxic alcohols.
Other causes of Osmolar Gap: Mannitol, radiocontrast dye, acetone, propylene glycol
You should be able to get a Stat Ethylene Glycol level from Quest Labs within 3-6 hours. You will need to call the lab to make sure the test gets done as a Stat. Andrea makes it a point to repeatedly call the lab to make sure the specimen is in process and to get the result.
Ethylene glycol, found in antifreeze, deicers, and brake fluid. It tastes sweet, but some have bittering agent and all have fluorescein added.
Ethylene glycol exposure from 1) alcoholics running out of ethanol, 2) improper storage, 3) suicide, 4) poisoning
Absorbed mostly through GI in 1-4 hrs, all other exposures minimal. Low Vd, not protein bound- means HD will remove it. Half life 3 hrs metabolized by alcohol dehydrogenase.
4 clinical phases. Stage 1 is CNS, over 30 min to 12 hrs. Looks like intoxication-somnolence, ataxia, slurred speech. If a massive ingestion- cerebral edema, seizures.
Stage 2- metabolic. Occurs at 4 -36 hrs. Get metabolic acidosis, kussmauls respirations, hypocalcemia, cardiac instability. Most likely to die during this phase. Bicarb drips during this phase can be helpful to counteract the acidosis.
Stage 3- Renal. Occurs at 24-72 hours. Renal tubular necrosis, hematuria, proteinuria.
Stage 4- Neuo, only in significant ingestion. Delayed effects from osmotic demyelination. EG levels > 1000 mg/dL
What to order for ethylene glycol ingestion? BMP, serum ethanol, serum osmolality, stat toxic alcohols, abg, ua, apap, asa, tox screen, EKG.
Who to diagnosis? Ethylene glycol level. Presumptive- pH < 7.3, bicarb <20, osmolar gap >10, urinary oxalate crystals with appropriate clinical context.
Osmolar gap equation= 2(Na) + bun/2.8 + glc/18 + etoh/4.6. Should be less than 20, the normal range is -14 to +12. It may be normal in late ingestions. Other factors that can elevate osmolar gap- acetone (DKA, dehydration), glycerol (mouthwash), propylene glycol (Ativan), mannitol, sorbitol, radiocontrast dye. Roughly osmolar gap x 6.2 = ethylene glycol level.
Gold standard level- GC mass spectrometry. Send STAT to Quest but you must talk to lab as the patient is drawn. Can get results in 3-6 hrs. Do NOT just order it through FirstNet or it will come back in 2 weeks. Watch units as they are not standard for reporting.
Anion gap- Na – (Cl + HCO3). Above 16 is abnormal. In ethylene glycol ingestions- elevated from glycolate and lactate.
ABG machine analyses gylcolate and lactate the same. So lactate may be 25, and serum lactate is 7 for example.
Urine studies less helpful. Calcium oxalate crystals only found in 50% (can also be reported as amorphous crystals). You can fluoresce the urine BUT fluorescein ingestion does not always come out in urine AND kids’ urine naturally fluoresce.
Treatment- can use NG aspiration if early and massive exposure. Activated charcoal doesn’t bind well but can be given for co-ingestion. Improve metabolic profile with bicarb, magnesium, and calcium.
Inhibit metabolism with fomepizole (alcohol if you don’t have ifomepizole). Works by inhibiting alcohol dehydrogenase. Pregnancy category C, but only FDA approved antidote. Give if ethylene glycol level >20 OR suspicion + osmolar gap >10 if early, OR suspicion + 2 presumptive criteria.
Fomepizole dosing- load 15 mg/kg with max of 1 g. then 10 mg/kg q12 hrs x 4 does, then 15 mg/kg q 12 hrs. But interval goes down to q4 hrs while on dialysis. Oral = IV. Earlier administration = better outcome. Adverse effects except headache are rare. It does taste bad.
When can you give fomepizole alone? If treated early and for prolonged period- until ethylene glycol level decreased. Also can use in pediatric patients. Must have pH < 7.3, modest anion gap (<20), no renal dysfunction, adequate fomepizole supply. If ethylene glycol <100, fomepizole alone is well supported.
