If you don't see images, please scroll to the bottom and click "Read in Browser"
Burns EKG Basics
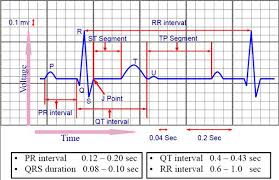
*EKG Intervals
Harwood comment: when determining the QRS interval, measure at the lead with the widest QRS.
General Approach to Evaluating an EKG
- Heart Rate
- QRS: wide or narrow?
- Rhythm: Regular or Irregular?
- P waves
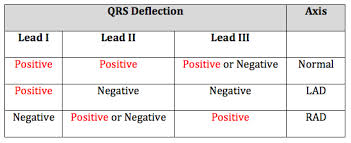
- Axis If the QRS is predominantly positive in I and II or AVF it is a normal axis
- ST changes
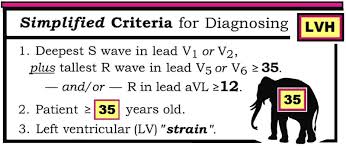
- LVH, QT interval
- Special signs (osborne wave, brugada sign, WPW)
*Rule to determine Axis
*Simplified LVH Criteria
Ianitelli Procedural Sedation
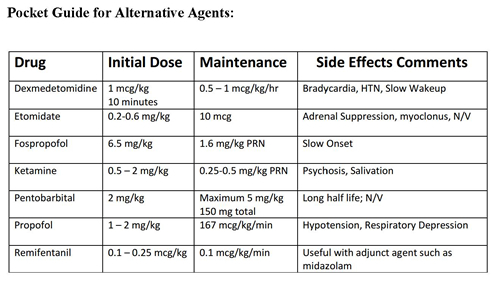
*Comparison of Common Sedation Agents
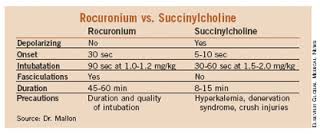
*Comparison of Succinylcholine with Rocuronium
Case 1. 19yo male with GSW to abdomen. Patient is hypotensive and tachycardic. Barounis comment: I would use low dose etomidate to avoid hypotension. Give a higher dose of succinylcholine due to poor perfusion of muscles in shock. Elise comment: I would use ketamine to avoid hypotension. Harwood comment: I would use reduced dose of etomidate.
Case 2. 32 yo female with altered mental status. Hypotensive, tachycardic, and febrile. O2 sat is 92% on RA.
Harwood and Girzadas comment: Delayed Sequence Intubation with ketamine. Pre-oxygenate then give succinylcholine to intubate. ED Pharmacist comment: Have push dose pressors ready for any hypotension that would develop.
Case 3. 72 yo female found down. Patient has right hemiplegia. Patient has been on the floor for at least 18 hours. BP is 100/60, Pulse of 70.
Consensus was using ketamine or low dose etomidate to avoid hypotension. Consensus was using rocuronium to avoid hypokalemia in a person with possible rhabdomyolysis/hyperkalemia/renal failure. Samir Patel comment: Succinylcholine is safe in chronic renal failure patients but be prepared to manage any hyperkalemia. In the setting of acute renal failure, rhabdomyolysis, or hyperkalemia, avoid succinylcholine.
*Contraindications to Succinylcholine
Case 4. 58 yo male with a Gluteal Abscess. Normal vital signs. Most people felt ketafol would be the optimal choice. Playing devil’s advocate, Kelly Williamson felt that using pain control and light sedation with fentanyl and versed could also work. The benefit of this approach would be to avoid procedural sedation and any complication of sedation.
Kennedy Use of Pressors
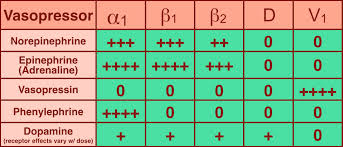
*Pressor Chart
Norepinepherine is your workhorse pressor. It is probably the first choice for most non-hemorrhagic shock situations.
Septic shock: first choice norepinephrine, second line is epinephrine or vasopressin
Anaphylactic shock: First choice is epinephrine, second line is vasopressin
Spinal Shock plus bradycardia: Epinephrine, second line is dopamine
Spinal Shock with normal rate: First choice is norepinephrine
Cardiogenic shock: First choice: Use a combination of dobutamine for inotropy with norepinephrine to reach a MAP of 65.
