Patel/Burch Oral Boards
Case 1. 30 yo female patient presents with syncope. Patient was tachycardic and hypotensive. Patient had some abdominal tenderness. Further history revealed that patient had a fall about a week earlier on to her left side. On FAST, patient has free fluid in morrison’s pouch. Diagnosis was splenic rupture. Patient required IVF and IV PRBC’s to resuscitate and get to OR for surgical management.
According to the American College of Surgeons (ACS), mortality from splenic injuries accounts for approximately 10% of all trauma-related deaths [5]. In 1998, Cocoanour stated that the incidence of delayed splenic injury was approximately 1% [6]. However, in 2017, Furlan et al. reported that the incidence of delayed splenic injury has risen to 3%-15% with an inconsistent association with the severity of splenic trauma [7]. Compared to the 1% mortality associated with acute splenic injury, the mortality from delayed diagnosis of splenic injury following blunt abdominal trauma ranges from 5%-15% [3]. The trend in the increased presentation of delayed splenic injury is a risk of patient morbidity and mortality and can be attributed to the difficulty in identifying delayed splenic rupture. Difficulties with diagnosing delayed splenic injury may include atypical presentations that may mimic other pathologies, the lack of symptomatology, or equivocal imaging. Due to the variability in presentation and the difficulty with the initial assessment of delayed splenic injury, it is the opinion of the authors that delayed splenic rupture be considered in the differential diagnosis of an acute surgical abdomen regardless of the time or mechanism of the inciting event.
(Chikamuche, Cureus. 2018 Feb; 10(2): e2160.)
Delayed rupture of the spleen remains a real diagnostic entity and may occur in 1% of blunt abdominal trauma victims. The process most likely results from rupture of pre-existent subcapsular hematoma of the spleen. Such a hematoma is likely the result of parenchymal injury that may or may not be detected by CT scan. Such delayed ruptures can present atypically and after minor trauma that may be interpreted by the patient to be insignificant, and therefore, forgotten. In these instances, continued clinical vigilance and early appropriate imaging will likely decrease morbidity.
