Conference Notes 10-5-2016
Chastain/West Oral Boards
Case 1. Child with anaphylaxis. Patient has angioedema of lips/pharynx and signs of shock. Initial treatment with IM epinephrine, IV steroids, IV Benadryl, IV Pepcid. Epinephrine drip was started after initial IM epinepherine. It is ok to give repeated doses of IM epinepherine before moving to IV epinephrine. Steroids/Benadryl/Pepcid/ nebulizer treatments are second line therapies in anaphylaxis. First line/life-saving treatment for anaphylaxis is epinephrine. Epinepherine dosing in kids is 0.01mg/kg. This can be difficult to measure out appropriately. Easy dosing for kids is to use the EPIpen junior (0.15mg of 1:1000) IM for kids less than 30kg.
Delay in epinephrine for anaphylaxis increases mortality. The rapidity of onset of anaphylaxis predicts the severity. Most fatalities occur in the first hour.
Elise comment: EPIpens are the way to treat anaphylaxis. It greatly simplifies the dosing. Patients weighing less than 30kg get EPIpen junior. You can redose the patient every 15 minutes if needed.
Case 2. 55 yo male brought in by EMS after being rescued from a house fire. Patient has soot on his face and body. Patient has cough and sore throat. Exam of the oro-pharynx demonstrates soot and carbonaceous sputum. Patient was tested for CO poisoning. Labs did not indicated severe acidosis making cyanide poisonin unlikely. During ED course, patient developed increased dyspnea, throat pain, and stridor. Patient was intubated early to avoid airway obstruction. Patient was also treated with 100% FIO2 for CO poisoning.
Harwood and Elise both felt this patient needed to be treated with hyperbaric O2 even though he was intubated and receiving 100% FIO2.
There were some questions about the mechanism of how hyperbaric oxygen works. This is an exerpt from a Medscape article:
Most oxygen carried in the blood is bound to hemoglobin, which is 97% saturated at standard pressure. Some oxygen, however, is carried in solution, and this portion is increased under hyperbaric conditions due to Henry's law. Tissues at rest extract 5-6 mL of oxygen per deciliter of blood, assuming normal perfusion. Administering 100% oxygen at normobaric pressure increases the amount of oxygen dissolved in the blood to 1.5 mL/dL; at 3 atmospheres, the dissolved-oxygen content is approximately 6 mL/dL, which is more than enough to meet resting cellular requirements without any contribution from hemoglobin. Because the oxygen is in solution, it can reach areas where red blood cells may not be able to pass and can also provide tissue oxygenation in the setting of impaired hemoglobin concentration or function.
Basically hyperbaric oxygen increases the amount of oxygen dissolved in the serum. This increased oxygen can then diffuse further into tissue than normobaric oxygen.
Michelle comment: Be aggressive with prophylactic intubation in patients with signs ofinhalation injury. Inhlation injury is the main cause of fire-related deaths. It is associated with patients being in a closed space fire.
Case 3. 19yo male with difficulty breathing. Patient developed left chest pain while lifting weights. Chest x-ray showed pneumothorax. Patient was treated with chest tube. Spontaneous pneumothoraces can be treated with mini-chest tube (pneumothorax kit).
*Pneumothorax Look for the pleural reflection. Dr. Asokan’s tip: look in the spaces between the ribs for lung markings.
Muhammad Neonatal Resuscitation
Normals
1) Periodic breathing is normal-looks like rapid breathing followed by pause of about 10 s. Apnea requires 20s pause and should be associated with cyanosis or bradycardia
2) HR 100-220 normal. BP MAP > gestational age. Temp should be between 36.5 and 38 or sepsis eval required.
3) Weight loss of up to 10%V in first week normal. Should be back at birth weight at 2 wk. Double breath weight at 6 months. Should be fed about 1 oz/hr. Constipation is defined by consistency of stools not frequency. About 8 wet diapers or more in 24 hrs.
Case 1- g1p0 at 25 y/o presents in labor. How do you prepare?
1) History- term (plastic wrap for pre-term)? Maternal risk factors? How many babies? Fluid clear?
2) Basics- Dry, stimulate, warm (radiant warmer). Three Questions- Term? Good tone? Breathing or crying? If yes, no resuscitation. Apgars at 1 and 5 min
One minute to treat if ventilation compromised.
ABCs
A- suction only if needed (changed from previous). If you do suction, mouth before nose. Avoid deep suctioning
B- assess effort, apnea, bradypnea, gasping
C- auscultate for HR (vs palpate base of umbilicus)
Use PPV if apnea after 30s, gasping, or HR < 100 (usually secondary to respiratory problem)
Use either flow inflating bag (control pressure manually, set at 10-20, more for pre-term) or T-piece resuscitator (set pressures)
Sniffing position with shoulder roll.
Start at room air O2 (21%), and titrate up if needed.
