Special thanks to guest scribe Dr. Elise Lovell!
Conference Notes 10.14.2015
8 am: Oral Boards: Harwood vs. Paik
Case 1: 20 month female with abdominal pain/vomiting. Lead poisoning: Look for neuro sx, GI sx, hematology. May show up as radio-opaque flakes on KUB. CBC with basophilic stippling. Lead levels useful. Need to notify Health Department, call Tox Consult, remove from source, assess other kids. Treatment Dimercaprol (BAL) IM, followed by Ca Na2EDTA.
Case 2: 20 yo male unstable Transmediastinal GSW. Need Echo, CT Chest, potentially bronch/esophagus. Codeà ED thoracotomy; Shock/>1500 Chest Tube output immediately or 200 cc/hour for 3 hoursà OR; Stableà workup.
Case 3: 30 day female, ALTE: Pertussis. Reason for apneas in neonate: bronchiolitis (RSV or influenza), pertussis. May have 6 weeks of cough. Treat with macrolide, exposures to be treated as well. Diagnosis with PCR. Admit if apnea, seizure, pneumonia, age <4months, respiratory distress, poor feeding. Immunize!
9 am: Radiology-Head CT West and Ede:
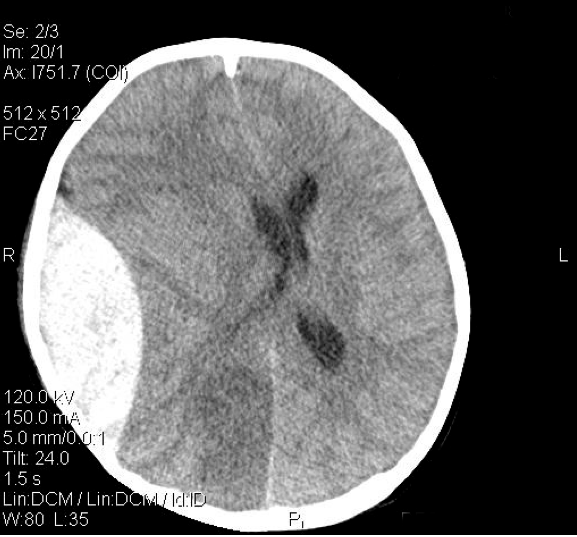
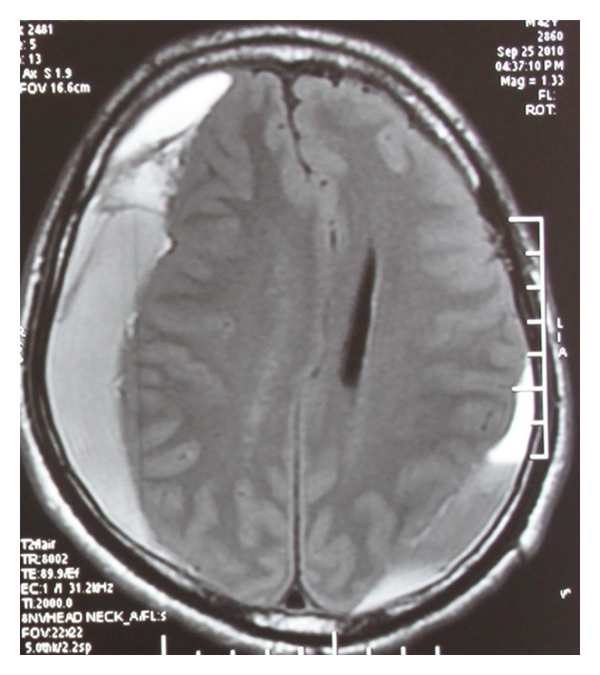
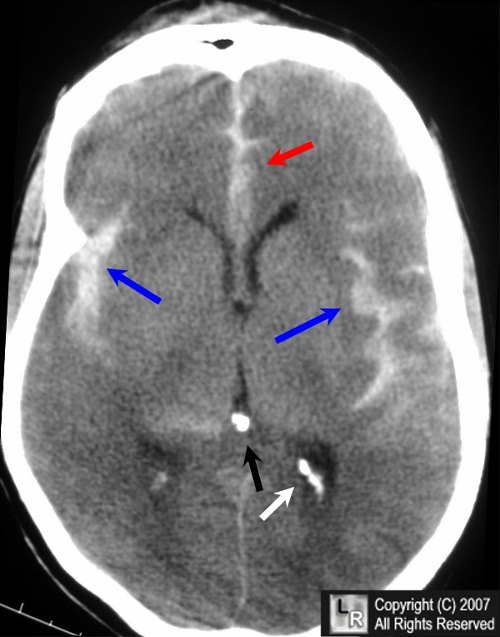
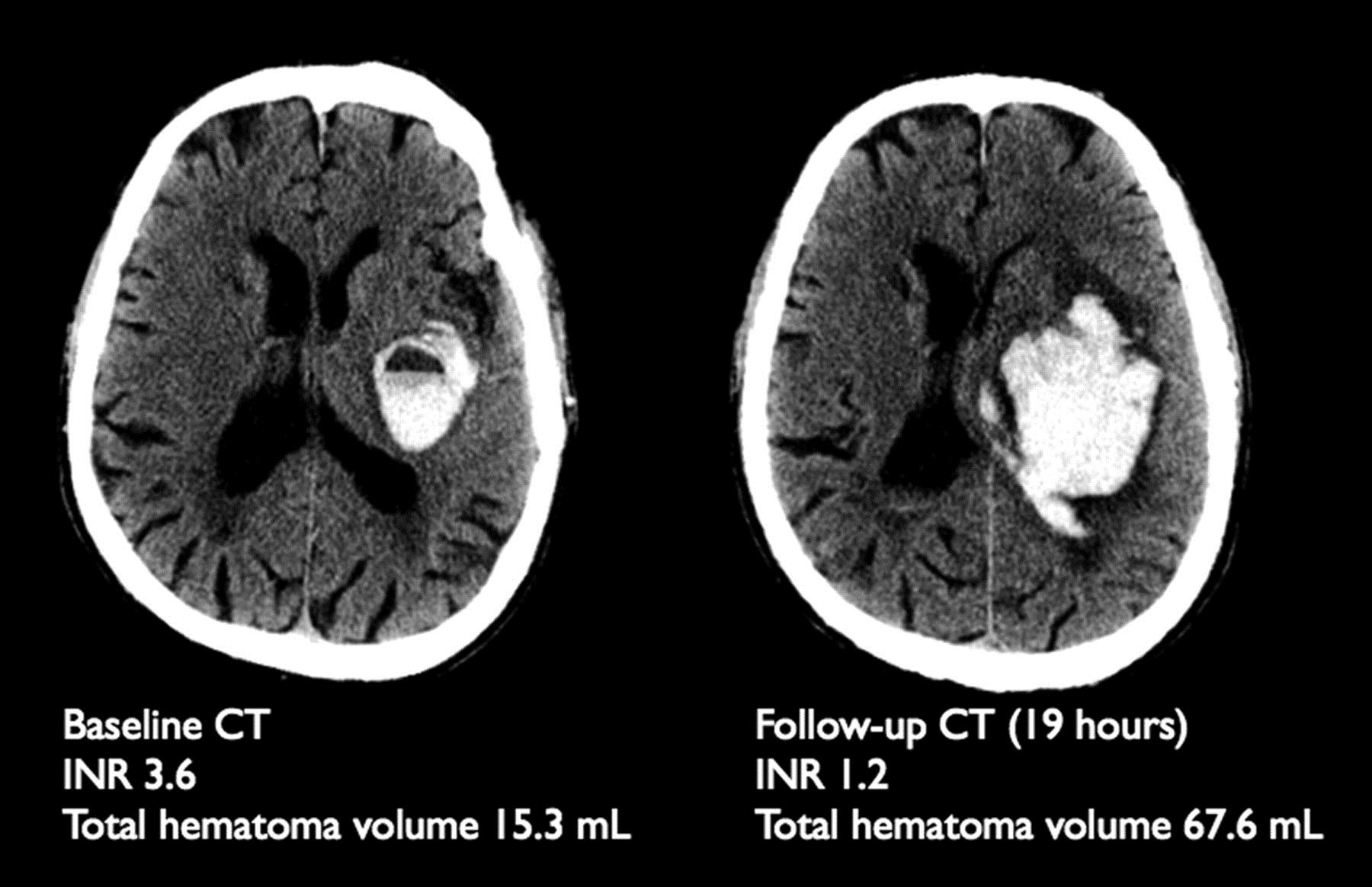
Use systematic approach: “Blood Can Be Very Bad” = blood, cisterns, brain, ventricles, bone
Bleeds:
Epidural hematoma, lentiform, does not cross suture lines. Usually arterial (middle meningeal classic). May have lucid interval then decompensate.
