Permar STEMI Conference
Case 1. Sorry I missed this first case
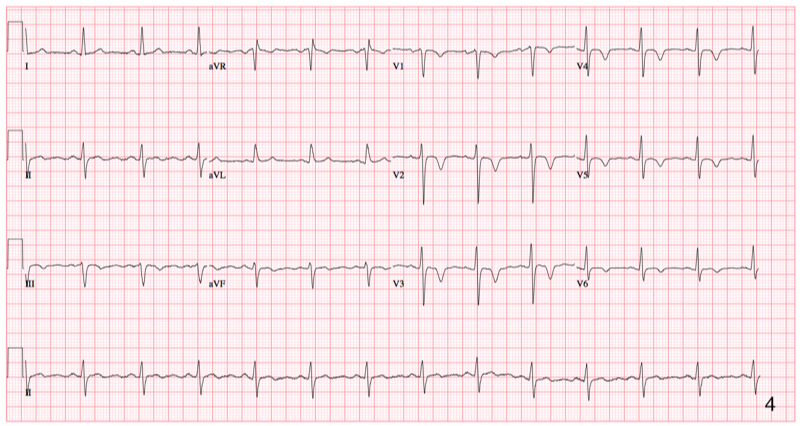
Case 2. 41 yo male with no prior cardiovascular diagnoses presents with chest pain and diaphoresis. In the ED the patient was hypotensive. EKG showed an inferior/posterior MI. A Code STEMI was called immediately.
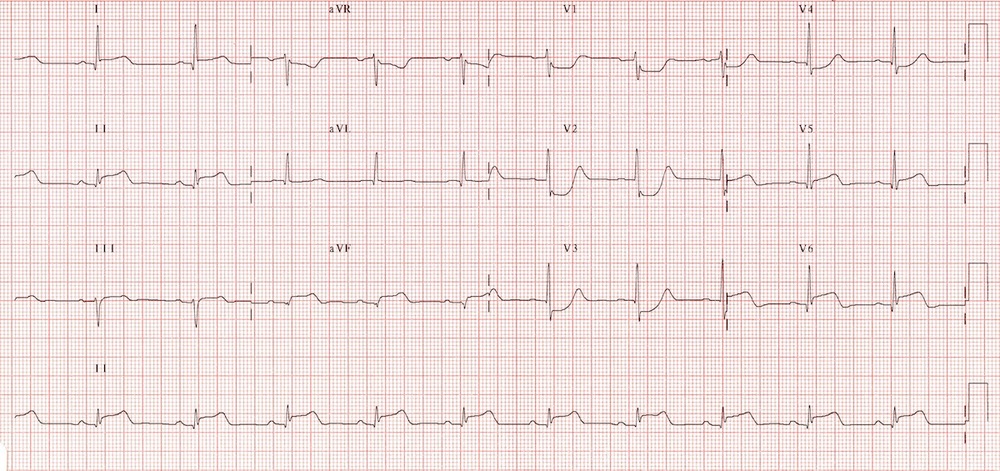
*Inferior-Posterior MI
Patient developed torsades in the ED. He was resuscitated multiple times. He made it to the cath lab. Cath showed severe multi-vessel disease. Despite a balloon pump, ICD, medical resuscitation, and angioplasty the patient died.
Dr. Dia comments: Using a larger volume balloon in the balloon pump (50ml vs 40 ml) is more effective. There are also temporary ventricular assist devices or ECMO that could be useful is these situations. Balloon pump by itself has not been shown to improve 30 day mortality.
Dr. Levin and Silverman comments: There are Impella devices that could be possibly placed in the cath lab. These are percutaneously placed left ventricular assist devices.
Dia comment: To support a cardiac arrest patient with ECMO it has to be VA ECMO so that you are supporting the left heart not just the right heart.
Harwood comment: This patient’s anatomy was fatal. Be very careful with vasodilators (nitro) in patients with inferior/posterior MI’s. Think RV infarct. Also intubate these very sick patients prior to sending them to the cath lab. The cardiologists agreed with these comments.
Silverman comment: I have developed a lower threshold to intubate patients prior to cath. If we have to intubate during the cath, it slows down and interrupts the cath procedure.
