Lee/Felder Oral Boards
1. 33yo female had a seizure. Patient is post-partum. Vitals: HR=118, BP=95/60 otherwise normal. Patient gave history of peri-partum hemorrhage followed by difficulty with breast feeding over the last 2-3 weeks. Labs show sodium of 113 and potassium of 6.2. Patient also had signs of UTI. Concern was raised foradrenal insufficiency and stress dose steroids were given. Diagnosis is Sheehan’s syndrome.
*Sheehan’s syndrome
Be alert for associated hypothyroidism due to lack of TSH. Treatment for this case included Normal Saline if patient is no longer seizing. Mark Pharm D comment: If patient is still seizing give hypertonic saline 30ml/hour. Goal is to raise the serum sodium level by 12 in 24 hours.
Christine comment: I like this idea from Emcrit http://emcrit.org/podcasts/hyponatremia/
Basically for the seizing hyponatremic patient, give 100 ml of hypertonic over 10-60 min, then re-evaulate. Should be ok for 50 kg or larger adult. And bonus for me, easy to remember.
Give hydrocortisone 100mg Q8 hours.
2. 10mo male noted by parent to have had a seizure in the crib. Seizure lasted less than 5 minutes. No Fever. No one else is ill in the home. No PMH. On exam, the child is playful. On further history, the babysitter noted that child had fallen out of car seat earlier on the day of ED visit. A head CT and skeletal survey were ordered. Imaging shows a skull fracture. The skeletal survey shows a metaphyseal chip fracture and old rib fractures.
*Metaphyseal chip fracture
Diagnosis was seizure secondary to non-accidental head injury. DCFS was notified and child was admitted to ICU. This case illustrates the need to always be alert to the possibility of non-accidental trauma.
3. 68yo female transferred from the NH with ongoing seizure. HR= 120, BP=130/80, Pulse OX=98%, Dexi=25. It was learned through discussion with NH that patient accidentally received long-acting insulin instead of lovenox. Patient was given IV dextrose followed by D10NS drip to prevent further hypoglycemia.
Be aware of adverse drug events in patients coming from a nursing home.
Check blood sugar in every patient who seizes and every patient who cannot speak normally with you.
Elise comment: If a patient who is seizing does not respond to initial Ativan, you have to start thinking about more uncommon causes of seizures such as hyponatremia, INH toxicity, hypoglycemia, hypocalcemia.
PharmD comment: When treating severe hyponatremia you can go up by 12 meq over 24 hours.
Harwood comment: For Sheehan’s you need to test for and treat adrenal insufficiency and hypothyroidism. For the boards, verbalize your assessment of the problem and your plan of management so the examiner can accurately evaluate your medical knowledge. In my experience, the NH will never admit to a drug error. If you suspect accidental insulin administration, you can order an insulin level. A high level will indicate exogenous insulin in the patient.
Den Ouden The Force Awakens/Thoughts on Being an Emergency Physician
1. We have an impossible job. You have to accept the fact that you can’t meet all the demands placed on you.
2. Patient satisfaction is a trickytask. A UC Davis study showed a 26% higher mortality rate in the most satisfied patients.
The Cost of SatisfactionA National Study of Patient Satisfaction, Health Care Utilization, Expenditures, and Mortality FREE
Joshua J. Fenton, MD, MPH; Anthony F. Jerant, MD; Klea D. Bertakis, MD, MPH; Peter Franks, MD
Arch Intern Med. 2012;172(5):405-411. doi:10.1001/archinternmed.2011.1662.
Text Size:
Background Patient satisfaction is a widely used health care quality metric. However, the relationship between patient satisfaction and health care utilization, expenditures, and outcomes remains ill defined.
Methods We conducted a prospective cohort study of adult respondents (N = 51 946) to the 2000 through 2007 national Medical Expenditure Panel Survey, including 2 years of panel data for each patient and mortality follow-up data through December 31, 2006, for the 2000 through 2005 subsample (n = 36 428). Year 1 patient satisfaction was assessed using 5 items from the Consumer Assessment of Health Plans Survey. We estimated the adjusted associations between year 1 patient satisfaction and year 2 health care utilization (any emergency department visits and any inpatient admissions), year 2 health care expenditures (total and for prescription drugs), and mortality during a mean follow-up duration of 3.9 years.