(Allen, The Journal of Emergency Medicine, Vol. 23, No. 2, pp. 165–169, 2002)
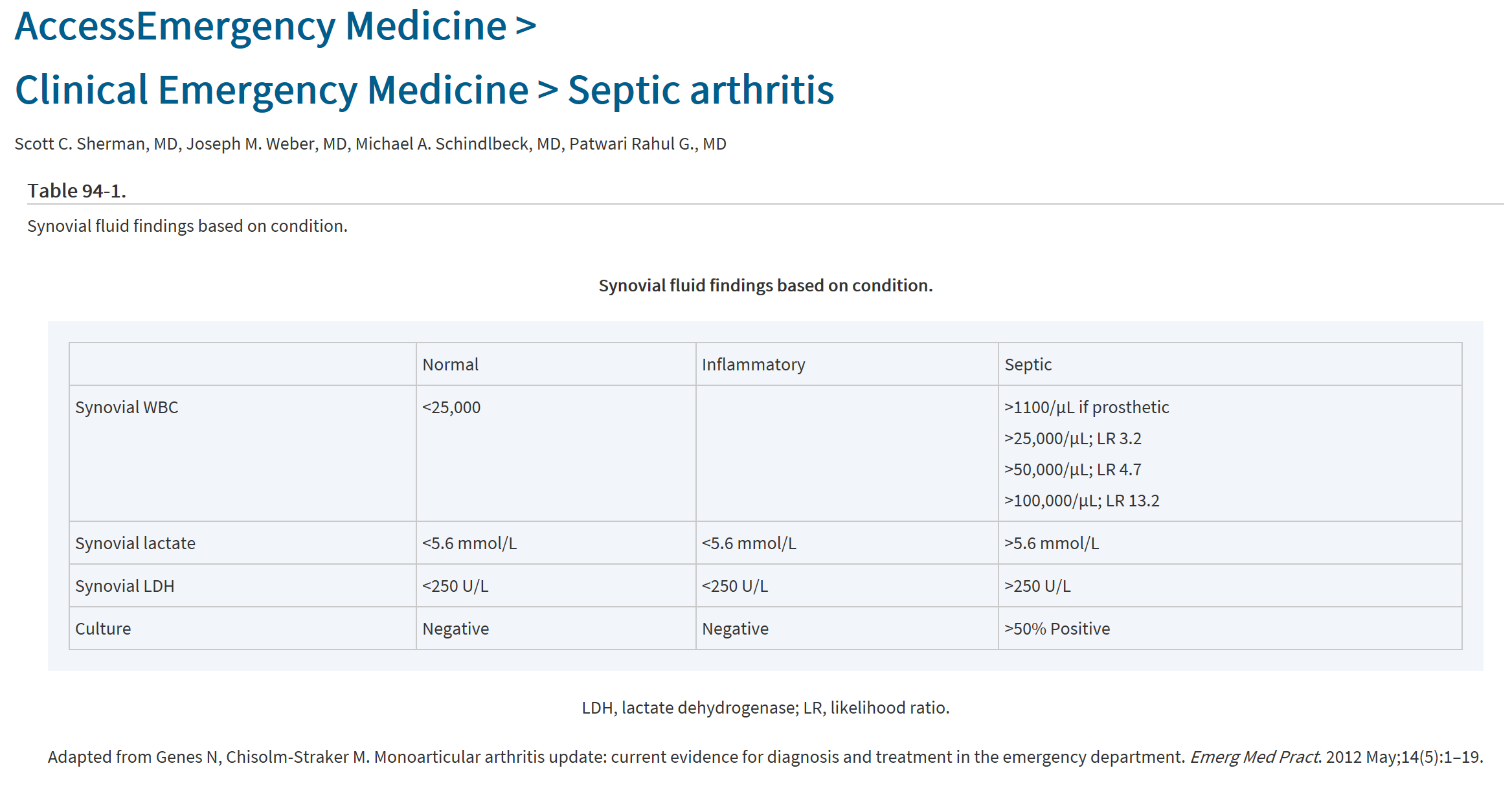
Case 2. 32 yo male patient with knee pain. Patient had concurrent paronychia on great toe of same lower extremity. Arthrocentesis of knee shows 192,000 WBC’s. Most likely patient had hematogenous spread from paronychia causing septic arthritis. Treatment requires IV antibiotics and joint irrigation.
Case 3. 39yo firefighter presents with confusion with shortness of breath. Patient is tachycardic. Patient was fighting a fire when his team members pulled him from the burning building. Exam shows soot and edema in nasal passages and oropharynx. Patient required emergent intubation to protect airway. Patient’s CO level was 22%. Patient also had 2nd degree burns on 25 %BSA.
The initial diagnosis of smoke inhalation is made from a history of exposure to fire in an enclosed space and physical signs that include facial burns, singed nasal hair, soot in the mouth or nose, hoarseness, carbonaceous sputum, and expiratory wheezing. No single method for diagnosing the extent of inhalation injury exists. Measurement of arterial carboxyhemoglobin is used to document prolonged exposure to products of incomplete combustion. The chest radiograph may be normal initially. Bronchoscopy and radionuclide scanning may also be helpful in evaluating the full extent of injury.
Treat suspected inhalation injury prior to definitive diagnosis. Provide humidified oxygen (100%) by facemask. Obtain arterial blood gas concentrations, including carboxyhemoglobin levels. Control of the upper airway is achieved by prompt endotracheal intubation. Indications for intubation include (1) full-thickness burns of the face or perioral region, (2) circumferential neck burns, (3) acute respiratory distress, (4) progressive hoarseness or air hunger, (5) respiratory depression or altered mental status, and (6) supraglottic edema and inflammation on bronchoscopy. Additionally, consider the patient's anticipated clinical course. (Tintinalli 8th ed.)
Patient also required crystalloid resuscitation per the Parkland formula and transfer to a burn center. There also needed to be discussion of hyperbaric O2 therapy for CO toxicity with receiving hospital.
