Barounis Coma
The most important thing in this lecture is finding brainstem signs in the comatose patient.
Start with a good history. Look for prodromal symptoms such as headache, vomiting, fever, syncope, depression. Then try to find out the rapidity of onset of coma. Find out the patients baseline function.
Evaluate the motor response to pain. If the patient localizes to pain that is a positive response. If no response or posturing then look for brainstem signs. Basically check the pupils.
Miosis=opioids, pontine hemorrhage,
Fixed mid sized pupils=mid brain lesion or brain death
Unilateral fixed dilated pupil=uncal herniation from a mass, bleed, or aneurysm
Bilat fixed dilated pupils=almost always due to a medication, atropine during a code can do it.
Bilat small reactive pupils= non specific, can be due to metabolic disease like sepsis.
Anisocria + sudden coma is basilar artery stroke
Eyes deviate to side of stroke in the brain. Logan Traylor’s mnemonic (you can’t look away from the train wreck)
Eyes deviate away from irritation in the brain such as seizureLogan Traylor’s mnemonic (the seizure is irritating so you look away)
So,
If gaze is looking to opposite side of hemiparesis (weak arm or leg)= stroke
If gaze looks toward hemiparesis (weak arm or leg)= seizure
Skew (eyes not aligned completely up and down) is another sign of brainstem lesion
Vertical nystagmus is a sign of brainstem lesion
Anisocria, skew deviation, lateral deviation, vertical nystagmus are signs of brainstem cause of stroke.
Cheyne stokes breathing is another sign elevated ICP or brainstem lesion
If a patient has anisocoria or skew deviation they need a CTA to identify need for embolectomy.
Dave described a case in a middle age man who presented with acute coma. He had anisocoria on exam.
If the patient has no abnormal eye findings and has a gag or cough reflex then the problem is in the cortex.
*Algorithm for the evaluation of Coma (emcrit)
*Four score is better than GCS because it forces you to look at the eyes.
Dave made the point that if you have a febrile comatose patient, you very strongly need to consider doing an LP. The LP can be therapeutic in these patients because it may lower the ICP and improved cerebral perfusion pressure.
*Neurocritical Care for Comatose Meningitis patients.
*PRES
Posterior reversible encephalopathy syndrome (PRES) is a neurotoxic state that occurs secondary to the inability of posterior circulation to autoregulate in response to acute changes in blood pressure. Hyperperfusion with resultant disruption of the blood brain barrier results in vasogenic oedema, but not infarction, most commonly in the parieto-occipital regions.
Terminology
PRES is also known as hypertensive encephalopathy or reversible posterior leukoencephalopathy.
The term PRES can be a misnomer as the syndrome can involve or extend beyond the posterior cerebrum. Furthermore, although most cases involve a resolution of changes with the treatment of the precipitating cause and clinical recovery some patients can progress to develop permanent cerebral injury and be left with residual neurological defects. (Radiopaedia)
Marynowski/Holland Oral Boards
Case 1. Patient presents with massive GI bleeding from aorto-enteric fistula. Treat with 2 large bore IV’s. Transfuse immediately with uncrossmatched blood. Intubate. Place NG tube to suction. Give antibiotics for infected aortic graft. Get patient to surgery emergently.
Elise comment: With massive bleeding always initiate the massive transfusion protocol.
Case 2. Patient presents with rash and pre-syncope. Diagnosis is Lyme’s disease with heart block. Treat with appropriate antibiotic. Doxycycline, amoxicillin, cefuroxime, ceftriaxone are all OK for treatment of lyme disease. Elise comment: For heart block IV ceftriaxone is recommended by IDSA guidelines. Perform or consult for pacemaker. 1 study noted that 38% of patients required a temporary pacemaker.
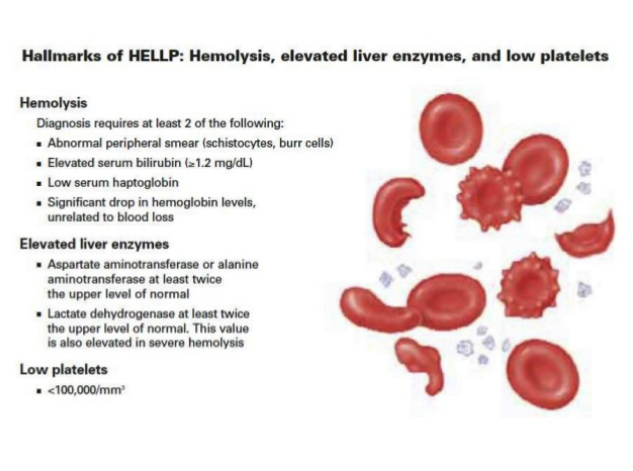
Case 3. 34 week pregnant patient with nausea, vomiting, and abdominal pain. BP is 142/94. Patient has laboratory findings consistent with HELLP syndrome.
