Tekwani Quarterly Difficult Airway Conference
3 Indications for Intubation
1. Protect airway 2. Failure to oxygenate or ventilate 3. Anticipated Clinical Course
Assessing for Difficult Laryngoscopy
These are the bedside tools to assess for difficult laryngoscopy
Difficult Bag-Valve-Mask mnemonic "ROMAN"
Radiation Obesity/Obstruction/OSA Mask seal/Mallampati/Male Age older than 55 No teeth. Any of these portend difficult bagging.
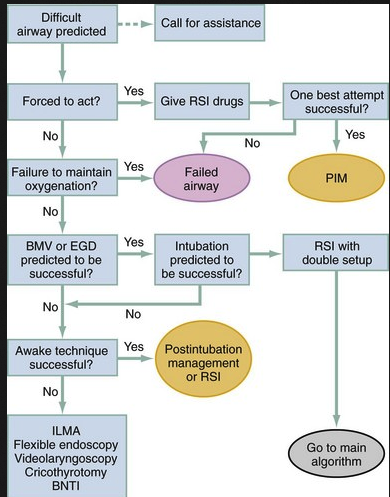
Difficult Airway Algorithm from Ron Walls Difficult Airway Course
Optimize your preoxygenation with a NRB hooked up to O2 open to flush rate (wide open, turn the dial on the wall oxygen device as far as it will go. This has been shown to provide more FIO2 than 30L/min) or use Bipap. Also hook up passive oxygenation with 15L NC. Keep the patient upright when preoxygenating.
Faculty Pearls
Consider increasing etomidate dosing for induction to 25mg for morbidly obese patients
For intracranial hemorrhage pre-treat patients with fentanyl 3 micrograms/kg given slowly a few minutes prior to giving your induction agent.
Avoid succinylcholine 72 hours to 6 months post stroke or other neuro injury.
Thenar grip is superior to C3 or other bagging techniques.
When intubating children place some towels behind their torso to elevate the thorax to give more room for the larger occiput and to better line up the external ear canal to the sternal notch.
Intubating LMA is a key rescue device to have ready to go for difficult intubations. It can be used as a bridge to cricothyrotomy and/or provide 1 further attempt at intubation if you are able to effectively bag through the LMA.
Carlson Critical Care Toxicology
Unfortunately I missed this outstanding presentation
Alex/Wigfield Emergencies in Lung Transplant Patients
The survival of lung tansplant patients is 50% at 5 years. The first year after transplant has the highest risk of death. If a patient survives the first year they have a 70% 5-year survival.
Lung transplant patients can suffer from gastroparesis due to vagal nerve injury, opioids and diabetes.
Lung transplant patients are immunocomprised. Beware of unusual and atypical presentations. Infections can progress rapidly and be catastrophic. Culture and image aggressively. Start antibiotics rapidly. Always contact the Lung Transplant Service early in the ED course 708-684-9646 or even better use Perfect Serve to contact Dr. Alex.
Calcineurin inhibitors (cyclosporin, tacrolimas) can cause elevated ammonia levels. So if a lung transplant patient is obtunded or comatose check an ammonia level. These drugs can also cause PRES (Posterior Reversible Encephalopathy Syndrome)
Diagnostic pathway to PRES
Bilateral posterior findings of PRES on MRI
Acute rejection occurs mostly in the first year after transplant. The key findings are pulmonary symptoms (dyspnea, cough, abnormal CXR) and/or a drop in FEV1. CXR's may show infiltrates or be clear. You will likely need to treat for both rejection with IV steroids and infection with IV antibiotics. Dr. Alex was more concerned that we treat possible infections with broad spectrum antibiotics. The Transplant Service will order steroids later if needed.
Anti-rejection medications are prone to cause renal failure, encephalopthy, and serious infections. (Think Beans, Brain, Bugs)
If you are going to get a CT chest on a lung transplant patient do it without contrast unless you are looking for PE. You want to avoid any contrast insult to the kidneys if possible.
Patients on steroids can have perforated viscous without minimal abdominal symptoms. Steroids can also make patients prone to bone fractures and AVN.