Today’s Conference Notes contains 2 weeks of Learning! Both May 25th and June 1st are included in this post.
Meyers and Faculty Wilderness Medicine Conference
Top things I learned without taking notes:
1. Top causes of death in the wilderness are: 1. sudden cardiac death/ACS, 2. drowning, and 3. exposure (hypo/hyperthermia)
2. Most common injuries in the wilderness are musculoskeletal and soft tissue injuries such as fracture, sprain, dislocation, contusions, lacerations.
3. Prior planning can significantly decrease your risk of death, illness, injury in the wilderness. Be sure to have enough water, some food, and a rain jacket/insulating layer in case weather conditions change suddenly.
4. We all agreed that probably the best strategy tomake a fire in the wilderness would be to pack water/wind proof matches and take some cotton balls with Vaseline smeared on them in a plastic sandwich bag. Thewater/wind proof matches are not that expensive and the Vaseline coated cotton balls are very light and compact. When you use the match to light the cotton balls they flame very quickly providing a great fire starter.
5. Have a first aid kit with medications/supplies to treat anaphylaxis, clean and repair wounds, treat pain and ACS with aspirin, and have a broad spectrum antibiotic with multiple indications. Elise recommended Levofloxacin as a once a day antibiotic with a wide spectrum of indications (pulmonary, urine, skin, bite wounds).
6. Tourniquets are a good thing for life-threatening limb bleeding. Recent military data demonstrates that if you apply a tourniquet proximal to life-threatening bleeding in an extremity before shock develops, the survival rate is around 95%. If you apply the tourniquet after shock develops, the survival rate drops to around 35%. Tourniquets can remain in place for 2 hours without much negative effect. The tourniquet articles that John Meyers sent out are an excellent read and worth your time.
7. Treat jelly fish stings by irrigating/rinsing with sea water. For patients having severe pain try immersing the limb under hot water. Some toxins are heat labile and pain may improve. Most jelly fish stings resolve in 15-30 minutes.
8. Moving injured people in the wilderness is energy intensive and difficult. Splinting a patient so that they can walk or even partially mobilize them can sometimes be life-saving.
9. Humans don't have as much fear of fast moving water as they do of cliffs but more people die of drowning or going over rapids/water falls than falling of cliffs. Be cautious of fast moving water.
Htet STEMI Conference
Case 1. Patient presents with chest pain, altered mental status, and hyperglycemia. EKG shows diffuse ST elevation.
*Example of similar EKG.
Troponin was elevated above 8. Second EKG shows similar diffuse ST elevation. For the most part, the ST segments were concave upward making myopericarditis more likely. ABG and anion gap shows DKA. Troponin continued to trend up. Echo was performed in the ED which showed 35% EF and hypo-kinesis of the baso-inferolateral wall. Patient was managed medically for DKA.
The next day patient went to cath lab and had clean coronary arteries. Diagnosis was myopericarditis.
Patient was transferred to ICU. At about 6 hours in the ICU, patient suffered a PEA arrest.
A recent retrospective review of myopericarditis shows that the prognosis of myopericarditis is for the most part excellent. 3.5% of patients will have residual CHF. A handful of patients had sudden cardiac death or tamponade.
Case 2. Elderly patient presents with syncope.
EKG shows Sinus rhythm, slightly long PR interval, some inferior Q waves and poor R wave progression.
Initial work up with labs and CT was non-specific.
3 hours later in the ER the patient had another episode of syncope.
Cardiac Catheterization did not demonstrate acute coronary occlusion but did demonstratechronic coronary disease. Patient had episodes of V-tach in the lab and was treated with amiodarone and lidocaine.
Treatment for Recurrent V-tach
Amiodarone
Lidocaine
Magnesium
Correct hypokalemia
Atropine
Transvenous overdrive pacing
Beta-blocker
AICD placement
Monomorphic V-tach is usually due to scarring of the ventricle. Polymorphic V-tach is usually due to ischemia. Cardiologist consensus was that amiodarone was the go-to drug for any form of Ventricular tachycardia.
Cardiologists felt that beta-blockers should be given for recurrent V-tach if the patient is not hypotensive, in shock, or has asthma. I asked cardiology how it works that we are beta blocking the patient while at the same time overdrive pacing them. They said at a cellular level it makes some sense. You want to block ventricular beta receptors and use the pacing to shorten the refractory period.
Case3. Patient with diffuse ST depression and ST elevation in AVR can mean proximal LAD occlusion.
*1 Proximal LAD Occlusion EKG.
Marshalla 5 slide F/U
Patient presents with sore throat and fatigue. On exam the patient has malaise. Initial clinical picture appeared more like a viral syndrome. Patient requested water from the doctor.