*HELLP syndrome
Treat with magnesium and treat hypertension. If the infant is <34 weeks give the mom steroids prior to delivery to promote fetal lung maturation.
Greenberg Tachyarrhythmias in Adults
*Antiarrythmic Categories
For Afib there is no mortality difference between rate control and rhythm control. Rate control is easier so that method is favored.
First lines drugs for Afib with RVR are Cardizem or metoprolol/esmolol.
Amiodarone can have both rate and rhythm benefits in Afib. Amio can take more than an hour to have an effect.
Digoxin can be given in a loading dose to control the rate in Afib. It starts to work in about an hour. Make sure you correct any potassium abnormalities to avoid arrhythmias.
For stable VT the PROCAMIO study showed better efficacy and less adverse reactions for procainamide compared to amiodarone. Unfortunately procainamide is not available until 4th quarter of 2018 due to limited production.
If VT is refractory to amiodarone, second line is lidocaine, followed by third line phenytoin.
Treat polymorphic VT with magnesium first line or defibrillation. If the QT is not prolonged you can cautiously try a beta blocker or amiodarone. Consult cardiology.
For shock refractory V-fib (electrical storm) , give amiodarone. If V-fib still refractory consider esmolol and double defibrillator defibrillation. There is case report and small study data showing some benefit.
Nejak Supplemental O2
I missed this excellent lecture.
Pediatrics Faculty Member Bronchiolitis
Don’t order a viral panel or rapid RSV testing. It is painful to the child and there is no benefit.
Don’t use albuterol or epinephrine, or hypertonic saline nebs. The Peds EM faculty felt you could trial an albuterol MDI and check for improvement. The MDI takes out the humidified oxygen that is delivered by a neb and gives you a cleaner test of whether albuterol is helping or not.
No steroids.
Supplemental oxygen if needed.
Nasal suctioning is good. Deep suctioning is bad.
No CXR unless child is going to ICU or you have concern for pneumothorax.
Febrile infants under 90 days of age with bronchiolitis have a low risk of concomitant meningitis. LP may not be needed in infants over 30 days. Under 30 days you should still do an LP in febrile infants with bronchiolitis.
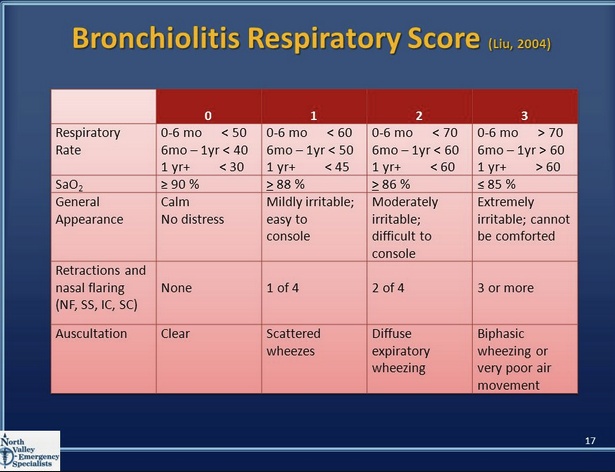
*Bronchiolitis scoring. If the score improves by 2 points with treatment that is significant. This scoring system can only be used to assess the effect of an intervention. It has not been validated to determine disposition. However, 3 is considered a low score and 8 is a high score that may necessitate ICU admission.
Elise comment: Do a score, suction, do another score. This will be the best measurement of the effectiveness of suctioning.
Ede/West GU Emergencies
Treatment for paraphimosis
Prior to reduction attempts, give local anesthetic with a dorsal penile block or ring block.