Levin comment: Intubation in the cath lab takes more time than in the ED. Patient selection for these unstable patients is critical for making the best decision whether to go to cath or not .
Group discussion regarding taking post-arrest patients to cath lab. There is an EM push to get post-arrest patients to the cath lab. Cardiology has the some contrary concerns that post-arrest patients frequently die in the cath lab or shortly therafter. Careful patient selection and good communication between EM and Cardiology is crucial.
Case 3. 55yo male had out of hospital V-Fib Arrest. Patient was resuscitated pre-hospital. ED EKG showed an anterior MI.
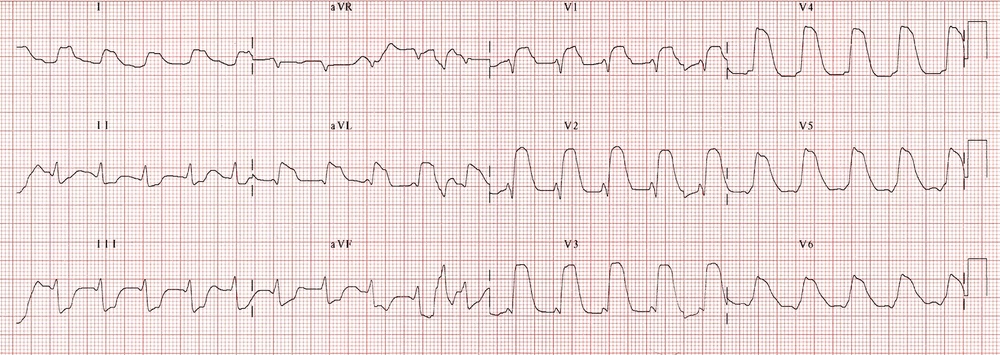
*Anterior MI
Silverman comment: This patient was continuously unstable in the ED with repeated V-Fib arrests. He should go to the cath lab, but he was never stabilized long enough to make cardiac cath possible. He recommended loading the patient with amiodarone and if you can get a period of time with a blood pressure present, get him to the cath lab.
Be sure you document you cath lab decision making. Document that the patient is unstable, that the case is complex. This will take them out of the 90 minute timing issues.
This patient eventually stabilized for cath lab. He had a 100% LAD occlusion. He was placed on balloon pump. Patient was transferred to MICU and had another V-fib arrest. He was resuscitated but then had PEA and died.
Dia comment: PEA suggests to me either a respiratory problem or ventricular rupture. Silverman comment: He had respiratory failure due to pump failure and worsening pulmonary edema. We are moving toward having an ECMO device or Impella device to support these patients beyond a balloon pump. Cooling the post-arrest patient is also super-important. We can place a cooling catheter in the cath lab if necessary.
Harwood comment: Cooling is not indicated for patients who are conscious after arrest.
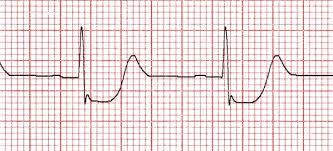
Case 4. 64 yo Patient presents with chest pain and subtle EKG suggesting posterior mi. Dia comment that with AVR showing subtle elevation and diffuse mild ST depression also consider LAD lesion. Harwood noted prolonged qt interval as well.
Posterior EKG showed very subtle st elevation in V7-9. There was no consensus in the audience about calling the STEMI based on these EKG’s.
Patient was managed medically. He went to cath 1-2 days later. Cath showed severe multi-vessel disease with LAD and marginal branch with 90% occlusions.
Silverman comment: This patient had very elevated blood pressure so there is a lot of room to medically manage this patient with nitrates and beta blockers and cool them down without emergent cath.
Cardiology comment: In the initial EKG the anterior t waves are inverted suggesting anterior ischemia rather than posterior mi which may have st depression with upright t waves.
*Anterior ischemia
*Posterior MI
Kadar/Putmann Oral Boards
Case 1. 26 yo female with abdominal pain for 5 days. Patient has fever and tachycardia. History reveals vaginal discharge. Only medication is an oral contraceptive. Physical exam demonstrates lower abdominal tenderness and CMT and vaginal discharge. Diagnosis is PID with a TOA. Critical actions: Get a pregnancy test, provide pain control, obtain cervical and vaginal specimens, get a pelvic ultrasound, start IV antibiotics (IV cefoxitin and IV doxycycline plus IV flagyl), Consult GYN.
