Girzadas/Chinwala Oral Boards
Case 1. 55yo male presents bradycardic and hypotensive after beta blocker overdose.
Tintinalli algorithm for different modalities to treat beta blocker overdose.
Case2. 7 yo male with GSW to the right thigh. Patient is hypotensive and tachycardic. Patient was resuscitated with IV crystalloid and IV PRBC transfusions. Patient had abnormal ABI and soft signs of vascular injury. Patient had CTA showing vascular injury an patient was taken to the OR.
Tintinalli algorithm for management of penetrating vascular trauma.
Case 3. 4yo male who had non-fatal drowning.
If normal O2 sat, normal mental status, normal lung exam after 4-6 hours patient can go home.
Pecha Kucha
Robinson Foley Catheters
The most frequent complication of urethral catheterization is infection. Foleys are the #1 cause of nosocomial infections so use them judiciously.
Patients are colonized within about a week of an indwelling foley catheter. So diagnose UTI only in symptomatic patients and/or with positive culture results.
Dr. Lovell comment: If the nurse can’t place the foley, the emergency physician needs to attempt placement of foley prior to consulting GU.
Florek Tracheostomy Problems in the ED
Risk of tracheo-innominate fistula is highest at 7-14 days after surgery.
Lubricate the Shiley prior to placing it in the tracheostomy site.
You can attempt to oxygenate patients with a mask over the patient’s mouth or over the trach site.
Some patients are neck breathers and can’t exchange air through the mouth (laryngectomy, laryngeal mass)
Most common cause of tracheostomy bleeding is mucosal irritation. Worst cause is tracheoinnominate fistula.
To control TI fistula first overinflate the shiley balloon to tamponade the bleeding. If that is ineffective you can insert your finger in the tracheostomy site and compress against the sternum
Tracheoinnominate fistulas are quite rare, occurring in less than 2% of cases, but they carry a mortality rate of 25% to 50%.9 They may present as the classic “exsanguinating bleed” but often present with a less impressive sentinel bleed. Any bleeding of more than a few milliliters of blood should raise concern for a possible fistula of the innominate artery. Prompt critical resuscitation measures and emergent consultation with a Vascular Surgeon and Otolaryngologic Surgeon is required. Definitive management is surgical. Techniques for temporarily controlling bleeding from the innominate artery include local digital pressure, hyperinflation of the tracheostomy tube cuff, and traction on the tracheostomy tube. An alternative method is to deflate the tracheostomy tube cuff, reposition the cuff at the bleeding site, and then reinflate or hyperinflate the cuff. When bleeding occurs, the tracheostomy tube should not be removed until the airway is secured by another means from above (orally or nasally). (EM Procedures Reference)
Erbach Dialysis Access Complications
50% of dialysis catheters develop an infection within 6 months.
AV grafts have 10% rate of infection, and AV fistulas have a 5% rate of infection
Bleeding from dialysis graft, treat with direct pressure or quickclot gauze. Consult with Vascular Surgery. Below are some other suggestions from Tintinalli.
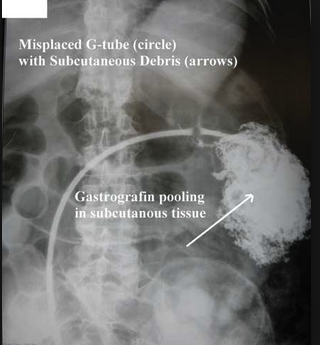
Friend G-tubes
If G-tube is clogged, first try with flushing with warm water. If that won’t work, your can try cola.
If a g-tube site is less than 4 weeks old don’t replace the tube and just consult GI. In the first 4 weeks, the site is not fully mature and replacing the tube could end up in the wrong place. After 4 weeks we need to get the tube replaced as soon as possible to avoid closure of g-tube site.
Don’t replace J-tubes.
Gastrograffen in SubQ
Intraperitoneal gastrograffen
Lorenz Insulin Pumps
Insulin pumps give a basal rate of insulin and bolus dosing when a patient eats. Patients can also have long term glucose monitors for multiple days in the skin that communicate directly with the insulin pump or an apple watch.
Patients who have pumps who are hypoglycemic, treat first with glucose then second disconnect the pump.
You can see a patient’s bolus history by reviewing their pump data.
Chinwala VP Shunts
Obstruction is more common in the first year after placement. Proximal obstruction is due to choroid plexus and distal obstruction is due to thrombosis.
Staley The Febrile Neonate
Temp of 38C at home or in the ED is considered positive for fever in the infant.
In neonates with fever, the risk for serious bacterial infection is about 13%.
The clinical appearance of a neonate does not predict serious bacterial illness. You will need to rely on tests to identify serious bacterial illness in this age group.
For patients 0-28 days of age with a fever of 38C or higher, do full septic workup. Get a CXR only for patients with respiratory symptoms such as cough or increased work of breathing. Get a NP swab to screen for RSV. Give ABX within 1 hour for these very young children. (Amp and Cefotaxime) add Vanco if the infant is critically ill or mom was treated for Group B strep.