Pediatric Septic Shock (cold extremities) First choice is epinephrine, second line is dopamine
Pediatric Septic Shock (warm extremities) First choice is norepinephrine
Hypoplastic left heart syndrome with shock: First choice: Milrinone Second line: Dobutamine
Push dose pressors: Give during RSI in a hypotensive patient. Can also use in other clinical situation with expected rapid/short duration episode of hypotension
Epinepherine 1ml of cardiac epinephrine added to 9ml of saline in a syringe. You can give 1 ml of this diluted epinepherine every 2 minutes as needed for hypotension.
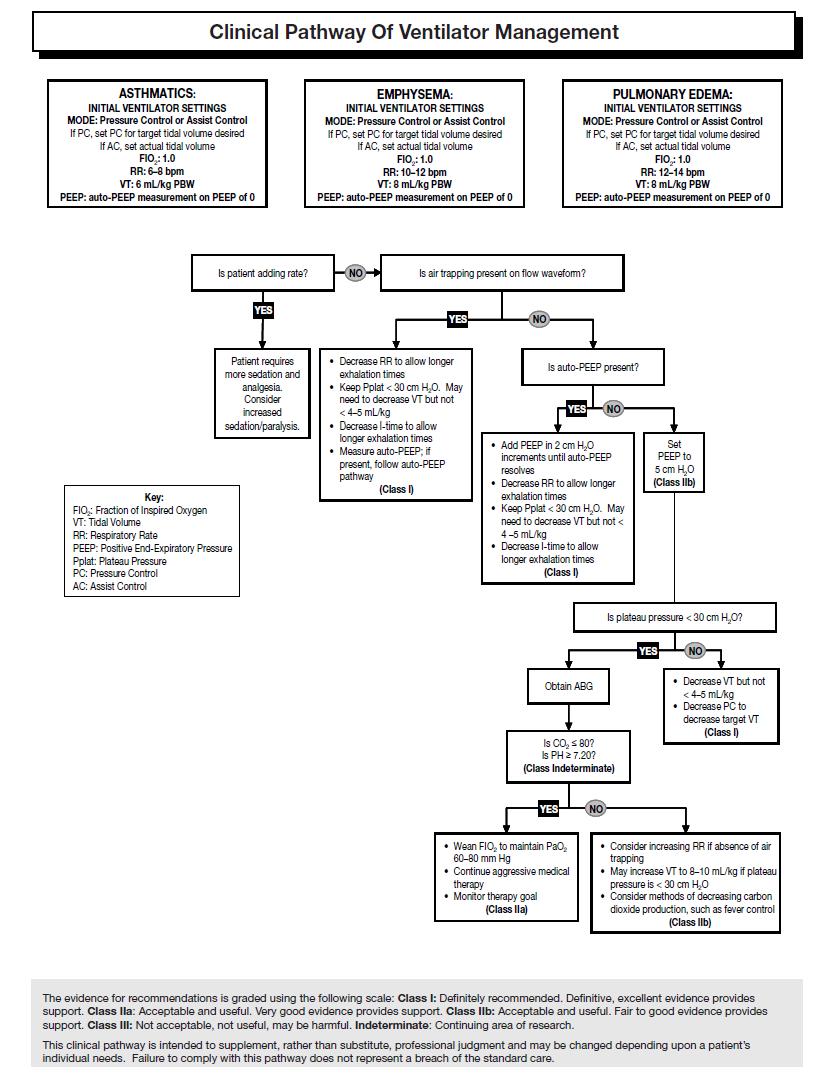
Myers Ventilator Management
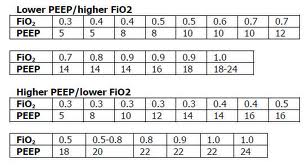
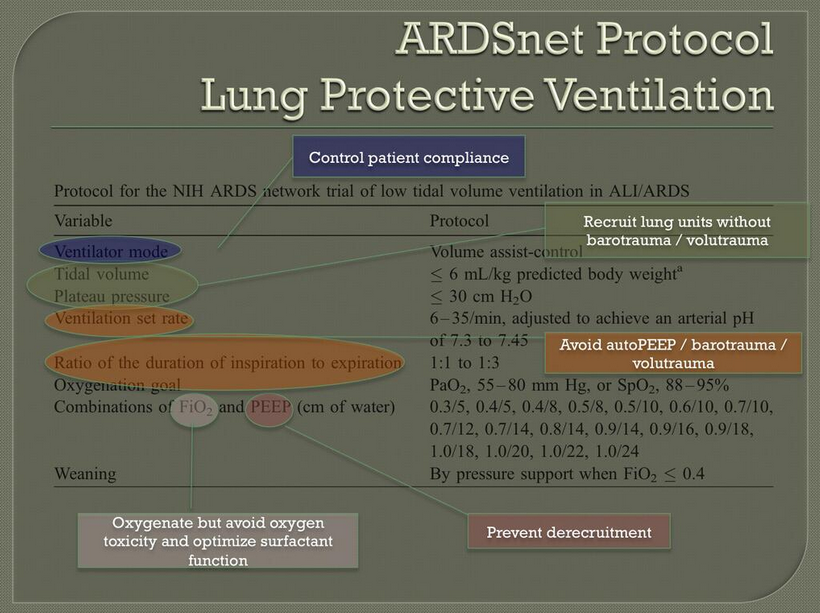
Ventilator management in the lung injured patient who doesn’t have asthma or COPD: Start on assist control. Keep volume low, tidal volume of 6 ml/kg of ideal body weight. Use the ventilator rate to provide appropriate ventilation. Don’t change tidal volume to adjust ventilation. 