Kmetuk M&M
71 yo female presents with syncope and altered mental status. BP 72/60, HR 140, RR 28, T 35C, O2 Sat 95%. Rhythm strip shows Afib with RVR. Only history available was that the patient was discharged from another hospital the day before for unknown illness.
Initial evaluation included a negative FAST exam. Bedside ECHO showed a suspected enlarged RV. Abdominal Aorta was normal.
On the physical exam abnormal findings included: diaphoretic skin, cold skin, pale conjunctiva, diminished peripheral pulses. Stool was heme negative.
EKG was Afib with RVR. The initial therapeutic action was to cardiovert to see if the Afib was the cause of her instability. Cardioversion converted her to sinus but she was still altered and hemodynamically unstable.
Patient is next intubated. IV fluids were given and pressors started.
ABG shows a significant lactic acidosis, HGB is 7, PO2 is low for 100% FIO2 (215)
CXR is non-contributory to the diagnosis.
The patient’s vitals improved with the above treatment. Patient was placed in the Queue for CT of chest and abdomen. The CT was delayed due to Radiology wanting a Bun/Cr prior to the study.
Family arrives to the ED and relates a history of DVT, mixed connective tissue disorder, and pulmonary hypertension for the patient. Patient also had a recent cardiac cath and a subsequent right femoral pseudoaneurysm during her recent hospitalization. The pseudoaneurysm was treated during that prior hospitalization with ultrasound guided thrombin injection. Patient at that time was also started on Xarelto.
In the ED , the CT PE was negative. CT of the Abdomen and Pelvis showed a large retroperitoneal bleed.
*Retroperitoneal Bleed
The patient was given FEIBA and the massive transfusion protocol was initiated.
Patient went to IR for vessel embolization. In the hospital she had a stormy hospital course and eventually died.
Retrospective Considerations:
- Earlier intubation could be considered
- Repeat FAST exam after sedation to get a better image
- More frequent re-evaluations
- Delay in CT scanning cost some time
- Massive transfusion protocol possibly could have been initiated sooner
- Better utilization of resources possibly could have elicited more history earlier in the ED course.
Harwood comments: I am proud of how well you managed this patient. Doing the FAST exam so early was great. It really helped you narrow down the differential diagnosis rapidly. Patients that are agitated from shock need to have shock corrected or they won’t become last agitated. You guys made the right move to not give TPA early on for suspected possible PE. That move would have meant immediate death. It was great that you pushed for the CT despite an abnormal creatinine. You gave blood rapidly. I also liked that you cardioverted Afib acutely. There was a lot of great management moves here.
Think about retroperitoneal bleed when patients are on anticoagulants, have coagulopathy, chronic dialysis also increases the risk, invasive procedures and blunt/penetrating trauma are also rsk factors.
Patients can complain of back, groin, flank or abdominal pain.
Look for cullen’s sign or grey turner’s sign. However, this patient had neither of these.

*cullen’s sign
*grey turner’s sign
Ct plain or with IV contrast will show a retroperitoneal bleed. FAST has a high false negative rate. If you are going to use FAST to identify retroperitoneal bleeds, you should do sequential FAST exams to evaluate for intraperitoneal extension.
Treatment is IR intervention or surgery with fluid and blood resuscitation and reversal of coagulopathy.
Elise comment: You guys did a great job managing this difficult case. As a department we need to find a way to remove the barrier of delaying CT because of Radiology waiting for Bun/Cr result.
Garrett-Hauser Ethics
Ethics in the news: Utah passed a law allowing the state to use a firing squad as an alternate form of execution if they are unable to obtain an appropriate supply of drugs for lethal injection.
American Academy of Pharmacists advises that no pharmacists take part in judicial executions.
Use of firing squads for exeution may go to the Supreme Court for a decision on their legality.
Supreme Court will decide this summer on the use of force against the mentally ill. The decision involves the Americans with Disability Act. This decision may have far reaching ramifications for law enforcement and emergency medicine.