Attempt manual reduction by squeezing edema from foreskin and attempting to direct the foreskin over the glans. You can use an ace wrap to compress the edema from the foreskin prior to attempting reduction. Alternatively you put granulated sugar or mannitol-soaked gauze on the edematous foreskin to draw out the edema. Osmotics (sugar or manitol) may take an hour or more to work.
If these strategies are unsuccessful, you can use a 25g needle to make multiple punctures in the edematous foreskin to help edema drain.
Last strategy prior to surgery would be to make a dorsal slit thru the edematous foreskin.
Management of gross hematuria with clots: Start with manual irrigation of the bladder with a 60 ml Toomey syringe. Follow that up withcontinuous bladder irrigation in the ED. If gross blood with clots doesn’t clear in the ED these patients should be admitted for continued irrigation and GU evaluation. If the urine clears with irrigation these patients can be considered for discharge.
Fournier’s Gangrene: You need to emergently consult GUfor source control of this infection with surgery. Next, start big gun antibiotics(Zosyn, Vanco, and Gent) and include Clindamycin (inhibits toxin production). Alcoholics and diabetics are more prone to this infection.
*To detorse a testicular torsion, “open the book” on the affected testicle only. There seemed to be some consensus among those present that you detorse only 90 degrees at a time and re-assess by seeing if the pain is better or use bedside ultrasound to see if there is blood flow restarted to the testicle. If no change in pain or flow then detorse another 90 degrees.
Consider imaging the kidneys of elderly patients with pyelonephritis or urosepsis. There is a significant percentage of patients that will have ureteral stones and obstruction. You can get a CT, get a formal US, or do bedside US to check for stone and hydronephrosis.
Factors that increase the risk of developing kidney stones include:
- Family or personal history. If someone in your family has kidney stones, you're more likely to develop stones, too. And if you've already had one or more kidney stones, you're at increased risk of developing another.
- Dehydration. Not drinking enough water each day can increase your risk of kidney stones. People who live in warm climates and those who sweat a lot may be at higher risk than others.
- Certain diets. Eating a diet that's high in protein, sodium and sugar may increase your risk of some types of kidney stones. This is especially true with a high-sodium diet. Too much sodium in your diet increases the amount of calcium your kidneys must filter and significantly increases your risk of kidney stones.
- Being obese. High body mass index (BMI), large waist size and weight gain have been linked to an increased risk of kidney stones.
- Digestive diseases and surgery. Gastric bypass surgery, inflammatory bowel disease or chronic diarrhea can cause changes in the digestive process that affect your absorption of calcium and water, increasing the levels of stone-forming substances in your urine.
- Other medical conditions. Diseases and conditions that may increase your risk of kidney stones include renal tubular acidosis, cystinuria, hyperparathyroidism, certain medications and some urinary tract infections. (Mayo Clinic Reference)
Marshalla UTI’s
Bacteria found in the urine of men and pregnant women is always abnormal and should be treated.
Nitrites are produced by gram negative bacteria only. The bacteria has to be present in the bladder for four hours to make nitrites.
Elise reference: Asymptomatic bacteriuria is common among older adults and practically universal among those with indwelling catheters.[7] The prevalence in healthy older women living in the community is around 20%, and in men >75 years old is 6-15%. In LTC facilities, the percentages are even higher: 25-50% in women and 15-40% in men.[11] The rise in prevalence parallels the increase in comorbidities, especially neurological, associated with micturition problems.[3,7]
The recommendations by the Infectious Diseases Society of America[11] and the Society for Healthcare Epidemiology of America[3] are clear concerning asymptomatic bacteriuria in the older population, whether residing in the community or in LTC facilities: routine screening and treatment are not recommended. There have been several studies[13-16] showing no benefits associated with the treatment of asymptomatic infections as measured in the rate of subsequent symptomatic infections, improvement of chronic urinary symptoms, or survival. Moreover, some harm can be caused, mostly associated with side effects of antimicrobials and increased resistance in uropathogens.[3,4,11]
Above is from Medscape, can find a similar message in many recommendations: http://www.medscape.com/viewarticle/586757_3
Traylor Personal Medical Kit
Logan told the tragic tale of how he had to resuscitate his dog that was seriously injured on a vacation.
Preventable deaths in the outdoors: Hemorrhage, tension pneumothorax, airway obstruction
Your kit should have: tourniquet, scalpel and tube for chest tube. Oral airway, LMA or ET tube. Narcan, epi-pen, and albuterol mdi.