15 breaths per minute is a reasonable starting point. Start FIO2 at 100% and rapidly titrate down to FIO2 of 40% if possible to hit goal of O2 saturation >90%. You can also use PEEP to improve oxygenation. PEEP stents open alveoli to improve oxygenation. PEEP can negatively impact the patient’s preload resulting in hypotension. Keep plateau pressure less than 30. Plateau pressure is the measure of risk of barotrauma. It is a measure of the alveolar barostress.
*Suggested FIO2/PEEP Table
*ARDSnet Protocol
Obstructive Strategy (Asthma, COPD Ventilator Management):
Lower the patient’s respiratory rate to a rate of 10 or even 8. Increase expiratory time by setting the I:E ratio to 1:5. Permissive hypercapnea is OK. Keep ph >7.2 Set PEEP to 0.
*Obstructive Ventilator Strategy
In the crashing intubated asthmatic patient, your first move is to disconnect the ventilator. Then compress the chest manually to improve exhalation of air.
Htet Introduction to Codes
Have the same approach every time to every Code you manage.
Start with IV, O2, Monitor, Vitals, Dexi, EKG,
Get help from nurses and techs, respiratory therapist, and other physicians.
Proceed in your management based on the data you gather from these first two steps.
Case 1. 64 yo female who is unresponsive following an mvc.
Start with IV, O2, Monitor, Vitals, Dexi, EKG,
