Experimenting with new format today. About 5 take home points for each lecture
Burns (visiting professor) Transfusion Safety
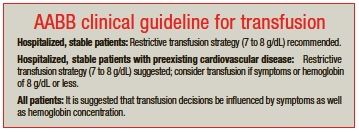
1. In general, Less is More when you are considering transfusions. U.S. physicians transfuse more blood products than European and Canadian physicians due to individual practice variation being greater in the U.S. Recent studies have shown that increasing # of units transfused of any blood product correlates directly with increased mortality, length of stay and wound complications even when controlled for patients’ severity of illness.
2. Patient outcomes are better with a transfusion threshold of HGB=7 rather than 8 or 10 unless a patient is having ACS. Harwood comment: Is 8 really better than 7 for ACS? Dr. Burns: Yes there is data that the mortality is less for ACS at a transfusion trigger of HGB=8 rather than 7. When you do transfuse, only transfuse a single unit and then re-assess before deciding to give a second unit.
3. Transfusion trigger for normotensive upper GI bleeds is HGB=7. The study that this recommendation is based on stipulated that EGD would be performed within 6 hours. Girzadas comment: If you are seeing a patient at night and EGD won’t happen for several hours should you make the trigger 8? Dr. Burns: This is a clinical decision. I may make sense to transfuse at 8 if EGD won’t be available for several hours.
4. Think of a blood transfusion as a liquid transplant. Stored blood cells become more sticky and inflexible. Stored blood acts as a nitric oxide scavenger that causes vasoconstriction. Dr. burns showed arterioles in a patient that received transfused blood and you could see the vasoconstriction. Stored blood is also pro-inflammatory and pro-thrombotic. It is unknown how long blood can be stored before these types of changes progress to the point of affecting patient outcome.
5. TRALI (transfusion associated acute lung injury) is the #1 cause of transfusion related death. TACO (tranfsuion related circulatory overload) is #2 and likely to soon overtake TRALI. Physicians frequently volume overload patients with blood transfusions.
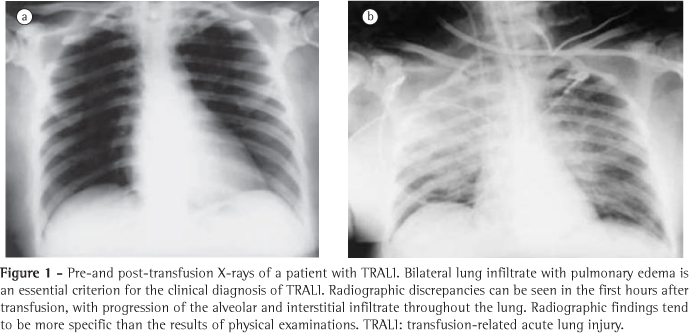
*TRALI
* General Transfusion Guidelines
Permar STEMI Conference
Thanks to Dr. Trale Permar for sharing his EKG slides!
1. Prinzmetal’s angina is due to focal coronary vasospasm. EKG can show ST segment elevation. It is not associated with coronary artery plaques. It can cause arrhythmias. Occurs predominantly in younger women smokers. Associated with other vasospastic diseases such as Raynaud’s and migraines.

*Prinzmetal’s EKG with ST elevation in AVL
2. Myocarditis can be due to bacterial, viral, autoimmune or medication causes. Clinical picture can present like a STEMI with ST changes and elevated troponin. It can also look like acute decompensated heart failure. Cardiac biopsy is the gold standard for diagnosing myocarditis. Paul Silverman said they don’t routinely due biopsy because it has not been shown to improve outcome. MRI can be useful to diagnose myocarditis. Rule of thumb: You diagnose peri-myocarditis at your peril. If it looks like a STEMI, treat it like a STEMI and take patient to the cath lab.
3. Patient with severe anemia had a globally ischemic EKG. ABG is the best test in our ED to rapidly get a HGB. The treatment is PRBC transfusion. Paul Silverman said he would not take a severely anemic patient to the cath lab. The need for blood and resuscitation takes patient out of the mandate for a 90 minute door to needle time. You have time in these patients to resuscitate them. Harwood comment: This patient did not have a STEMI. She has global ischemia due to anemia. She needs PRBC replacement.