Results Adjusting for sociodemographics, insurance status, availability of a usual source of care, chronic disease burden, health status, and year 1 utilization and expenditures, respondents in the highest patient satisfaction quartile (relative to the lowest patient satisfaction quartile) had lower odds of any emergency department visit (adjusted odds ratio [aOR], 0.92; 95% CI, 0.84-1.00), higher odds of any inpatient admission (aOR, 1.12; 95% CI, 1.02-1.23), 8.8% (95% CI, 1.6%-16.6%) greater total expenditures, 9.1% (95% CI, 2.3%-16.4%) greater prescription drug expenditures, and higher mortality (adjusted hazard ratio, 1.26; 95% CI, 1.05-1.53).
Conclusion In a nationally representative sample, higher patient satisfaction was associated with less emergency department use but with greater inpatient use, higher overall health care and prescription drug expenditures, and increased mortality.
3. What scares EM docs? Lawsuits, Peds emergencies, big misses, difficult airways.
4. Make a human contact with patient and family. Shake their hand. Make eye contact. Find out their fears. A good emergency physician is like being a waiter. You have to guide patients thru the system and keep them updated.
5. Repeat your plan of care multiple times to the patient. Make a verbal contract with the patient.
6. Tell patients you want to make them feel better. Tell patients you will rule out anything emergent.
7. You have to do some “doctoring” that is reassuring the patient, review the “extensive” testing you did in the ED, express a caring nature to patients.
8. Everyone has bouncebacks.
9. Tools to screen for aortic dissection: HX of migratory pain and uncontrolled hypertension, bilateral blood pressure, CXR, d-dimer (imperfect test, you can’t document that you used it to screen for dissection), CTA. CTPE will find dissections as well.
*Adam Bonder’s Reference: AHA Algorithm for working up Aortic Dissection
*Harwood’s Reference for using d-dimer for screening for aortic dissection. This applies to low risk patients in the above algorithm
D-Dimer as a Test for Aortic Dissection: Relevant or Not?
Daniel J. Pallin, MD, MPH reviewing Asha SE and Miers JW Ann Emerg Med 2015 Mar 24.
A meta-analysis finds that a low D-dimer level excludes aortic dissection but only in low-risk patients, who might not be tested anyway.
Previous studies have shown that d-dimer levels tend to be high in the presence of aortic dissection and low in its absence. But is d-dimer testing sufficiently sensitive to contribute to clinical decision making? To find out, investigators conducted a meta-analysis to assess the negative predictive value of a normal d-dimer result among patients evaluated for aortic dissection. They analyzed the results according to pretest risk determined by an American Heart Association risk score. The score designates a patient as low risk if there are no high risk findings, which range from Marfan syndrome to new aortic insufficiency murmur, but, importantly, include chest, back, or abdominal pain of abrupt onset, severe intensity, and ripping or tearing quality. The pre-test probability (prevalence) of aortic dissection in low-risk patients is 6%.
In pooled analysis of data from four studies including 1557 patients, a d-dimer level <0.5 µg/mL had a sensitivity of 98% and a negative likelihood ratio of 0.05 to rule out aortic dissection. For non–low-risk patients, the authors concluded that d-dimer testing was not sufficiently sensitive to rule out aortic dissection and should not be used.
10. Simple epinepherine drip for anaphylactic shock: Put 1 mg of cardiac epinepherine in 1 liter of NS. Give 1 drop per second thru an antecubital IV. You can titrate up as needed. You can do this with any pressor, 1 mg in 1 liter of saline gives you a 1mcg/ml solution.
11. Win your patients over. Make human contact with the patient and their families. Set the expectations of the ED visit.
Htet Jeopardy
Boutoniere and swan neck deformities are seen with rheumatoid arthritis.
*boutoniere and swan neck deformities, mallet finger is also pictured. Mallet finger is due to trauma.
*monteggia vs galeazzi fracture
*Kanavel’s cardinal signs
The incidence of appendicitis during pregnancy is the same as in non-pregnant patients. The incidence of perforation during pregnancy is increased however.
Harwood comment: The location of the appendix does not change during pregnancy. It is an urban myth that the appendix rotates up to the RUQ during pregnancy.