Case 2. 2 year old child with fever and rash. Heart rate/pulse/respirations are normal. Dexi is 100. Rectal temp is 39. History reveals 5-6 days of fever and now has a diffuse erythematous rash. Review of systems is negative. Exam shows red cracked lips and bilat conjunctivitis. Patient has bilat hand swelling. There is cervical lymphadenopathy. Skin shows a diffuse erythematous rash. Diagnosis is Kawasaki’s disease. Critical actions are Starting ASA and IVIG. Order ECHO and consult ID or rheumatology. Rash can be very nonspecific. 20% of untreated patients will develop coronary artery aneurysms 2-6 weeks after illness. These aneurysms can lead to sudden cardiac death later in life.
*Kawasaki’s
Case 3. 3 year old with possible nasal FB. Vitals are normal. Airway is patent, no respiratory distress or choking. Mom states the child said he put something in his nose and has pain. Exam demonstrates FB in the left nostril. Critical actions: Remove FB with kissing technique (mom blows air into child’s mouth rapidly with non-affected nostril occluded) or forceps or balloon catheter technique.
McVicker (312-550-1941 You can text Tricia with any safety event)
Root Cause Analysis
No one goes into healthcare to hurt patients or break rules. If an error happens it is because our system broke down.
Root Cause Analysis is a structured process for identifying the causal or contributing factors underlying adverse events or other critical incidents.
Accidents in health care almost never stem from a single cause. They come from a mix of failures or work conditions that align precisely to slip through every existing defense.
*Swiss Cheese Model of Error
The goal of RCA’s is to learn from adverse events and prevent them from happening in the future. We talk about what happened and why it happened. Then we try to come up with a plan to prevent it from happening again.
Residents are very helpful to the RCA process because they know the micro processes of patient care.
ACMC does RCA’s when there is an event of unexpected death or severe harm to a patient. RCA makes safety a real priority and focuses on how the system failed. It does not focus on personal blame.
The RCA process is protected under the Illinois Review Act. It is not discoverable for malpractice cases.
The RCA process identifies the probable causes of an event, looks for reasons why they happened, and then identifies ways to prevent such an event from happening again.
During the RCA a timeline of events is developed. Then causal events (the why’s) are mapped out in a flow chart.
Cash M&M
“Failure is instructive” “We do not learn from experience…we learn from reflecting on our experiences.”
Case 1. 35 yo female with hyperglycemia and LLQ pain. Ct showed ureteral stone. UA showed blood and WBC’s. 18 hours later, patient was febrile and tachycardic. Creatinine had bumped to 2.58. Patient became hypotensive. IV antibiotics were started. Nephrostomy tube was placed. Patient later expired from sepsis.
Reflections: Take ownership of sign outs. They are truly your patients. Don’t slip into autopilot mode. Make sure that planned interventions are getting done.
Girzadas comment: Keep a lookout for these obstructed kidneys with any signs of infection (fever, wbc’s in the urine). There is urgency in getting these kidneys drained by IR with a nephrostomy tube.
Case 2. 30 yo female had left flank pain. UA shows leukocytes and blood. Ultrasound shows left renal hydronephrosis. Vitals show HR=108 and BP =106/72. Patient was discharged. 2 hours later the patient returns to the ER unresponsive. Vitals were 39.8C and hypotensive/tachycardic. At this point lactate is 7. IV Fluids, IV antibiotics were given and patient was intubated. An emergent nephrostomy tube was placed. Urine showed klebsiella. Patient improved and was discharged home.
Reflections: Pay attention to vital signs. Beware of communication failures between nurses and docs. Be vigilant with hallway patients and on busy shifts.
Harwood comment: The receiving sign out team has fresher brains and should be willing to re-evaluate the patient later during their shift.
Natalie Htet comment: Using ultrasound can show hydronephrosis in these patients but I have seen two patients who had some hydro seen on ultrasound come back to the ED and large ureteral stones were then identified on CT. Hydro on ultrasound does not give you much data on the size of stone or severity of obstruction.