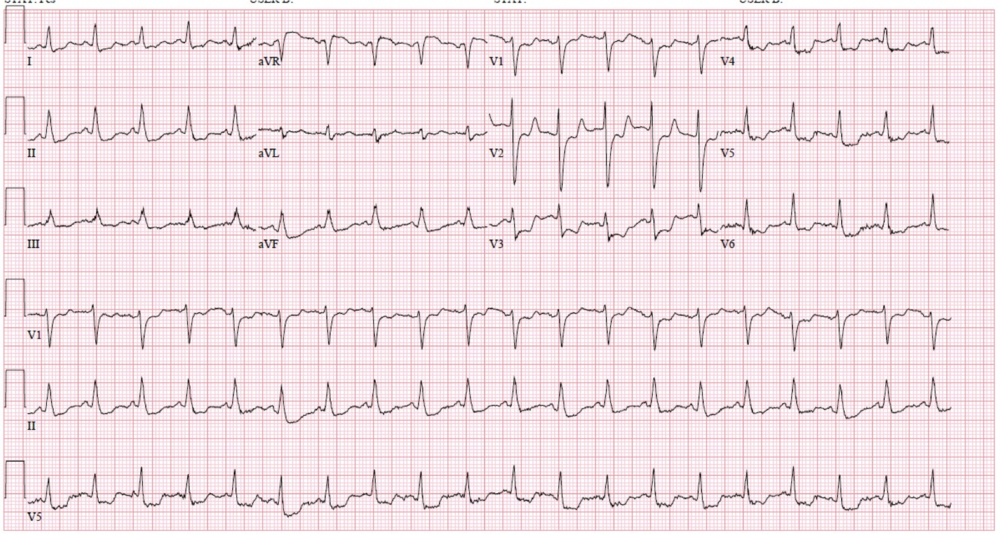
*Global Ischemia due to anemia EKG
4. STEMI and RBBB: Any ST elevation in RBBB is always abnormal. The key is where the ST segment starts. It has to be at least 3 small boxes out from the start of the QRS (120ms).

*RBBB & STEMI (inferior ST elevation)
5. Tall T wave in V1 > V6 is a early indicator of ischemia.

*Tall T wave in v1
6. AVR ST elevation with diffuse ST depression is an indication for Cath Lab was the consensus of the cardiologists present. It is an indication of multi-vessel disease.

*AVR ST Elevation with lateral ST depression
7. There is no longer a strong indication to give 600mg of Plavix in the ED for acute STEMI's. The cardiologists can give brylenta in the cath lab instead. This lowers the risk of bleeding for patients who end up going to CABG. This is cardiologist dependent so speak with them about their preference.
Febbo/Harwood Oral Boards
Case 1. Weakness after large meal including some alcohol. Diagnosis was hypokalemic thyrotoxic periodic paralysis. Patient developed V-Tach while in the ED. Critical actions: Give beta-blocker, give KCL, and synchronized cardioversion for the V-Tach. Teaching points: This disease is due to a mutation in potassium channels (channelopathy). EKG in this case showed U waves due to hypokalemia. Asian patients are most common. 95% are males. Associated with exercise, carbohydrate load, etoh, and stress. Episodes last on average about 13 hours. You have to be cautious on how much potassium you give, because patients can have a rebound hyperkalemia. Probably give 40meq. Give propranolol in 1 mg doses.
*Hypokalemic and hyperkalemia EKG changes. U wave becomes more prominent with worsening hypokalemia
Case 2. 14yo female with blurry vision. Normal Vitals. Patient also has headache. Physical exam showed papilledema. LP demonstrated an opening pressure of 280mm H2O. Diagnosis is idiopathic intracranial hypertension. Critical actions: CT scan of head followed by LP to check opening pressure. Teaching points: Most commonly identified in obese females. It can cause blindness. Look for other papilledema causes. Visual fields have to be checked because that is the earliest eye finding. Idiopathic intracranial hypertension can be related to oral contraceptives, vitamin A, and steroids. Patients can report hearing intracranial noises or pulsatile tinnitus. Opening pressure has to be checked with the patient laying on their side. Diamox is the initial treatment. Surgical treatment includes stenting of the venous sinus, optic nerve sheath fenestration, or a CSF shunt.