If you don’t have fomepizole, give ethanol. Can be oral or IV. Its cheap BUT 1) hard to maintain steady level, large volumes needed, kids get hypoglycemic, more CNS depression. Shoot for a level of 100-150, increase rate with dialysis.
Theoretical benefit to adding thiamine 100 mg iv q6h until ethylene glycol gone, pyridoxine 50 mg iv q6h x 24 hours
Methanol- found in more products. It is absorbed more quickly. Absorbed through skin and inhalation.
Methanol metabolized to formaldehyde and formic acid. It causes ocular toxicity and metabolic acidosis.
Clinical toxicity often delayed. Early- CNS depression, seizures, cogwheel rigidity. Ocular- snow field vision, unreactive pupils, APD on presentation is bad. Renal toxicity rare.
Diagnosis it by methanol level, osmolar gap, and anion gap. Can see putamenal hemorrhages on CT which is fairly specific.
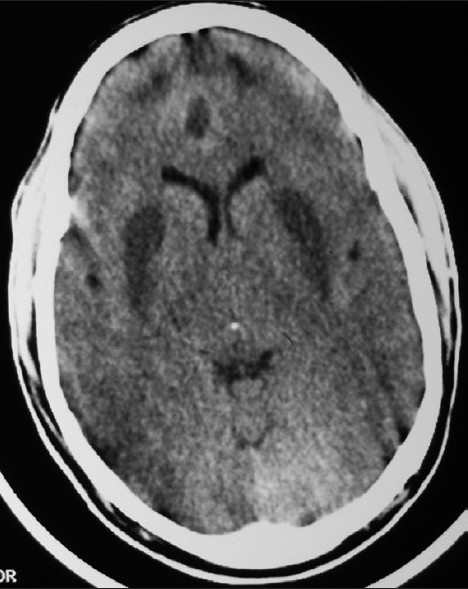
*Methanol CT findings Putamen Hemorrhages (symmetric hypodense NIKE swoosh appearing lesions)
Treat by inhibiting metabolism, leucovorin for folate 50 mg IV q4h (theorectical benefit), dialysis, ophtho benefit.
Can skip hemodialysis if level < 80 and pH < 7.3, modest anion gap (<20), no renal dysfunction, adequate fomepizole supply.
Isopropanol- osmolar gap w/o anion gap. Biggest side effect is GI irritation or bleed. Manage symptomatically. The compound can interfere with creatinine measurement. No fomepizole. HD only if level > 500 mg/dl.
Beckemeyer Stroke Management
Stroke patients have priority over other ED patients in que for CT.
If no blood on CT and pt presents within 3-4.5 hours consider TPA.
In stroke patients do these three things first: check glucose, assess airway, and get a CT head.
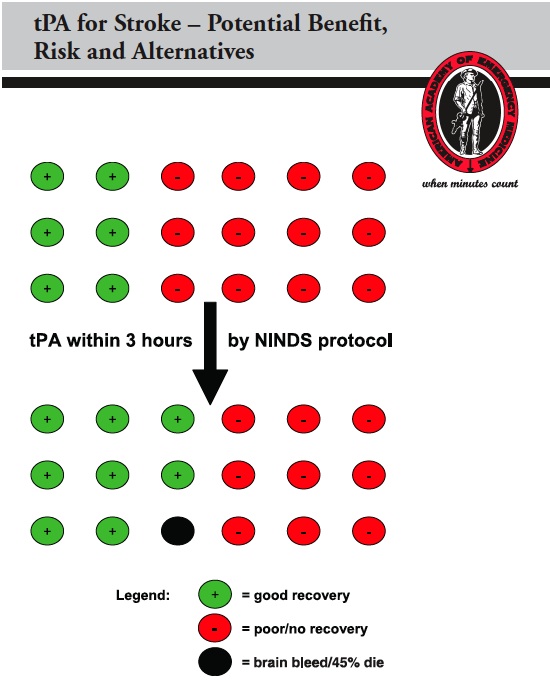
Risk –Benefit of TPA for Stroke :
It is difficult to convey this clearly to patients and their families. According to the NINDS data shown below, about 11 patients in 100 who receive TPA will benefit over receiving only asa. 6 in 100 patients treated with TPA will have intracranial bleeding and about half of the patients with brain bleeds will die.
