Ryan/Traylor Oral Boards
Case 1. 65 yo male with right flank pain. He has a fever and is borderline tachycardic. Patient has history of lymphoma and is on Chemotherapy. On exam, patient has a herpes zoster type rash on right flank and multiple other areas of his body.
Diseminated Herpes Zoster (DHZ) Rash. It is bilateral and is not localized to a single dermatome. The condition is called disseminated herpes zoster (DHZ) when more than 2 contiguous dermatomes are affected, more than 20 vesicles are observed outside the initial dermatome, or involvement is systemic. DHZ is rare and most frequently occurs in immunocompromised patients.
The patient has neutropenia on CBC. IV acyclovir was started 10mg/kg Q8 hours. Patient was also given antibiotics for neutropenia.
Airborne precautions: Airborne droplet nuclei measuring ≤5 μm can remain infective and suspended in the air for hours at a time, particularly in enclosed and poorly ventilated spaces. Airborne transmission of tuberculosis,63-65 measles,66,67 and severe acute respiratory distress syndrome (SARS)68–70 has been described in ED settings. Varicella(including disseminated zoster), highly pathogenic influenza, and smallpox may also be transmitted in this manner. Rapid identification and isolation of ED patients suspected of harboring an airborne disease hinges greatly upon heightened clinical suspicion, as in the case of tuberculosis.71Proper HCP protection against airborne droplet nuclei requires use of either an N95 or powered air purifying respirator. (Liang, Ann Emer Med 2014)
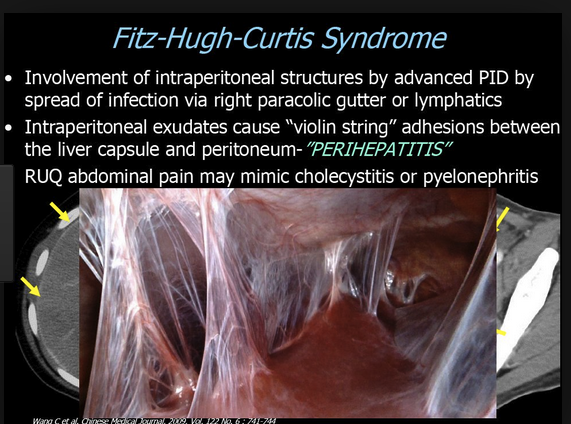
Case 2. 19yo female presents with right side abdominal pain. She has fever and tachycardia. UCG is negative. On history, patient has abnormal vaginal discharge. Exam demonstrates RUQ tenderness as well as CMT and bilat adnexal tenderness on pelvic exam.
Liver enzymes are not diagnostic. They may range from normal to markedly elevated.
Treatment should include
Alternatives include gentamicin + clindamycin; or ampicillin/sulbactam + doxycycline
Continue parenteral antibiotic administration for 24 hr after clinical improvement, then switch to oral antibiotics to finish 14 day course
Laparoscopy can be used to lyse adhesions in the acute and chronic stages of Fitz-Hugh–Curtis syndrome
Add metronidazole when anaerobes are a particular concern
Case 3. 4 yo male with left hip pain and won't bear weight. No fever. Other vitals are normal. History reveals patient had a mild viral illness a week prior. X-rays are negative. Labs are all normal. Diagnosis is toxic synovitis.
You can differentiate toxic synovitis from septic hip by normal CBC, ESR, and CRP and no fever. You should also get X-rays of the hip. Harwood comment: Assessing the response to NSAID's is really a critical action. If the child can walk after oral NSAID's that is a key finding to ruling out septic joint.
2011 Singhal Journal of Bone and Joint Surgery Br. If a child has a normal CRP and can bear wieght, he/she has a low risk of septic joint. Abscence of fever and low WBC count also help differentiate but are less predictive.