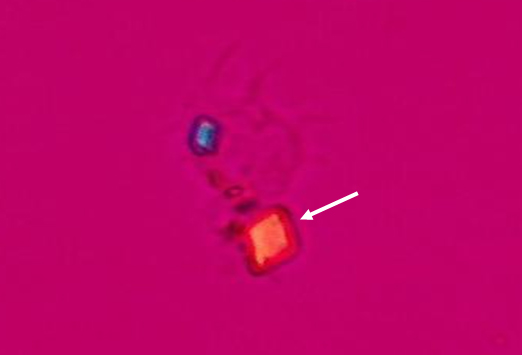
Case 3. 50yo male with 2 days of wrist pain. No history of trauma. Xrays are negative. Joint aspiration performed. Synovial fluid shows gout. Critical actions: wrist xray, pain management, and arthrocentesis. Teaching points: Gout cocktail= hi dose ibuprofen 800 QID, single dose of po colchicine 0.6 mg, 10 mg of po decadron, and norco. This cocktail is advocated by Jim Roberts of Roberts & Hedges fame.
*Uric acid crystal
*Calcium pyrophosphate crystal
Htet Trauma Lecture Facial Trauma
50yo Female with facial injuries due to MVC. Pt had multiple facial fractures.
1. Airway is at risk due to airway edema, loss of mandibular or facial bone support, aspiration, avulsed teeth, and bleeding.
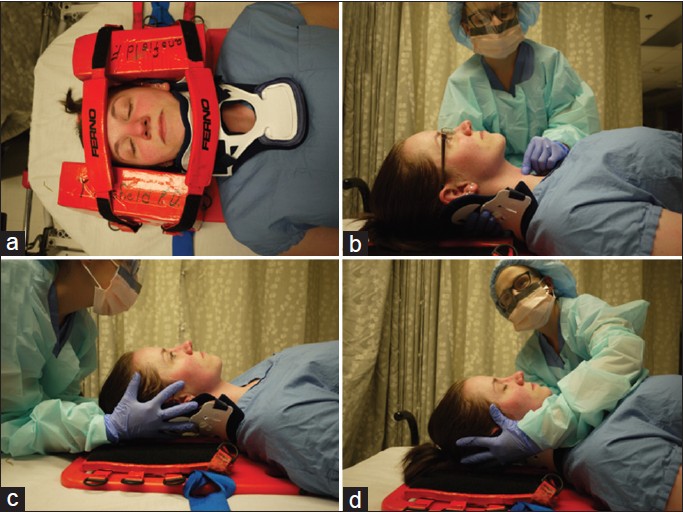
2. Endotracheal intubation preferred over nasotracheal intubation. Best approach is video laryngoscopy unless bleeding severely obstructs video view. If so, attempt direct laryngoscopy. You can use intubating LMA as a bridge device. Surgical cricothyrotomy is your go-to rescue technique if intubation is impossible. If you have time fiberoptic intubation may be an option. All faculty present felt that retrograde intubation techniques were “relegated to the dust bin of history”
3. Manual in-line stabilization is superior to a c-collar in minimizing movement of c-spine and giving optimal view of the airway during intubation.
*Manual in-line stabilization C and D
4. CT head is 90% sensitive for picking up facial fractures. Panorex can pick up alveolar ridge and mandibular fractures that CT max-face can miss.