*Outcomes after TPA
There was a discussion between Erik and Harwood about how to best describe to patients and their families the risks/benefits of TPA.
Keep patients from getting severely hyper/hypo glycemic. Keep them around
140-180. Give IVF. Volume depletion can worsen cerebral blood flow. Have nursing in ED do a simple water swallow test to see if patients can swallow.
Be sure to use the TPA checklist every time to check for contraindications.
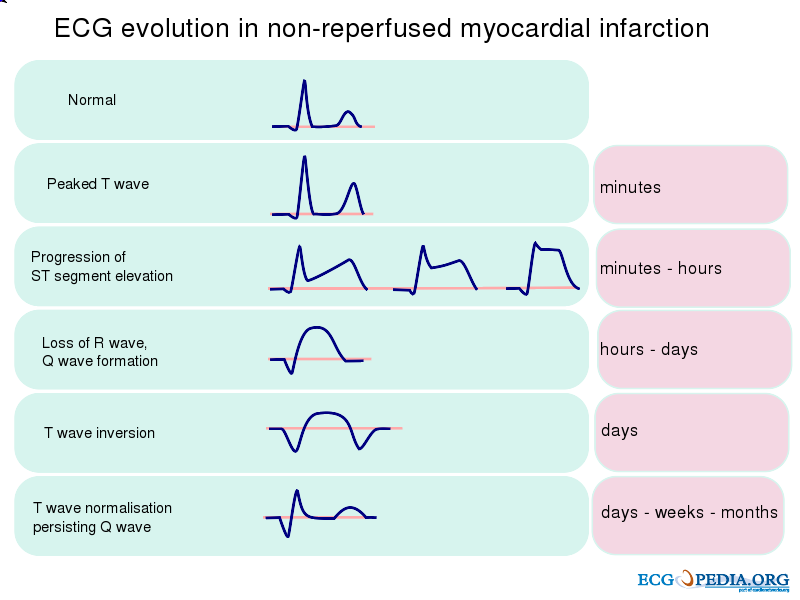
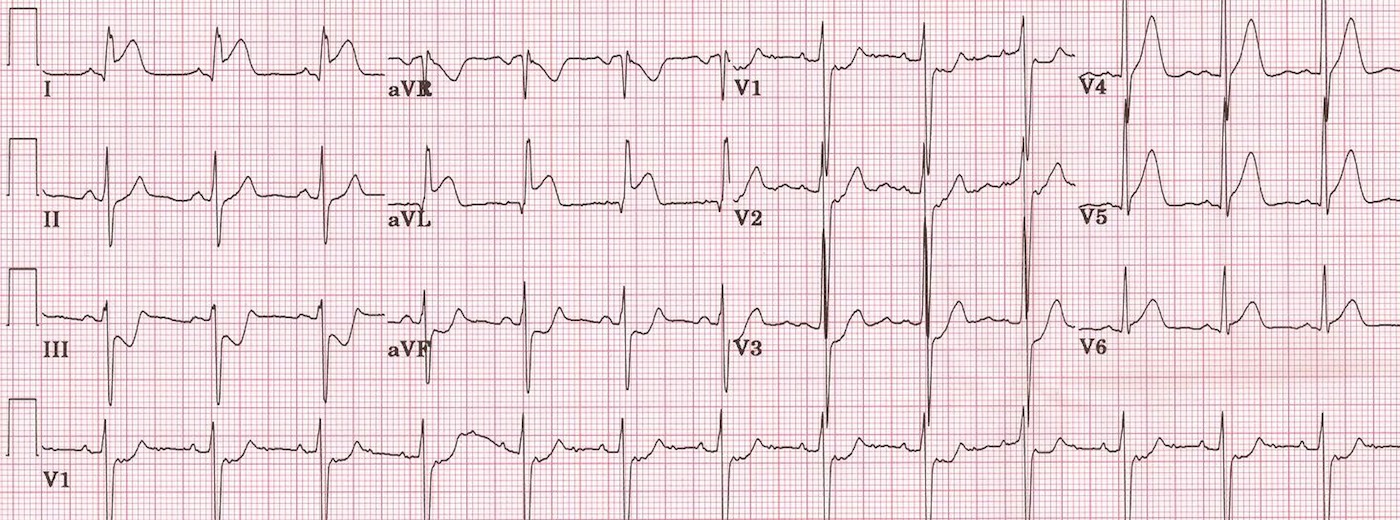
Negro EKG Interpretation
*Evolution of ST changes with STEMI
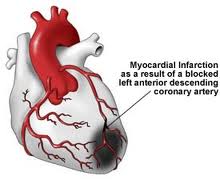
Anterior STEMI: Vessel occluded is LAD. Prognosis is worst of all infarcts due to size of myocardium at risk.