If LFT’s are elevated, get HSV serology and start IV Acyclovir. Elevated LFT’s are a sign of HSV infection.
For patients aged 29-60 days with fever, get a CBC, blood culture, UA and urine culture. Urine studies are the highest yield tests. Again, limit CXR’s to patients with respiratory symptoms. Get a Procal, CRP and viral testing. If biomarkers are negative don’t do LP in this age group. If you don’t do LP, discharge without antibiotics. If biomarkers (WBC, Procal, CRP) are elevated, do an LP and start antibiotics. If UA is positive get a blood culture (bacteremia 10%) and consider LP (meningitis 1/200). If you do an LP and decide to treat with antibiotics, give ceftriaxone. Any discharged patient needs arranged close follow up.
Infants less than 60 days who are fussy at home and have temps close to febrile (close to 38C) should be observed in ED for a couple of hours and have temp rechecked. Consider getting a CBC, blood culture, UA, and urine culture in these borderline kids.
In infants under 60 days, a temp >/=40C indicates a 40% risk of serious bacterial illness.
Tips for doing LP’s in infants: put the CPR compression board under the patient to keep the patient from sinking into the bed. After you insert the LP needle through the skin, you can remove the stylet and advance the needle without the stylet so that you can identify CSF as soon as you enter the CSF space.
Insert the LP needle between the L4 and L5 spinous processes in the intervertebral space in the midline of the back, and direct the needle toward the umbilicus. This interspace is easily located because it lies in line between the iliac crests. Introduce the needle with the bevel of the needle up. Insert the needle until the characteristic "pop" identifies introduction into the subarachnoid space. An alternative method is to remove the stylet from the needle49 after the needle pierces the skin. Advance the needle, without the stylet, incrementally until CSF flows. Occasionally rotating the lumbar needle clockwise or counterclockwise up to 360 degrees may help improve flow if the bevel of the needle is sideways. When removing the lumbar needle, replace the stylet. (Tintinalli 8th ed)
Barounis PE and Pulmonary Embolism Response Team
From Dr. Barounis: Here are some takeaways from today's lecture, please share with other residents. I included a lot of the literature that I had obtained for the lecture so feel free to review yourself and see if you come up with different takeaways.
Imaging:
CT scans, not V/Q's for sick people please!
Massive PE:
1. Massive PE is life-threatening and immediate thrombolysis is recommended by all major societies. At ACMC surgical embolectomy can be considered if immediately available as an alternative in candidates for surgery, or when thrombolysis has been attempted and unsuccessful.
DOSE 10mg bolus, followed by 90mg over 2 hours. Consider MOPETT dosing in high bleeding risk patients (see below).
2. Hold heparin when starting tPA as there appears to be no benefit with likely a higher likelihood of bleeding.
3. Obtain a fibrinogen level prior to beginning thrombolysis (same time you are getting PT/INR/PTT). If fibrinogen is dropping consider stopping tPA, hold heparin.
4. Try high flow nasal cannula, and avoid intubation when possible prior to thrombolysis given high propensity for cardiac arrest during intubation. If diagnosis is uncertain, will require clinician judgement. Most patients die from shock, RV failure >>> hypoxemia
5. CALL 40-0702 for help This will activate the PE response team
6. Start pressors early, probably can avoid volume loading altogether. (RV perfused by MAP, not DBP)
Submassive PE:
1. Thrombolysis is indicated to reduce risk of Hemodynamic decompensation and development of respiratory failure, in the select cohort of patients at high risk of deterioration (prognostic features below)
2. The data on ultrasound-assisted thrombolysis has not been consistently shown to improve long-term outcomes, see the ULTIMA trial/ SEATTLE II trial (included below) based on RV/LV ratio @ 3 and 6 months. It did show reduce RV/LV ratio at 24 hours. ULTIMA is the only RCT comparing EKOS to heparin. The PEITHO trial also showed no reduction in PH, or death at 24 month f/u in patients who received tenecteplase vs. placebo. IT APPEARS THERE IS SHORT TERM BENEFIT, but LONG TERM patients own fibrinolytic system appears to do the job.
3. Ultrasound assisted thrombolysis has not shown improvement in clot resolution over plain catheter directed thrombolysis in the only RCT comparing the two (see below, engelberger). Each ekos catheter is around $1,100.
4. Lower dose tPA appears safe and equally effective, and is appealing in patients with submassive PE to avoid hemorrhagic complications. Currently this is done using CDT with ekos at ACMC, and future studies may prove that lower dose controlled thrombolysis will be equally efficacious?? MOPETT dosing tPA for submassive PE with high risk features, or even stable massive PE
5. Poor prognostic features: tachycardia, tachypnea, hypoxemia, lactic acidosis (>2), PESI SCORE, BOVA SCORE, poor cardiopulmonary reserve.
6. Patients with concomitant DVT and PE have higher inpatient mortality than PE alone.
PERT TEAM:
Call 40-0702; please obtain the labs provided in order set (top righ thand side of PERT DOCUMENT included below).
Best,
Dave
Proposed Management Algorithm for Massive and Sub-massive PE