In Illinois, Emergency Physicians can provide information on intoxication levels of a patient when asked by the police. You can’t however call the police to notify the police that a patient involved in a motor vehicle collision is intoxicated. ACEP is against emergency physicians answering police questions about intoxication. It is Shayla’s advice that we do answer police questions. The law is unclear if an emergency physician can refuse to give info to the police. Also the police cannot force emergency department staff to draw ETOH levels or obtain a drug screen. These samples cannot be obtained forcibly from a patient unless it is vital to their emergency care. If the police are pressuring you regarding any of the above situations, contact the on-call administrator and they will contact the hospital lawyer.
Case 1. LVAD patient had 4 teeth pulled at dentist’s office. Patient arrived with profuse oral bleeding. In the ED, patient becomes unresponsive. Patient becomes more awake and refuses intubation. Patient was intubated anyway based on the fact that because he was in extremis he lacked decisional capacity.
Case 2. 38 yo male had head injury and ETOH intoxication. He was a Trauma patient. The patient signed out AMA. Patient fell in the waiting room bathroom and hit his head again. He is brought back into the ED. He then wants to sign out AMA again. There is the question of whether the patient has capacity to make an informed decision to sign out again. Shayla felt that the patient does not have capacity to sign out AMA again. She based this decision on 2 factors : No clear reason why he was so anxious to leave. Already 1 prior bad result from his first AMA decision.
Case 3. 86yo female diagnosed in the ED with pneumonia. Family did not want patient admitted. They were going to provide home care. Patient gets worse in the ED. She required O2. Family still wanted her to go home. If she has to stay in the hospital the family wants no info given to other family members. Shayla made the point that if a family member is making unreasonable demands on behalf of a patient, you can ask a family member to produce the health care power of attorney. This will verify that the family member actually has the legal authority to make demands/decisions.
Case 4. NH patient with history of dementia. The patient arrives in septic shock. The nursing home physician calls the ED and states he wants patient to receive IV fluids and Antibiotics. Patient has NH POLS Form documenting that she has opted to not be transferred to the hospital and did not want IV fluids. Family could not be contacted. Emergency physicians opted to send patient back to the NH to respect patient’s wishes.
Elise comment: This patient has a desire for a peaceful death. The system is working hard to not do that and provide further medical intervention.
Case 5. 8 month infant with gastroenteritis and dehydration. Patient has history of congenital heart disease s/p surgery. Child won’t take po fluids. ED physician wants patient admitted. Mom is refusing and angry and is leaving AMA. Shayla discussed that there were many perspectives on this case. Optimally the ED physician can discuss with mom what she is concerned/angry about and how that can be mitigated. More importantly a decision has to be made regarding how ill the child is. If the child is dangerously ill or has serious cardiac disease, the emergency physician needs to take custody of the child. If the child is not dangerously ill, probably the child can go home with the mom with instructions to get close follow up or return to the ED ASAP.
Jeziorkowski/Herron Oral Boards
Case1. 3yo child with 3 days of sore throat and fever. Patient has trismus. Exam demonstrates a peritonsillar abscess. CT head/neck shows abscess with deep space infection of the neck. Management includes IV antibiotics to cover anaerobes and MRSA. Also there needs to be ENT consultation for surgical drainage. Patient requires frequent reassessment during ED course evaluating for any developing airway concerns.
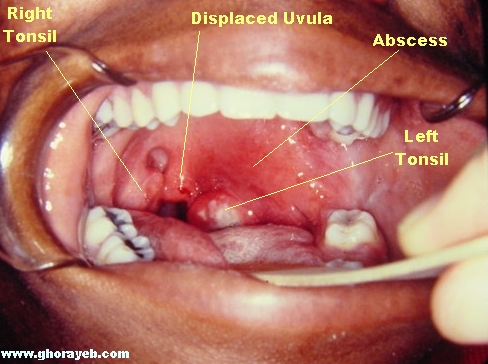
*Peritonsillar abscess
Case 2. Elderly patient presents with headache. Patient has physical finding of tender temporal artery. CT head is negative. ESR is 88. Diagnosis is temporal arteritis . Management includes: document visual acuity, start steroids, consult surgery to arrange for biopsy in the next few days.