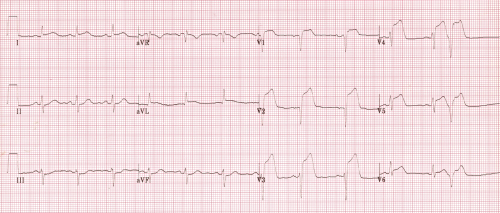
*ECG showing Anterior STEMI
*LAD Occlusion/Anterior MI
*EKG of Lateral MI (Most ST elevation in high lateral leads I, AVL)
Inferior Wall STEMI have risks of RV infarct and hypotension. Caution with IV nitroglycerin as it can cause hypotension. Lower mortality than anterior wall infarction.
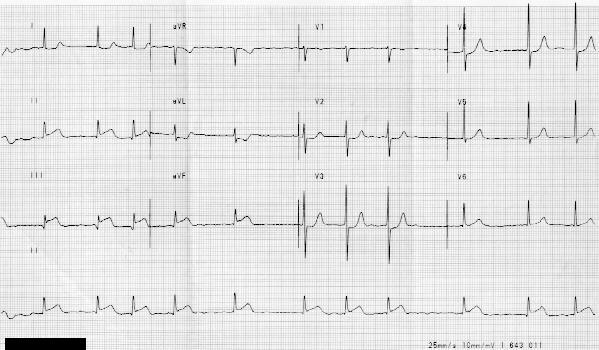
*Inferior Wall STEMI
If in the setting of inferior STEMI, the ST elevation in III is greater than II check right sided leads to evaluate for RV infarct. ST elevation in lead III > lead II suggest RV infarct. These patients need fluids to maintain BP and be cautious with NTG due to risk of hypotension.
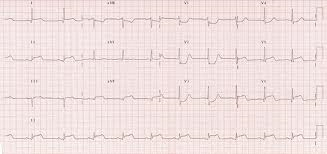
*Inferior Posterior STEMI
Balogun ABC’s of Vasoactive Drugs
Case1 75 yo female with COPD and DM. Patient presents in septic shock. EGDT initiated and patient is persistently hypotensive.
Norepinepherine is the first line pressor for septic shock.
Epi is second line for septic shock (and 1st line for anaphylactic shock). It has both alpha and beta stimulating effects.
Phenylepherine (neosynepherine) increases SVR by pure alpha stimulation. It is third line for septic shock. It can cause reflex bradycardia
Vasopressin increases peripheral vasoconstriction. It is also third line for septic shock.
Case 2 65yo male with antero-lateral STEMI. Patient is in cardiogenic shock.
Dopamine is the first line pressor for cardiogenic shock. At low doses, dopamine vasodilates mesenteric, brain, and renal vasculature. At higher doses it increases cardiac output and SVR.
Dobutamine is the first line inotrope in cardiogenic shock.
Milrinone is indicated for cardiogenic shock in the setting of CHF.
Case 3. 37yo male with hypotension following RSI. Treat with IV fluids and consider a push-dose pressor. Options are phenylephrine, epinephrine, ephedrine.