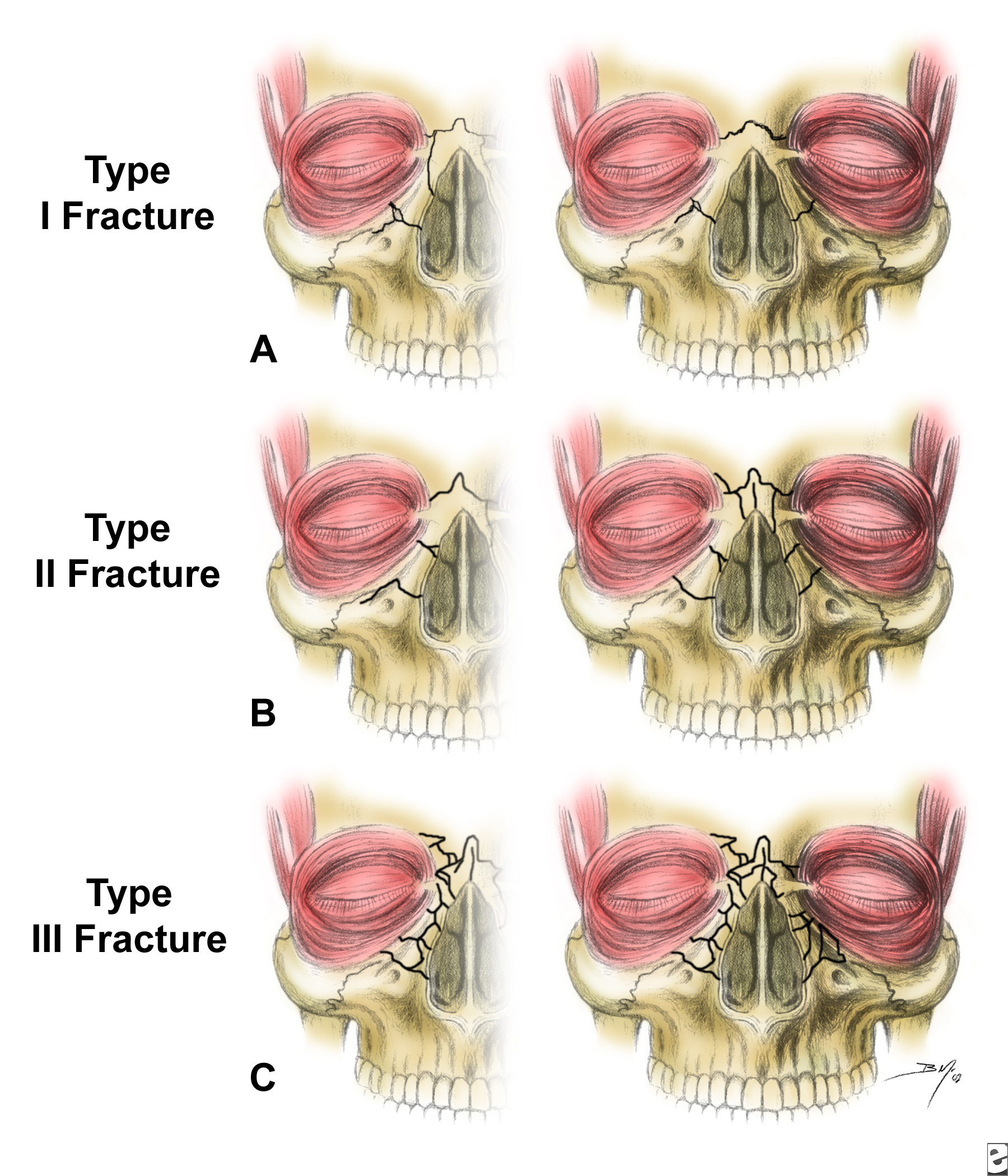
5. Fractures that require admission: Nasoethmoid, zygomatic arch, Lefort, and Tripod fractures.
*Nasoethmoid fractures
*LeFort Fractures
6. Dr. Omi comments: Defining/diagnosing facial fractures is not clinically important initially. Manage the airway first! Identify and manage other life threatening injuries next. After all that you can start to work up facial fractures.
Paik Safety Lecture
2 Psychiatric patients: 1 escaped from ED, the other was suicidal and was in her room for a prolonged period of time with no sitter.
1. There are 30,000 suicides per year and 5% occur in hospitals. At least 50% of the suicides that occur in hospitals result in a lawsuit. These are high-risk patients.
2. Be sure psychiatric patients have their clothing and belongings taken from them.
3. Be sure every patient has a sitter.
4. Having a physical ED space for psychiatric patients that is capable of being locked would be useful to prevent patients absconding from the ED.