*Temporal arteritis
Case 3. 40 yo male brought in by EMS for intoxication. Vital signs are normal. Patient is unresponsive and has signs of head injury.
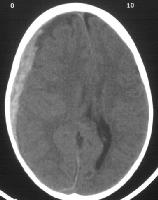
CT shows acute subdural hematoma.
*Subdural hematoma
Management includes: check blood sugar, protect airway with intubation, consult neurosurgery for emergent surgery, seizure prophylaxis, control ICP with mannitol.
Elise comments: Be sure to ask for pediatric patients’ immunization history when taking oral boards. Be careful not to upset kids who have a potentially tenuous airway. Sedate every patient who is intubated, even if they are altered or intoxicated.
Harwood comments: Always get a visual acuity and visual fields on a patient with suspected temporal arteritis. Check for warmth, swelling, tenderness, or knobbiness of the temporal artery. Most temporal arteritis patients can go home unless they have impaired vision. You want to get the biopsy done within one week. You may get a false negative finding on the biopsy if it is done after that first week of oral steroids. In the head injured patient with subdural, clear the neck as soon as possible so you can remove the collar. Removing the collar may improve venous return from the head and lower ICP. Also raise the head of the bed 30 degrees.
Balogun Resuscitation of the Unstable Cardiac Pediatric Patient in the ED
Case 1. 2 week old infant presents to the ED with respiratory distress. Breathing was noted by parents to be rapid overnight. In the morning, the patient became pale and limp.
5 things to know prior to arrival of a critically ill neonate
1. Get the vital signs
2. What is the mental status
3. What prehospital actions have been taken?
4. History
5. Patient’s weight, so you can anticipate drug dosing and device sizing
5 things you want to do prior to patient arrival
1. Stay calm
2. Get pediatric crash cart and broslow tape/pedistat app for drug dosing and device sizing
3. Order Prostoglandin E and/or dopamine
4. Call pediatric cardiology
5. Call pediatric cardiology
On arrival, the infant was cyanotic and working hard to breathe. The infant was arousable only with pain.
First action is to assess airway, breathing, and circulation.
Gain IV or IO access. Intubate the patient.
DDX: Bronchiolitis, Pneumonia, Sepsis, Congenital heart disease/heart failure, anaphylaxis, inborn errors of metabolism.
Cyanosis + tachypnea + shock+ <1 month=congenital obstructive heart disease until proven otherwise
Within the first month of age, unstable congenital heart disease is most frequently ductal dependent. These kids will respond to prostaglandin E.
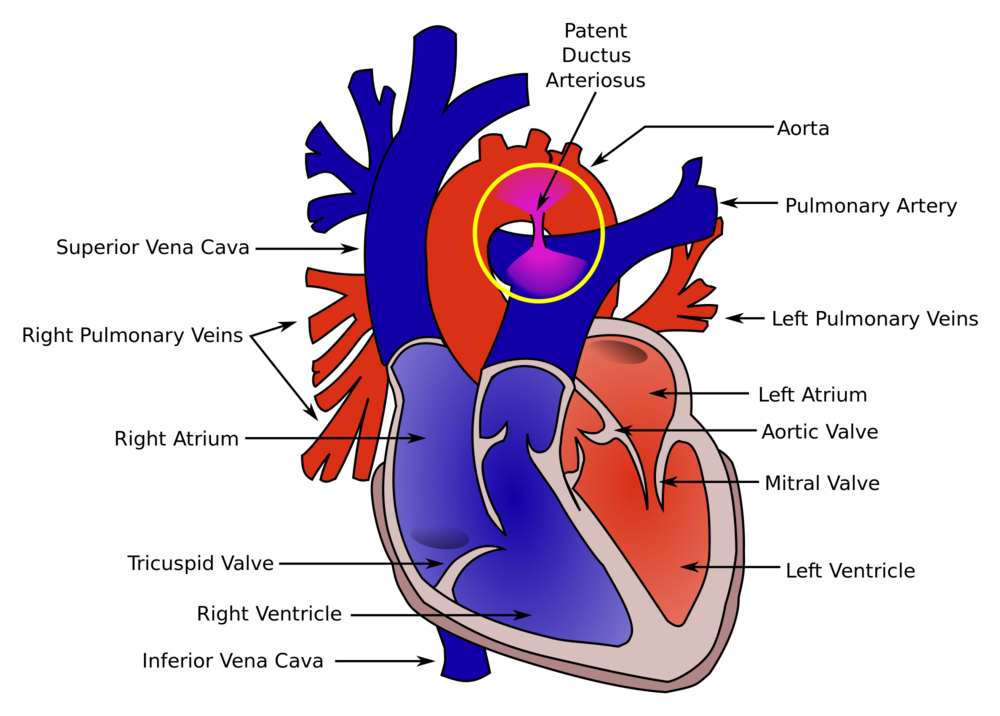
*Ductus arteriosus
Patent ductus blood flow is critical to survival in kids with various forms of heart disease. The ductus tends to close around 3-4 weeks of age. This natural closure can make a stable kid with congenital heart disease become rapidly unstable.