Chest compressions if no response to 30 s of PPV and HR < 60. Use 2 thumb technique. Compress 1.3 diameter of chest. 1 & 2 & 3 & breathe & 1 & 2 & 3 & breathe. Intubate or LMA at this point.
Term babies ETT 3.5 with Miller size 1. Pre-term 3, Miller 0. Insert ETT to depth of 3x tube size.
Should place UVC if no IV access, low lying UVC- only until you get blood flash. You can catheterize UVC up to 1 wk post-partum.
Umbilical line technique-
Pick the big, floppy one. 3.5 F catheter. Sterilize, stabilize with umbilical tape. Cut to 1-2 cm above skin surface. Clear thrombus if present. Place catheter about 4 cm, until blood return
Doses-
Epi- 0.1 mg/ml
Naloxone 0.1 mg/kg
dextrose 5 ml/kg of D10
NS 10 ml/kg
pRBCs 10 ml/kg
Special Considerations- Meconium
1) If vigorous, do nothing.
2) If not vigorous, its complicated. No longer emphasize intubation and aspiration (no proven benefit) although it is still IIB recommendation by AAP
Discontinuing resuscitation- Justified in stopping at 10 min if no signs of life.
Neonatal HPI-
Pregnancy and delivery- infection, GBS status.
Gestational age, d/c with mom? Birth weight?
Meconium passed, feeding, eliminating, issues with feeds?
Case 2. 15 do infant presents with seizure. Any infant less than 60 days with a seizure needs a big time work up including CT and labs. If CT and labs don’t give you a cause of the seizure, you need to proceed with LP. Test CSF for bacterial infection and HSV.
Child has another seizure in the ED. Check blood glucose. Treat hypoglycemia with 5ml/kg of D10. Place an IO for access to give benzo’s. Alternatively, you can give rectal valium, IM midazolam, IN midazolam.
* Elise Reference on IM Midazolam: Shorter duration of seizure, fewer patients seizing on arrival to the ED
Check the sodium level. This is a common electrolyte abnormality in neonates.
If child is still seizing, give phosphenytoin or keppra IV.
Sodium comes back 120. You need to treat with 3%hypertonic saline (3ml/kg). Remember 3 and 3= 3ml/kg of 3%hypertonic saline.
Think inborn errors of metabolism if hypoglycemia,metabolic acidosis, or elevated ammonia level is present.
You unfortunately have to consider non-accidental trauma in the seizing infant.
Case 3. 5 do infant presents with lethargy and poor peripheral pulses/delayed capillary refill. Heart rate is 200. Order prostaglandin immediately.
Get access with UVC or IO. Start IV fluid bolus and antibiotics.
You have to consider coarctation of aorta. These kids can get shocky after ductal closure. PGE (0.1mcg/kg/min) will open the ductus. PGE however can cause apnea. So you need to be prepared to intubate if necessary. If you need to transfer an infant who is receiving PGE you should consider intubating prophylactically prior to transport.
Case 4. 4 do male vomiting. Emesis is green. You have to think malrotation with volvulus in any infant that has bilious emesis. Consult surgery emergently. Start IV fluids and antibiotics. Start with plain abdominal x-ray but patient will need upper GI study.
*Malrotation with volvulus
*Another malrotation with volvulus
Plain xrays may be non-specific, you will need to consult surgery and get upper GI study.
Hart/Regan Ortho Cases of the Week
*SCFE More commonly affects boys 13-16 yo. Patients may have hip or knee pain. Get AP pelvis to compare both hips. Treat with non-weight bearing and operative repair.
*Jones fractureIs a fracture at the metaphyseal/diaphyseal junction of the 5th MT. It will be at the level of the inter-metatarsal joint.
*Pseudo-Jones fracture.
Jones fractures are prone to non-union. Pseudo-Jones or dancer’s fracture is due to avulsion injury. Jones fracture needs short leg post-mold and crutches. Avulsion injuries can be treated with ace wrap and post op shoe.
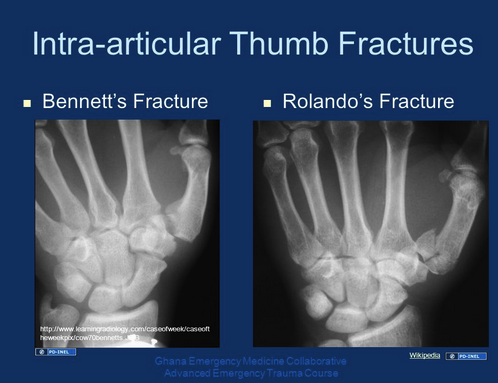
*Bennett fracture vs Rolando Fracture Treatment is thumb spica splint and operative repair. Benett has 2 syllables in the name and parts to the fracture. Rolando has 3 syllables in the name and 3 or more parts to the fracture.
*Maisonneuve fracture If you see a medial malleolus fracture, check the proximal fibula for tenderness. Keep your guard up for a maisonneuve fracture or a syndesmosis tear.
Ortho Lab