Case 3. 65 yo female with abdominal pain and fever. Tachycardia and hypotension. Patient notes some dark urine. On exam patient has suprapubic tenderness and mild right CVA tenderness. Urine shows blood and leuks. Diagnosis is pyelonephritis. A Ct was performed. Patient had an obstructing stone in right ureter. Right nephrostomy drainage tube was placed. Urine culture shows Klebsiella.
There was a discussion concerning whether we should be doing ultrasounds or CT on pyelonephritis more frequently to rule out ureteral stone/obstructed kidney. Mila Felder suggested we review a series of cases to develop a more robust clinical pathway for pyelonephritis.
Sola comment: I have been burned on signouts that say “This patient is being discharged so we don’t need to talk about this patient” A patient planned for discharge started vomiting and needed further care and I knew nothing about the patient. Harwood comment: I even ask about the patients that died on the last shift. In case family later shows up.
Ede 5 Slide Follow Up
27 yo female with RLQ abdominal pain and syncope. UCG was positive. Pain radiated to right shoulder. Exam shows BP 107/74 HR=95. Minimal blood in vaginal vault. Cervix closed. UA shows large blood. HGB=11.6. Beta HCG= 67. U/S showed free fluid in RUQ. Patient was taken to the OR. A left tubal pregnancy was removed. The patient had a ruptured ectopic pregnancy with a Beta HCG of 67.
Risk factors for ectopic pregnancy: PID prior tubal surgery, IUD, assisted reproduction, and previous ectopic.
Triad of ectopic pregnancy: Abdominal pain, vaginal bleeding, and amenorrhea.
Findings suggestive of ectopic on U/S: free fluid, mass, no intrauterine pregnancy.
Beware of heterotopic pregnancy in patients who are undergoing assisted reproduction therapy.
Harwood comment: Ectopic pregnancies are reported/known to have low Beta HCG’s. So don’t let a low Beta HCG lull you into complacency.
Munoz 5 Slide F/U
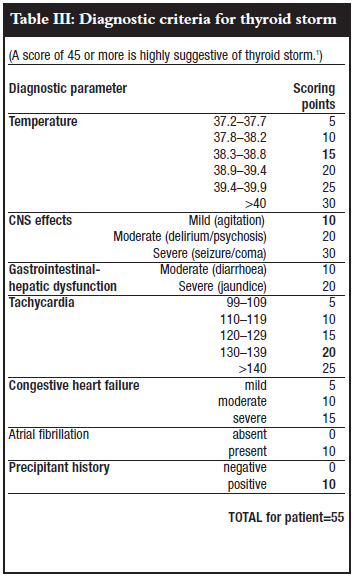
4 yo female with abdominal pain and lethargy. Patient had a history of Graves disease and is on propranolol. Child had been sleeping all day. Vitals show tachycardia and tachypnea. No fever. Child was lethargic on exam. Stool and emesis were heme positive. Labs significant for anion gap acidosis with an osmolal gap. ED docs considered toxic alcohol ingestion. Patient was admitted to PICU and eventually was diagnosed with thyroid storm. 7 days later the patient had thyroidectomy.
*Burch-Wartofsky Criteria
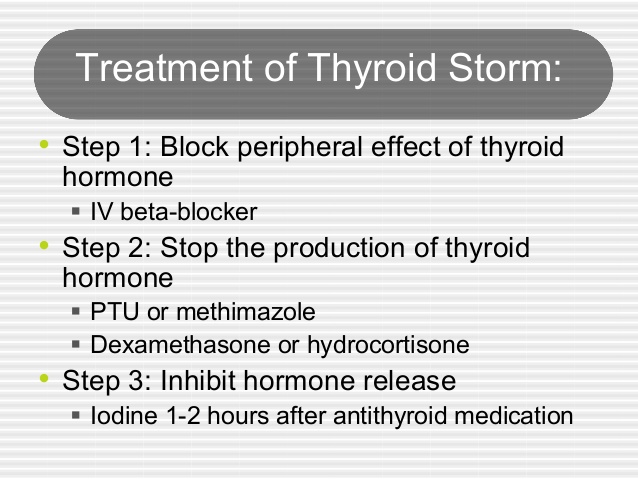
*Treatment for Thyroid Storm
Harwood comment: This seems like a case of apathetic thyroid storm in a child. This could be a case report material.