Schmitz Parkland Burn Formula
*Remember the 49er’s. 4ml in the formula and rule of nines. Palm=1% BSA but Palm does not include fingers. The picture is a little incorrect. Only the palm (no fingers)=1% BSA.
Lee Managing Stress in the ED
Stress impairs cortical functioning.
Manage your 4 domains when in a Resuscitation:
1. Environment: Set up the room optimally
2. Team: Give your team direction, specific roles and use clear communication
3. Self: Manage your own anxiety, your communication
4. Patient: Focus the other three domains on the care of the patient.
Mental rehearsal: go thru the procedure or resuscitation over and over in your mind before you need to do it.
*Arousal control: Square breathing
Positive self-talk: Navy Seals and athletes continually tell themselves they can do it, accomplish the goal, they have the necessary skills and training. They are prepared.
This builds confidence and increases the probability of accomplishing the task.
Visualize goals: Identify and map out all the smaller goals to reach the end goal.
Regan VP Shunt Obstruction
Shunt obstruction may cause change in mental status, headache, vomiting, or autonomic instability.
An obstructed shunt will not have the normal “squishy” shunt pump when you press on it.
If you are in a place where neurosurgery is unavailable and the patient is comatose or peri-code. You should tap the shunt to relieve pressure and test for infection.
To tap a shunt: Prep the skin with betadine. Insert a 25g butterfly needle perpendicularly into the shunt. Gently draw back CSF and send it to the lab. If you cannot withdraw CSF there is likely a proximal shunt obstruction and this patient needs to go to the OR emergently.
Stanek CHF Management
Think NAP: Nitro, Ace-I, and Positive pressure ventilation
Give nitro sprays initially and get IV dosing to about 100micrograms/min as soon as you can
ACE-I’s can be used also to lower BP/afterload
Bipap provides more functional alveoli and has been shown to improve oxygenation and prevent intubation.
Muhammad Pediatric Abdominal Pain
I missed a large portion of this excellent lecture.
HSP with significant abdominal pain should get an U/S to evaluate for intussusception. 5% of Kids with HSP can intussuscept. Intussusception is one of the few indications for steroids in HSP.
*Pediatric Appendicitis Score. Imaging strategy is usually start with U/S and if you need further imaging go to limited CT of the appendix area to minimize radiation exposure.
*ACMC Appendicitis Protocol
In the patient with possible ovarian torsion, the imaging study to get is pelvic ultrasound with doppler evaluation of vascular flow to ovaries.
If you see gallstones in an infant or small child think sickle cell disease or hereditary spherocytosis.
Katiyar Am I Really Too Slow? Billing and Coding
It doesn’t matter if you are fast. It matters how well you document.
Most EM jobs pay based on RVU generation. RVU=Relative Value Unit. It has 3 components 1. Work 52% 2. Practice expense 42% (EM is lower than other specialties) 3. Professional Liability 6%. EM has a relatively low RVU reimbursement ($35 per RVU compared with Neurosurgery which is $85 per RVU)compared to other specialties because we don’t have as much practice expense.
Kelly comment: Chart to a level 5 for all your patients. If won’t incorrectly upcode level 3’s and 4’s but it makes sure you are optimizing your charting and it simplifies your exam and charting.
Harwood comments: If you see a patient with an ankle sprain, you really don’t need to document a level 5 chart. Simple complaints are candidates for brief charts.
Critical care documentation and coding very significantly increases your RVU generation.
Level 4 RVU’s =3.33=$119
Level 5 RVU’s=4.93=$176
Critical Care RVU’s=6.33=$226
To max out your RVU’s , See the patient, treat them, and dispo them as quickly/smartly/efficiently as possible. Chart as you go. Don’t let your charts pile up. Charting later tends to negatively impact your documentation.
Poor charting leads to down-coding which negatively impacts RVU generation.
When doing ROS and HPI items, you only need one item per body area.
4-2-10-8“Fortutenate” Is the simple mnemonic to remember billing requirements for a level 5 charts.
4 descriptors of chief complaint, 2 past history items: medical/surgical/social, 10 ROS areas, 8 physical exam areas
Holland/West Administrative Updates
We discussed process improvements with getting new ECG’s and retrieving old ECG’s.
We discussed other actionable items that people brought up.