Subdural hematoma, crescent shape, does cross suture lines, usually venous, may be indolent, with non focal neuro exam.
Subarachnoid hemorrhage; Hunt and Hess classification, 75-80% aneursymal, CT excellent sensitivity within first 6 hours then drops off.
Intracranial hemorrhage, hypertensive -> basal ganglia.
Ischemic CVA: often negative CT in first hours of presentation. Look for hypoattenuation/sulcal effacement, blurring of basal ganglia in MCA infarcation, dense MCA sign (clot in MCA), insular ribbon sign-hypodensity and swelling of insular cortex.
Infections: in meningitis CT before LP if AMS, focal neuro deficit, seizure, concern for mass (malignancy, papilledema). Viral encephalitis CT usually normal initially, think about temporal changes for herpes.
Herniation: 6 types.
9:30 am: Syncope Lee:
Is it really syncope, or is it seizure , vertigo, etc?
Is it isolated primary syncope or is there an underlying cause (secondary syncope-cardiovascular, neurology, medication related)? Be more worried if no prodrome symptoms (drop attack), or if exertional syncope.
History and physical, including PMH, are key to identifying the cause.
In the young, think about dysrhythmia, seizure, pregnancy, blood sugar/electrolyte/volume status, bleeding/anemia.
Hypertrophic cardiomyopathy (LVH + Q waves)
Brugada (incomplete RBBB + downsloping ST segment)
WPW (delta wave + short PR)
Arrhythmogenic Right Ventricular Dysplasia (epsilon wave-upright wave, looks like an Osborn wave in a normothermic patient)
Who can go home? Low risk factors: primary syncope without concerning historical factors, age <50, no h/o CV disease, normal exam, normal ECG
San Francisco Syncope rule: H/O CHF, Hct<30%, abnormal ECG, SOB, SBP < 90. Careful-initial sensitivity of high 90s hasn’t held up well in other studies, but need to apply in correct population...a patient with a SAH would be low risk by this rule.
Rose syncope rule adds BNP, low O2 sat, in order to increase sensitivity.
None of the many rules are terrific....
CT extremely low yield-don’t do it unless high suspicion for CNS etiology, or if on anticoagulants, or if unwitnessed and old.
Can’t miss diagnoses? PE, SAH, Aortic dissection, AAA, ectopic pregnancy.
10:00 am: Toxicology Carlson: Aspirin toxicity
Shows up in variety of products (arthritis meds, IBD meds)-beware of combination products and brand names such as BenGay, Peptobismol, Alkaseltzer!
Enteric preps unpredictable absorption.
Low Volume of Distribution (good for dialysis) and high protein binding (bad for dialysis but can affect this by changing pH).
Pathophysiology/Clinical presentation: Key ABG: respiratory alkalosis + metabolic (lactic) acidosis. Will see hyperventilationàstimulates resp. center in medulla. Also stimulates vomiting center, causing GI loss of potassium. Uncouples oxidative phosphylationà metabolic acidosis and fever. Hypo or hyperglycemia. Relative CNS glucopeniaàadds to AMS. Direct ototoxinà tinnitus.
Single OD:
Mild: Tinnitus, N/V, hyperventilation hyperpyrexia
Intermediate: Agitation, dehydration, acid/base problems, non-cardiogenic CHF
Before they die: Lethargy/coma, hyperthermia, cerebral edema, seizure, oliguria, hypotension. A death from salicylate poisoning is a CNS death-watch their mental status!
Much less predictable symptoms with chronic OD, associated with delay in diagnosis, have higher CNS burder, more common in elderly, greater morbidity at lower levels.
Intubation-Keep Respiratory Rate High!! Avoid iatrogenic acidosis.
Treatment:
Charcoal-absorbs aspirin very well. Skip it if > one hour or if already symptomatic. Multiple dose no longer recommended.
IV Bicarb/urine alkalinization for ion trapping (bound vs unbound salicylate). Need to be sure to supplement potassium!! Body will resorb potassium if low, and waste HCl, so urine will stay acidotic unless potassium replaced. Follow urine pH, not ABG. Goal of urine pH > 7.5.