Probably the easiest use is 1ml of cardiac epi mixed with 9 ml of NS in a 10 ml syringe. This can be given in aliquots of 0.5 ml at a time. Data supporting push-dose pressors is basically from the anesthesia literature. Most of the patients in these anesthesia studies are young healthy females with transient hypotension from spinal anesthesia. No faculty would use push-dose pressors for post-procedural sedation hypotension. They would use it in a critically ill patient to manage post intubation hypotension or bridge the patient until a central line is placed.
No pressors for hypotensive trauma patients. They need volume replacement. Exceptions would be neurogenic shock and septic shock.
Jeziorkowski 5 Slide Follow Up
78 yo female with hx of COPD and O2 sat of 70%. She had a fever of 39.2. Severely dyspneic. Patient had just been discharged from the hospital and family noted patient has not been herself for the last few days.
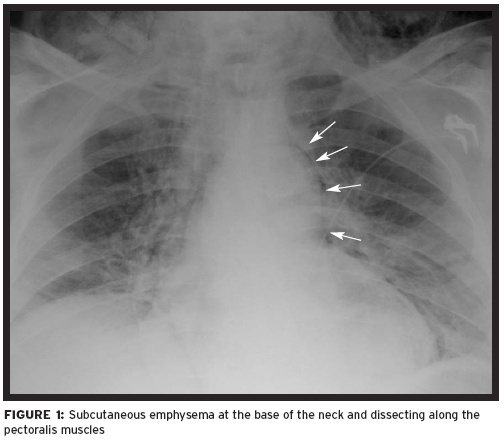
Chest X-Ray shows extensive subQ emphysema. Patient had a TEE during her recent hospitalization. Diagnosis of esophageal rupture was entertained. Iatrogenia is the most common cause of esophageal rupture.
*Esophogeal rupture with mediastinal and subQ air
3 areas of esophageal narrowing: cricopharyngeus, thoracic vessels, and lower esophageal sphincter. If the esophagus ruptures at the cricopharyngeus, the mortality is 6% . If rupture is at either of the other two narrow points, the mortality is around 33%. No clear reason why except that mediastinal contamination is more likely at these lower points.
Esophogeal rupture is a difficult diagnosis to make. Options for diagnosis are esophogram, endoscopy, and CT. Once diagnosed, give broad spectrum antibiotics, consider anti-fungals for the recently hospitalized patient, emergently consult surgery, give supportive care.
Delay in diagnosis results in increased mortality.
Purnell Altered Mental Status Time-Based Approach
What could kill the altered patient in next few seconds: non-perfusing rhythm, airway issue, hypoventilation, and hypotension.
Think to check glucose and consider narcan before intubating the altered patient. In the same vein, consider a c-spine injury prior to manipulating the neck for intubation
What could kill the altered patient in the next few minutes: hypoglycemia, hypothermia/heat stroke, MI, aortic dissection/rupture, intracranial hemorrhage, overdose, hyperkalemia.
What could kill my altered patient in the next few hours: Sepsis, meningitis, metabolic derangements, toxins, intracranial mass, necrotizing fasciitis, intra-abdominal catastrophies, TTP, non-convulsive status epilepticus. Hypo/hyper-thyroidism, neuroleptic malignant syndrome, serotonin syndrome.
Re-examine the abdomen in altered elderly patients multiple times to identify subtle tenderness. Have a low threshold to image abdomen in the altered elderly patient.
TTP mnemonic: FAT RN = Fever, Anemia, Thrombocytopenia, Renal dysfunction, Neurologic deficit. If the patient has 3 of these, start plasmaphoresis. Don’t Give Platelets, it will worsen the clinical situation.
For non-convulsive status, look for fasiculations of the eyelids or muscles in the hand. Elise picked up a case of this recently by noting eye deviation in an altered patient.
Kelly comment: In patients who are on thyroid meds and you want to check their thyroid function, get a free T4 in addition to TSH. The TSH will likely not be diagnostic if patients are on thyroid meds.
Labs are the best way to separate NMS and Seratonin syndrome. NMS will have elevated LFT’s, elevated CK, elevated WBC’s, low iron.