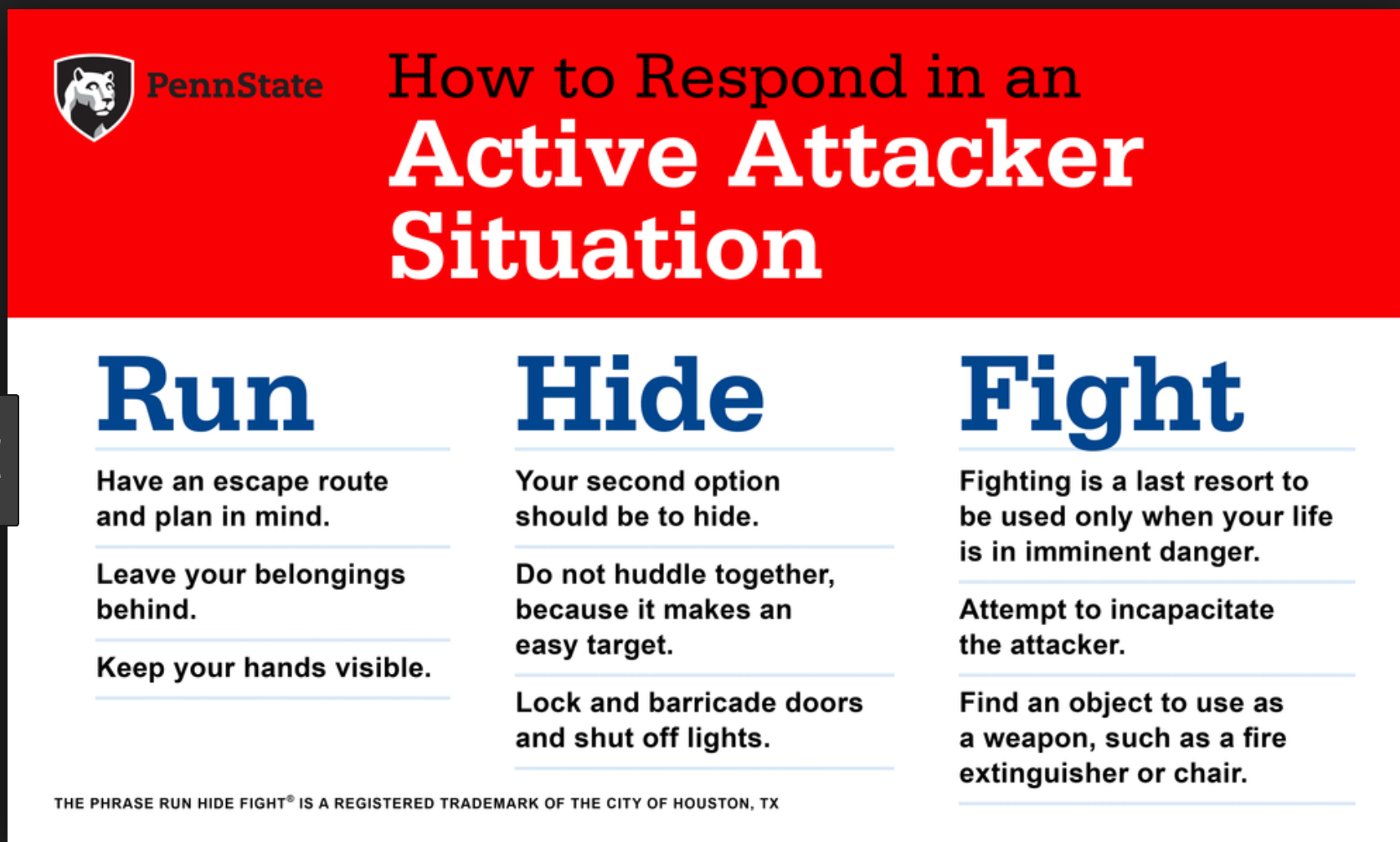
Regan/Cranmer Active Shooter Workshop
FBI definition: An Active shooter is an individual actively engaged in killing or attempting to kill people in a confined and populated area.
The Emergency Department is the most common site for violence/shooting in a hospital. 23% of hospital shootings occurred due to a person taking a security guard’s or police officer’s weapon.