Dialysis!! If AMS, ARDS/CHF, failing standard therapy, pH , 7.20, level >90 mg/dl. In chronic, symptoms trump level.
11:00 am: ENT/Epistaxis: Alexander
Assess if blood thinner use/predispositions for severe bleeding. Consider CBC, coags. Anterior= more common. Posterior=more serious.
Anterior: Kiesselbach’s plexus, often secondary to mucosal dryness, conservative measures to manage
Posterior: look at back of throat, often elderly patients with inherited or acquired coagulopathy. More challenging to control.
Treatment: ENT box! Get afrin, viscous lidocaine. Ask patient to blow nose, expel clots, in order to help vasoconstrictors to work. Direct pressure with fingers or 2 tongue depressors taped together for 10-15 minutes. Good lighting-use nasal speculum. If no anterior source visualized, consider posterior bleed. Use Frazier catheter as needed. Consider silver nitrate cautery if you see specific source of bleeding, cauterize around the bleeding site. Be prudent-can cause septal perforation. Thrombogenic gels and foams can help. Tranexamic acid (antifibrinolytic) can be used as topical application of injectable form.
Packing: Rapid Rhino balloon-soak balloon in water for 30 seconds before insertion. Blow up with air. Insert parallel to floor of nose. Alternative preformed sponge-Merocel. Consider coating with bacitracin ointment. Wet with saline AFTER insertion. For posterior pack, consider parenteral analgesics. Inflate posterior balloon first, then anterior balloon. Use minimal inflation necessary to control bleeding-can cause nasal necrosis!
Ant/Post balloon packing:
Antibiotics (Keflex) to help prevent sinusitis/toxic shock syndrome.
Admit if posterior packing required (airway obstruction, apnea, hypoxia, syncope/cardiac dysrhythmia possible).
Failed management-call ENT, may need embolization. Also “greater palatine foramen block” with 2 cc of lido + epi. Dr. Sherman hasn’t done it, so beware...
11:30 am: Pulmonary SG: Lovell
Primary spontaneous pneumothorax-if stable, consider treating with aspiration +/- Heimlich valve catheter, regardless of size of PTX. They usually don't need chest tubes!
Tuberculosis
•Primary infection (usually asymptomatic, infrequently pneumonitis)
•Latent (+PPD, Ghon complex on CXR reflecting healed primary)
•Immunocompetentà5% risk of progressing to active disease within 2 years, 10% lifetime risk
•Reactivation-fever, night sweats, hemoptysis, weight loss
HIV-most common cause of pneumonia is Streptococcus pneumoniae. Pneumonia in HIV associated with high rate of bacteremia. Pleural effusions are common. Think about TB with CD4 counts 250-500 (not just seen in low CD4 counts). If pneumothorax, think PCP.
High risk factors for lung CA: male, smoking, age > 40, no lower resp. infection symptoms. If abnormal CXR or high risk factors or active bleeding, needs CT + bronch.
Pleural effusions: transudate vs exudate
Exudate if:
•Pleural fluid /serum protein > 0.5 or
•Pleuralfluid /serum LDH > 0.6 or
•Pleural LDH > 2/3 upper limit serum LDH
Asthma and pregnancy: Beware of CO2 retention! During exacerbation, normal alkalosis of pregnancy is aggravated, leading to decreased placental blood flow. Hypoxemia is usually more severe in fetus than in mother.
•PaO2 < 70 = severe hypoxemia
•PaCo2 > 35 = respiratory failure
•B2 agonists, inhaled and oral steroids all safe
Bronchitis
•GOLD: Chronic: treat COPD exacerbations with antibiotics if increased SOB with increased sputum volume/sputum purulence, or intubated
• ACCP: For acute bronchitis, the routine use of antibiotics is not justified
Lung Transplant Pearls:
•Usually receiving tacrolimus (over cyclosporin) and mycophenolate mofetil (over azathioprine) and prednisone.
•Lots of drug toxicity and drug interactions-renal insufficiency (tacro and cyclo)
•Fever, cough, sputum, CP, FEV1 decline = rejection or infection. Isolate. Bronch.
•Most frequent cause of death long termà bronchiolitis obliterans (wheezing, tx antirejection agents)