ED management:
1.Intubate early. In this case it is critical to pretreat with atropine. Use etomidate or fentanyl to optimize hemodynamic stability. Use rocuronium if you need a neuromuscular blocker.
2. Keep O2 sat between 80-90%. Higher or Lower is bad.
3. Ventilator management: AC, TV 6 ml/kg, 30 breaths per minute, Peep 5, O2 sat between 80-90%
4. PGE is life saving in an infant <1 month with cyanosis, tachypnea, and shock.
5. Dopamine at 5mcg/kg/min should be started if shock persists after PGE
6. Third line management is an epinephrine drip
7. Give empiric antibiotic therapy after obtaining cultures
Dopamine is first line therapy in infants older than 1 month with shock. After one month they no longer have ductal dependent lesions and PGE is no longer therapeutic.
Elise comment: Have a dosing/sizing App (pedistat) on your phone for pediatric resuscitation. It is a huge help to cognitively offload a lot of mental work doing calculations.
Navarette comment: If an infant has an umbilical stump and they are in shock, you have to consider congenital heart disease and probably give PGE. The umbilical stump falls off usually around a month of age.
Harwood comment: The side effect of PGE is apnea. All patients who are given PGE should be intubated.
Kadar comment: The PICU says you will never be faulted for giving PGE in a shocky kid under one month of age. However, you will be faulted if you don’t.
Residents/RLT Town Hall Meeting
Separate email summary will be sent out to all residents.
Remke Safety Lecture Inventory
The inventory was revamped because the hospital had 500,000 expired products on their inventory shelves.
Our new model is based on the Toyota model. It is a lean supply method. We will have the products that we need to care for our patients, not more or less. We moved to a bin system. There is a tracking system for the bins. Red means inventory needs to stock more frequently, Blue means we are using the product less than expected. Green means our re-stocking is right on track for a particular product.
The locked cabinet can be entered with a Code # (the code is the charge nurse’s 4 digit phone number). The locked cabinet contains anoscopes, extra spinal needles, tonopen, ENT box and doppler. We have to be accountable to bring things like the Doppler and the tonopen back to the cabinet.
Supplies are grouped into wound care, airway management, and patient care. These subgroups are color coded as well.
Elise comment: We should have headings on each shelving system listing the subgroup of materials on each shelving unit.
There is a catalog on the front and back rows of the shelving units that lists every item on the shelves.
The phone number to use to contact inventory help is 41-8271 or 41-6282.
Each ED patient room is restocked 3 times a day. Inventory techs should be present at every Code Yellow and Code 44’s. No one should be questioning residents about how they are preparing for an incoming Trauma or Code 44 patient. If you need to open the airway box prior to the arrival of a potentially critically ill patient definitely do it.
Regan comment: A better labeling system or a tablet-based system that has a catalogue of items listed in commonly used ED doc terminology for each item would be helpful.