Lab work up shows hyperglycemia, anion gap acidosis consistent with DKA. Patient did turn out to have positive mono test.
*Diagnostic Criteria for DKA and HHS
Treatment of DKA= VIP=Cautious Volume replacement, Insulin, Potassium replacement.
Be cautious of the patient with malaise, weakness, and fatigue. Keep DKA in your differential.
Einstein 5 Slide F/U
Young adult male presents with chest pain. Exam was unremarkable. EKG showed diffuse ST elevation consistent with pericarditis. Troponin was elevated. CRP was elevated. ECHO and MRI showed acute myocarditis. MRI of the heart can show ventricular dysfunction in myocarditis. Diagnosis was myopericarditis.
*There is a spectrum of myo-pericarditis depending on the involvement of the pericardium and myocardium.
Kennedy Neutropenic Fever Bundle and A-Lines
I missed this excellent lecture but with the Neutropenic Fever Bundle, nurses can now access the porta-cath to draw blood and give fluids and meds without getting a CXR prior to usage.
Lee Ectopic Pregnancy
The discriminatory zone for transvaginal U/S is 1500-2000 hCG units. Viable IUP’s have an hCG increase of at least 66% over 48 hours. 15% of normal pregnancies can have a lower than expected (<66%) increase over 48 hours. 72 hour re-test may be more practical for patient convenience and getting a significant rise in hCG. If the hCG is not rising normally over three measurements then the pregnancy is considered abnormal.
Okubanjo Healthcare Disparities
Health disparities= Certain populations have different health problems due to genetic predisposition (type 2 dm, sickle cell disease, kidney stones)
Healthcare disparities= Certain populations have different healthcare access and quality due to racism, economics, or other discriminatory social factors.
Pain management has been shown repeatedly to take longer and have lower dosing in minority populations.
Girzadas question: How does a doctor monitor this issue in their own practice. How do we know we are not giving disparate care? Answer: Work to consistently treat all patients the same way.
Hayward Heme-Onc Study Guide
*Tumor Lysis Sydrome
Petechiae and mucosal bleeding are associated with low platelets or dysfunctional platelets. Thrombocytopenia does not usually result in deep tissue bleeding such as retroperitoneal bleeding or hemarthrosis.
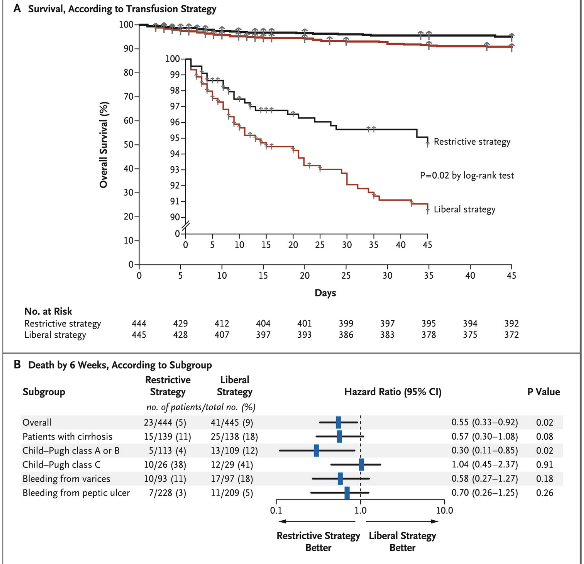
*Transfusion strategies in GI Bleeding
The most recent recommended threshold for PRBC transfusion in a patient with GI bleeding is HGB of 7. This more restrictive strategy demonstrated a better outcome than the liberal strategy of a cutoff of HGB of 9. The faculty all felt that if the patient is actively bleeding from the GI tract and the HGB is 8 or 7.5 they are going to start a PRBC transfusion rather than wait until the HGB gets to 7. Also patients with coronary ischemia associated with a GI bleed should be transfused at a HGB of 9.
Ted Toerne rule: In any test question or in real life, if the O2 sat is 85% and the patient is cyanotic consider strongly methemoglobinemia. The light wavelength of methemoglobin sets the pulse oximeter to 85%.
The youngest age a sickle cell patient can receive hydroxyurea is 9 months of age.
Acute hemolytic transfusion reactions will demonstrate on lab testing: shistocytes, low haptoglobin, free HGB in the blood and urine. Patients may develop hyperbilirubinemia over several hours.
*Cryoprecipitate components.
*Discuss with cardiology before giving Plavix or Brilinta for acute MI patients. If cardiac cath shows the need for CABG, use of these agents may delay or complicate surgery.