Get help from nurses and techs, respiratory therapist, and other physicians.
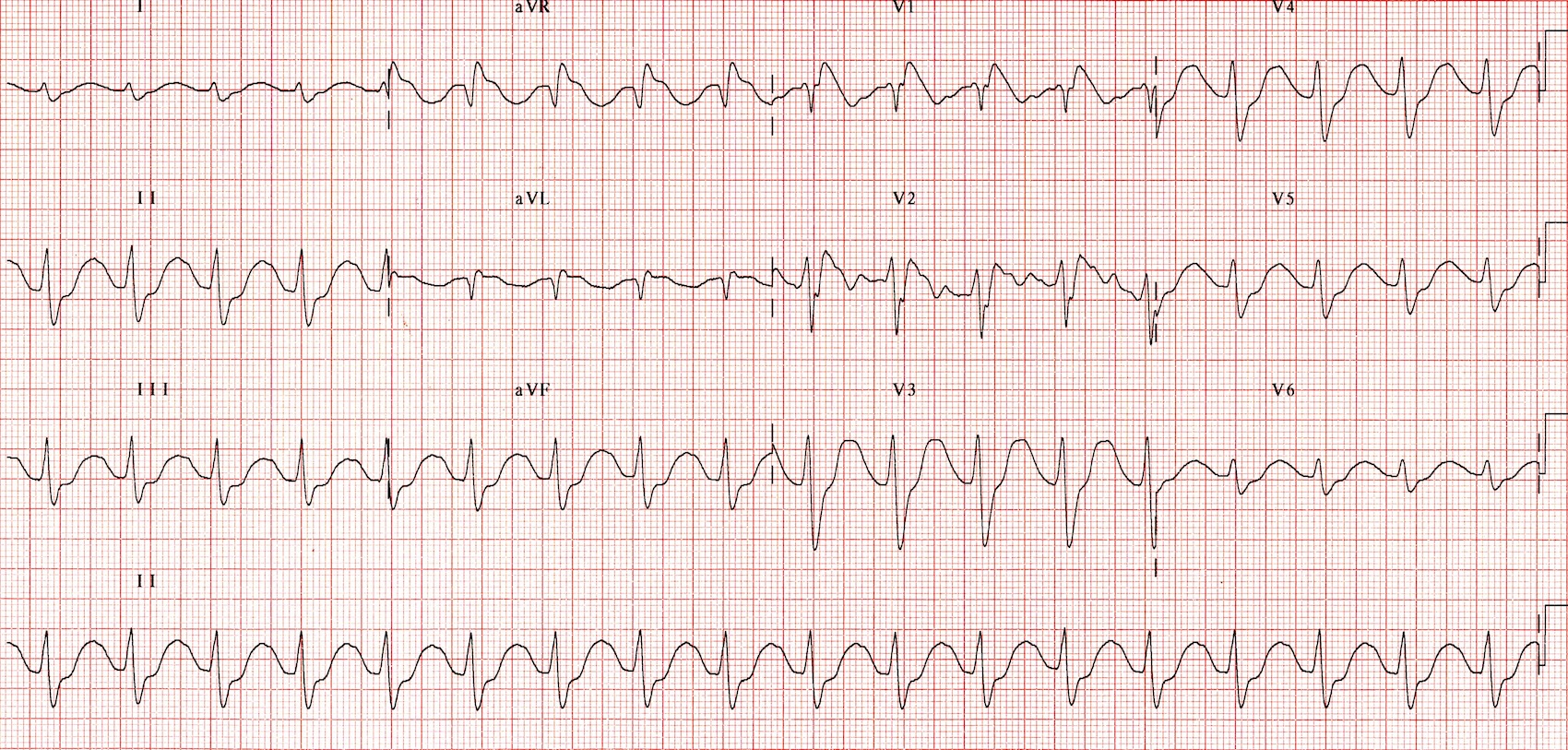
EKG shows TCA toxicity.
Consider intubation to potect airway
Give IV fluids
Consider pressors if hypotensive.
Give IV bicarbonate to narrow the QRS, and improve cardiac output and blood pressure.
*TCA EKG Note tall, wide terminal R wave in AVR and Wide QRS diffusely
Case 2. 65 yo female with fever and cough, hypotension and tachycardia.
Suspicion is septic shock.
Start with IV, O2, Monitor, Vitals, Dexi, EKG,
Get help from nurses and techs, respiratory therapist, and other physicians.
Intubate the patient considering the adjuncts of push dose pressors or delayed sequence intubation.
Give IV fluids, start antibiotics, give pressors if patient’s BP is not volume responsive.
Get appropriate labs including blood cultures and lactate.
Harwood comment: Bipap has been shown to decrease intubations but data demonstrating that it decreases mortality is difficult to find.
Case 3. 80 you female with sudden right hemiplegia.
Start with IV, O2, Monitor, Vitals, Dexi, EKG,
Get help from nurses and techs, respiratory therapist, and other physicians.