Dr. Regan says, if you hear shots and don’t see a shooter, run! Don’t wait for others or stop to get your stuff. Dr. Cranmer says, it is common to downplay or ignore popping sounds. Don’t do this, be situationally aware and pay attention to those noises. If you hear gunshots or popping noises, discontinue patient care. Don’t stop for victims or try to protect patients. If you die, you can’t help the patients later. Get out of there! Your safety takes priority over co-worker or patient safety. If you are running down a long straight hallway zig-zag down the hall to make it harder for the shooter to hit you. Do not run along the wall of a hallway. Bullets tend to ricochet and fly along the wall.
When you leave the building, keep your hands up and visible. Don’t have your cell phone in your hand. Don’t make any sudden movements. Don’t approach the police. Police are there to stop the shooter. You don’t want them to mistake you for the shooter. The meeting point outside our hospital for persons fleeing from an active shooter is the Ronald McDonald House.
If you are hiding and have a cell phone, text to a person outside the hospital to notify the police. Use any object in a room to barricade the door. Don’t open the door to let others in the room. If someone knocks on the door and says they are the police, ask them to slide their badge under the door or provide some other form of verification that they are the police before opening the door.
To report a shooter, call 41-1057 (Public Safety) and call 911.
If you have to fight the active shooter, work as a team to attack the shooter. Multiple people coming at the attacker at once is harder for them to fight back. Fight dirty and fight hard. Your life is on the line.
The inventory room is the safest room in the ED to hide/barricade in. It has heavy metal doors that can be locked. In the PED, the Inventory and storage rooms are the safer rooms with metal doors.
The notification for an active shooter overhead in the hospital will be: Security Alert-Active Shooter-Location. There also may be Everbridge text notifications.
Dr. Regan and Cranmer then covered specific scenarios and walked us through the ER to demonstrate escape routes and safe areas.
This workshop was a real eye-opener for ED staff. There was much discussion about the ethical choices of protecting your personal safety vs staying with patients. Dr. Regan and Cranmer both emphasized the importance of protecting your personal safety so you stay alive to care for patients.
Mullen Intracranial Hemorrhage
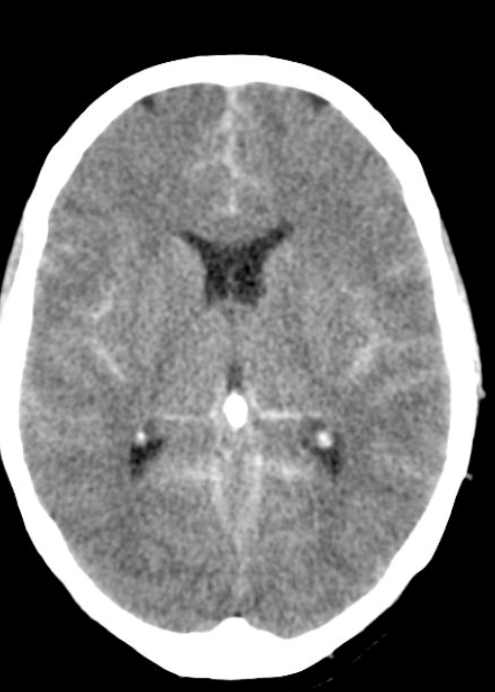
Epidural Hematoma.
Blunt trauma to the temporal or temporoparietal area with an associated skull fracture and middle meningeal arterial disruption is the primary mechanism of injury. Occasionally, trauma to the parieto-occipital region or the posterior fossa causes tears of the venous sinuses with epidural hematomas.
The classic history of an epidural hematoma involves a significant blunt head trauma with loss of consciousness or altered sensorium, followed by a lucid period and subsequent rapid neurologic demise. This clinical presentation occurs in a minority of cases. Traumatic blows to the thin temporal bone over the lateral aspect of the head carry the highest risk (e.g., baseball or pool stick injury). The diagnosis of an epidural hematoma is based on CT scan and physical examination findings. The CT appearance of an epidural hematoma is a biconvex (football-shaped) mass, typically found in the temporal region.