Rocky Mountain Spotted Fever is treated with doxycycline in adults and kids. Even though we traditionally don’t use doxy for kids, RMSF has high enough mortality that doxy is recommended even for kids. There was debate about the best antibiotic choice for a pregnant patient with RMSF.
CDC Reference:
The use of doxycycline to treat suspected RMSF in children is standard practice recommended by both CDC and the AAP Committee on Infectious Diseases. Use of antibiotics other than doxycycline increases the risk of patient death. Unlike older tetracyclines, the recommended dose and duration of medication needed to treat RMSF has not been shown to cause staining of permanent teeth, even when five courses are given before the age of eight. Healthcare providers should use doxycycline as the first-line treatment for suspected Rocky Mountain spotted fever in patients of all ages.
Other Treatments
In cases of life threatening allergies to doxycycline and in some pregnant patients for whom the clinical course of RMSF appears mild, chloramphenicol may be considered as an alternative antibiotic. Oral forumulations of chloramphenicol are not available in the United States, and use of this drug carries the potential for other adverse risks, such as aplastic anemia and Grey baby syndrome. Furthermore, the risk for fatal outcome is elevated in patients who are treated with chloramphenicol compared to those treated with doxycycline. Other antibiotics, including broad spectrum antibiotics are not effective against R. rickettsii, and the use of sulfa drugs may worsen infection.
Harwood comment: I would give a pregnant patient with RMSF an initial dose of IV erythromycin and consult ID and the CDC. There is no great answer in this very difficult situation.
*Centor Criteria. There was debate among faculty whether to perform a rapid strep test on the patients with 4 criteria or just treat them.
*Commotio cordis occurs when the pediatric chest is struck with a blunt object at just the wrong time during the QRS cycle to cause V-Fib. It has to do with the potassium channel currents.
Button battery ingestions are high stakes situations. If the button battery is in the esophagus it needs to be removed emergently. If it is in any other area of the GI tract, it probably can be watched to see if it passes. On xray you can identify if the object is a battery by looking for a circumferential crimp (double ring or Halo sign).
*Button battery on xray vs. coin on xray. Note the button battery has a double ring or Halo sign.
*Elise reference on the management of button battery ingestion
Kadar Critical CareM&M
Consider using a lower dose of sedation and a higher dose of paralytic when intubating the unstable patient. For example 10mg of etomidate and 1.5 mg/kg of succinylcholine. Harwood comment: I would never go past 2mg/kg of succinylcholine. Mark our PharmD said high doses (>2mg/kg) of succinylcholine can cause bradyarrythmias. Very high doses of rocuronium can cause tachyarrythmias.
Harwood comment: Consider using ketamine and topical lidocaine for an awake intubation/sedated intubation in the unstable patient. It is preferred to intubate in the ED versus other areas of the hospital. We have more resources at hand in the ED.
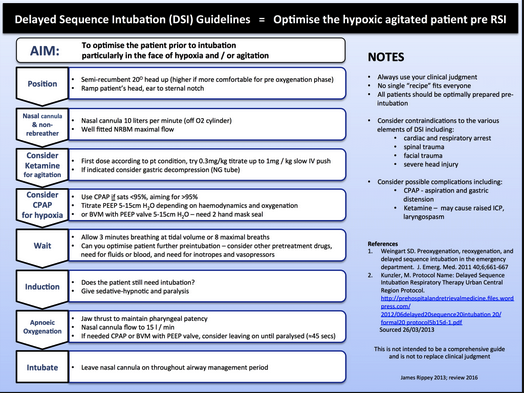
*Delayed Sequence Intubation
*Awake intubation. Rachel made the point that you could safely use both nebulized lidocaine and atomized lidocaine to anesthetize the throat. If you don’t have atomized lidocaine, you can use nebulized lidocaine and viscous lidocaine.
*3-3-2 rule
Cirone Physical Restraints in the ED
Restraint must be considered a last resort in the setting of the patient being at risk of harming themselves or others.
It is wrong to use physical restraints to prevent a patient from leaving the ED, punish them, or maintain an orderly environment.
Within 1 hour of initiating any physical restraint, the physician must evaluate the patient with a face-to-face clinical exam and document it on the correct form or in the medical record using an appropriate template.
Physical restraint has risk of aspiration, injury, and death for the patient. It also puts medical staff at risk of injury.