Get rapid CT of head
Identify last known normal neurologic function
Perform NIH stroke scale
Give TPA if indicated
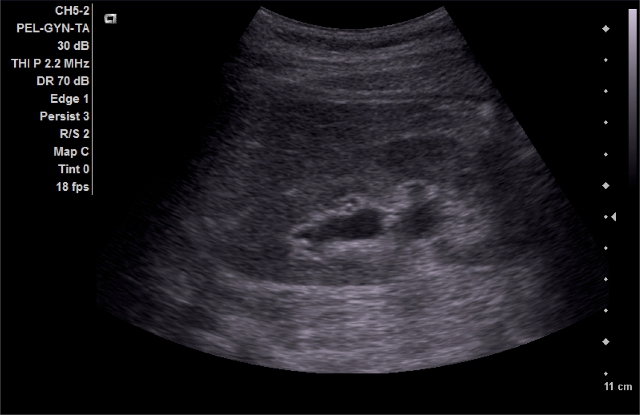
Samad Intro to Renal Ultrasonography
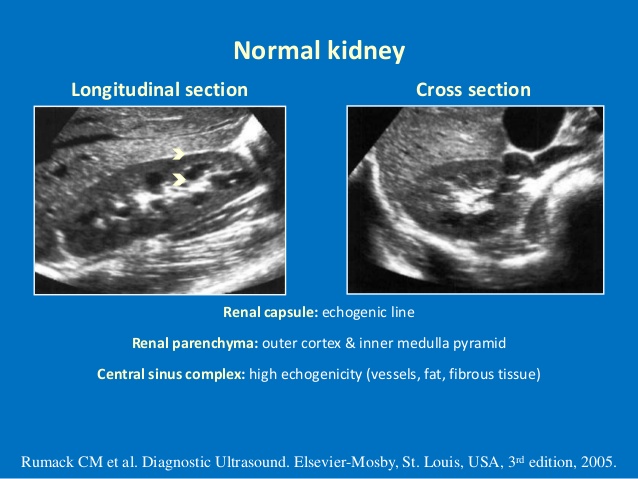
*Anatomy of Kidney on U/S
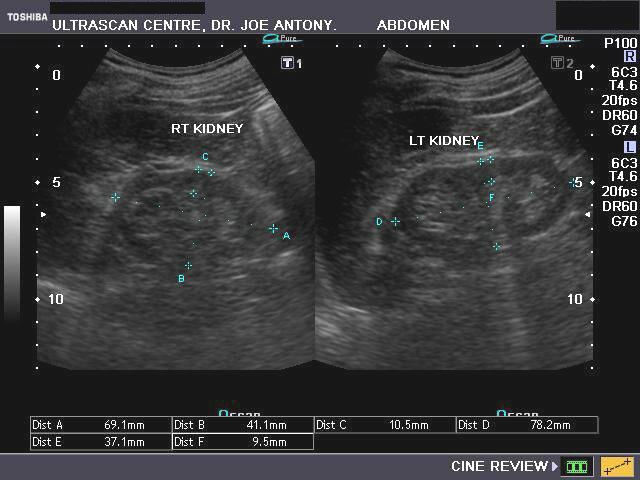
*Chronic Kidney Disease usually demonstrates smaller than normal kidneys, and decreased sonographic differentiation between cortex and medulla.
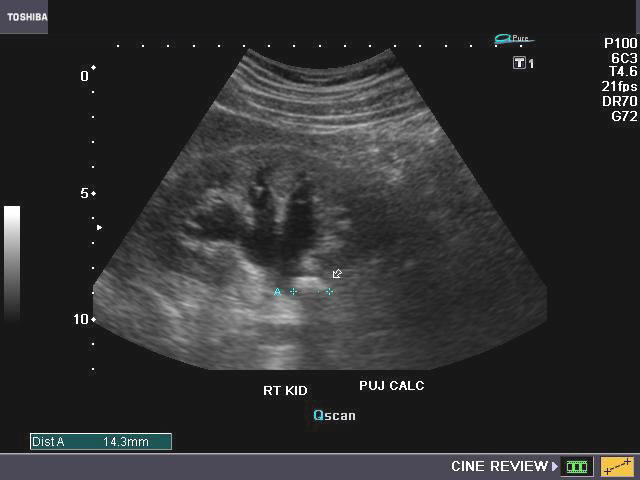
*Ureteral Pelvic Junction kidney stone
*Mild Hydronephrosis The key to identify mild hydronephrosis is seeing hypoechoic areas within the normally hyperechoic renal sinus.
CT is better than U/S for evaluating for pyelonephritis and it’s complications.
The first three differential diagnoses for enlarged kidney are: DM, multiple myeloma, and HIV nephropathy. The fourth is an infiltrative process like amyloidosis, lymphoma, or leukemia.
There was a discussion of a ureteral jet seen on ultrasound. A ureteral jet is a sudden rapid flow of urine from the ureter. If the ureteral jet is not seen, it suggests a significant ureteral obstruction. Elise comment: If you have a ureteral jet on one side and not the other it suggests a complete obstruction of the side without the ureteral jet. The finding of a unilateral absent ureteral jet may be a useful marker when trying to convince consultants to place a percutaneous nephrostomy in a patient with a suspect obstructed/infected kidney.