The high-pressure arterial bleeding of an epidural hematoma can lead to herniation within hours after an injury. Early recognition and evacuation reduces morbidity and mortality. Underlying injury of the brain parenchyma is often absent; full recovery may be expected if the hematoma is evacuated prior to herniation or the development of neurologic deficits. (Tintinalli 8th ed)
Subdural hematoma is caused by sudden acceleration-deceleration of brain parenchyma with subsequent tearing of the bridging dural veins. This results in hematoma formation between the dura mater and the arachnoid (Figures 257-8 and 257-9). Subdural hematoma tends to collect more slowly than epidural hematoma because of its venous origin. However, subdural hematoma is often associated with concurrent brain injury and underlying parenchymal damage. Brains with extensive atrophy, such as in the elderly or in chronic alcoholics, are more susceptible to the development of acute subdural hematoma. Even seemingly benign falls from standing position can result in subdural bleeding in the elderly. Children <2 years old are also at increased risk of subdural hematoma.
Acute cases usually present immediately after severe trauma, and often the patient is unconscious. In the elderly or in alcoholics, chronic subdural hematomas may result in vague complaints or mental status changes. Often, there is no recall of injury. On CT scan, acute subdural hematomas are hyperdense (white), crescent-shaped lesions that cross suture lines. Subacute subdural hematomas are isodense and are more difficult to identify. CT scanning with IV contrast or MRI can assist in identifying a subacute subdural hematoma. A chronic subdural hematoma appears hypodense (dark) because the iron in the blood has been metabolized.
The definitive treatment depends on the type, size, effect on underlying brain parenchyma, and the associated brain injury. Mortality and the need for surgical repair are greater for acute and subacute subdural hematomas. Chronic subdural hematomas can sometimes be managed without surgery depending on the severity of the symptoms. (Tintinalli 8th ed.)