Toerne ETOH Withdrawal
4 ETOH Withdrawal Syndromes include: Seizures, Uncomplicated withdrawal, Alcoholic hallucinosis, and DT's.
Seizures: Occur early in the course of withdrawal. (within 48 hours of cessation of drinking) Commonly the first symptom of withdrawal. These are brief, self-limited, generalized tonic clonic seizures.
Uncomplicated Alcohol withdrawl: Hyperadrenergic vital signs and tremor. There is no altered mental status.
Alcoholic Hallucinosis: Rare syndrome. Patients have hallucinations with otherwise intact mental status. Ted says he is not certain this syndrome exists.
Delirium tremens: The patient has adrenergic storm plus delirium. Delirium defines this syndrome. This can occur 3-10 days after cessation of drinking.
First management goal is to identify the patients in withdrawal or at risk of withdrawal.
Ted-T's key screening questions: How many days per week do you drink? When you drink, how much do you drink?
Other clues to alcohol abuse include ruddy facial complexion, swollen hands and feet, hypokalemia, hypomagnesiemia, anemia with an MCV around 105, and thrombocytopenia.
Management: Provide a quiet environment with frequent re-assessment. Screen these patients for other medical or traumatic problems. Administer withdrawal-specific therapy.
Ted suggests: Give two doses of lorazepam 2-4mg about 10-15 minutes apart. If patient still has severe withdrawal symptoms following that, give 10mg/kg of phenobarbital. If they still have severe withdrawal symptoms after lorazepam and phenobarbital, they are headed to the MICU. At that point start 5mg/hour lorazepam drip. Give another 5mg/kg of phenobarbital. If still having trouble managing withdrawal symptoms, the third line drug would be ketamine. Ted advocates early use of phenobarbital if the initial lorazepam is not controlling the patient's withdrawal signs.
Dawson Pediatric Sepsis
Gabby's Law requires screening protocols and severity stratification of pediatric sepsis. It also requires reporting of pediatric sepsis in Illinois.
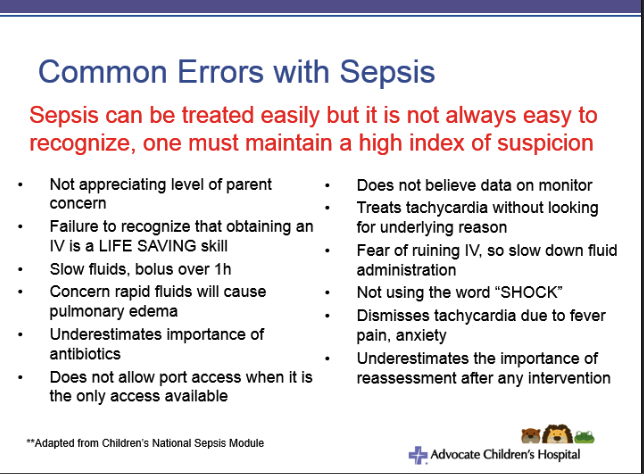
Remember that irritability or lethargy can be a sign of organ dysfunction (CNS). Lactate is not reliable for identifying sepsis in pediatric patients. If it is high, it is concerning. If it is normal the child may still be septic.
Risk factors for sepsis include: cancer, transplants, immunosuppression, short gut, congenital heart disease, indwelling lines and devices, chronic medical problems.
We screen for pediatric sepsis with vital signs and a bedside huddle.
This child's vitals point to sepsis. Next step is a bedside huddle with other caregivers to decide if further concern for sepsis is warranted and continuing down algorithm or if the patient has an alternative diagnosis.
In the first 20 minutes give a first IV fluid bolus 20ml/kg, start high flow O2, and get antibiotics ordered.
You need to get IV fluids into a kid rapidly using a push-pull method. Give 3 20ml/kg boluses in the first hour. Give antibiotics in the first hour. Start high flow O2 on all suspected sepsis patients.
Berklehammer GI Bleeding
Unfortunately I missed this excellent lecture.