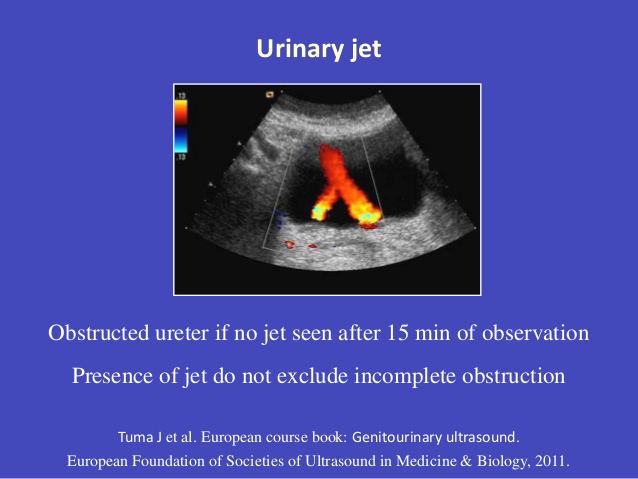
*Ureteral Jets on U/S using the Doppler U/S
Levine Understanding the Body’s Response to Traumatic Experiences
Sometimes the great care we strive to give patients in the ED can result in psychological trauma to those same patients despite our best efforts.
Psychological stress/trauma can result in real physiologic responses (fight or flight response)
Co-Regulation speaks to how caregivers can help a person experiencing emotional or psychological trauma cope with that event. We can control our tone, pace, and volume of our voice to calm and reassure patient. Gentle, appropriate touch and pleasant facial expressions can also calm and reassure the patient.
Physician strategies to diminish psychological trauma to the patient:
Allow family/friends to be with the patient
Educate patients about their diagnosis and what to expect both in the ED and when they go home.
Call Patients by their name and speak to them, not about them.
Remain calm and make a conscious effort to monitor your tone, volume, and rhythm of voice.
Use light touch on the arm, hand or shoulder to calm the patient.
Use verbal therapy. The following are a few examples: We are going to take care of you. We are going to make you feel better. You can say: I am here for you. We are going to get you through this. Life is really hard. You have been through some really tough stuff. Validate what patients are feeling and be careful to not undermine their thoughts, fears, or concerns.
Bonaguro Sepsis Update
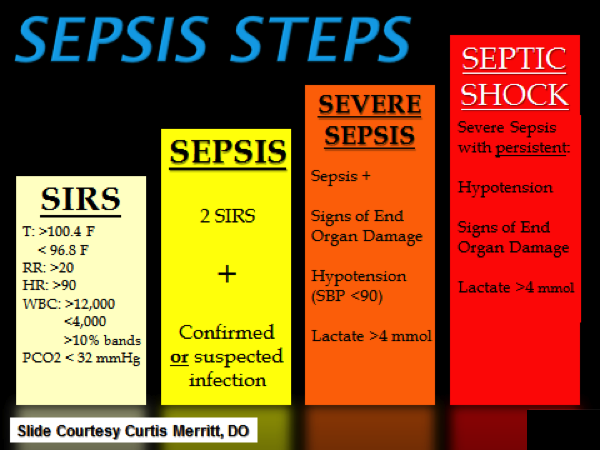
Sepsis continuum
When you suspect sepsis tell the nurse or SIMs that the patient is a Code Sepsis
Get an initial lactate and a 6-hour lactate
Septic Shock requires 30ml/kg crystalloid bolus. Give an initial 2 liter bolus instead of a 1 liter bolus. If you are worried about causing CHF give 2 liters in 500ml aliquots and frequently re-assess the patient.
Do a 6 hour re-exam including vital signs, cardiopulmonary exam, cap refill exam, pulse evaluation and skin exam. OR Do a bedside cardiac ultrasound and passive leg raise test. OR Place a central line and get a CVP.
You must write your sepsis H&P note within 6 hours of the patient’s ED arrival.
An EMR fix for these new requirements is the “ED Sepsis Advisor Power Plan”
This is a more advanced power plan in FirstNet than the ED Sepsis Power Plan. The Sepsis Advisor Power Plan has most of the above testing and documentation requirements built in.