Subarachnoid hemorrhage. Only 1% of patients presenting to the ED with headache have subarachnoid hemorrhage. However, 10% to 14% of those complaining of the "worst headache of their life" have subarachnoid hemorrhage.7,8 Acute onset of a severe headache is subarachnoid hemorrhage until proven otherwise.10,11 With third-generation CT equipment, CT scan done within 6 hours of headache onset is reported to have a sensitivity approaching over 99% and specificity over 99%, with a negative predictive value of 99.4% and positive predictive value of 100%.46,48 If head CT is negative for blood but suspicion for subarachnoid hemorrhage is strong, or if the patient presents beyond 6 hours of headache onset, the next step is LP to detect blood or xanthochromia in the cerebrospinal fluid. (Tintinalli 8th ed.)
Allam Chest Radiology
Detection of free intraperitoneal air (pneumoperitoneum) is one of the principal uses of radiography in patients with abdominal pain. Pneumoperitoneum is nearly always due to perforation of the gastrointestinal tract, and virtually all patients require surgery. In 80–90% of cases, free intraperitoneal air is due to a perforated peptic ulcer. An upright chest radiograph is the preferred imaging test because it readily detects free air under the diaphragm. In most cases, the clinical and radiographic findings are obvious, and radiography serves to confirm the diagnosis. Diagnostic difficulty arises when the clinical presentation is muted, particularly in elderly or debilitated patients, or when the radiographic findings are subtle (Cina et al. 1994). Although radiography can detect small amounts of free air, not all cases of peptic ulcer perforation show free air—sensitivity may be as low as 60% (Emergency Radiology)
5 T’s that give you a wide mediastinum on CXR
Thyroid enlargement
Thymoma
Teratoma
Traumatic Aortic Injury
Terrible Lymphoma
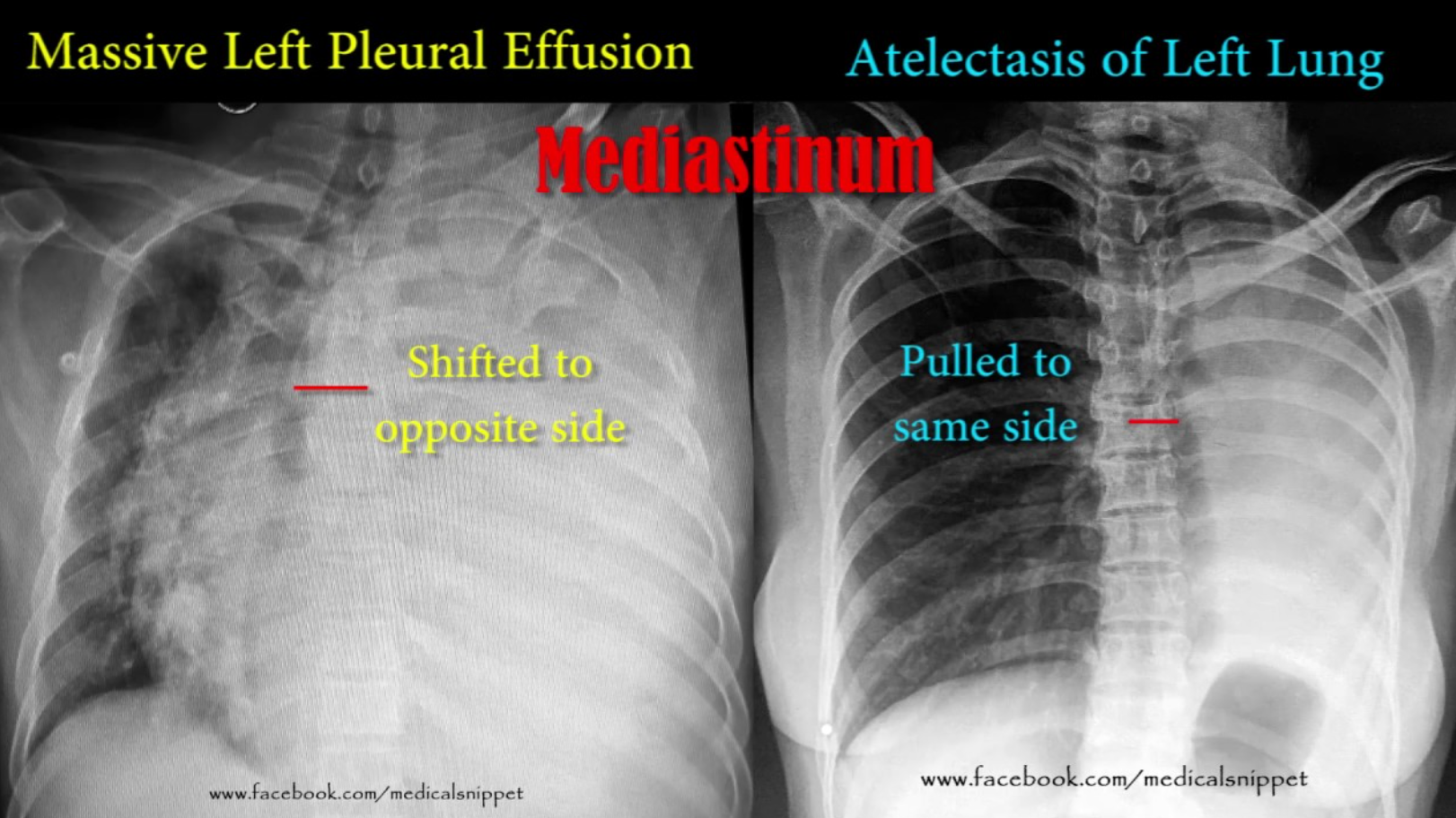
Two things will “white out” a lung, pleural effusion and atelectasis. Pleural effusion shifts mediastinum away from the affected lung. Atelectasis pulls mediastinum toward the affected lung.
Dr. Allam made the point that when checking NG tube placement, the NG tube should follow the spine until the NG gets below the diaphragm. If the NG tube is angling out laterally away from the spine in the chest you have to consider that it is in the lung. This CXR shows the NG tube in the left lung.
When checking CXRs with a pacemaker, follow the pacer wires from beginning to end to identify lead fracture. You have to look at the leads like you check ribs for fractures. You have to run your eyes over the entire wire.