Robinson M&M
No patient details, just the take home lessons.
If you have time, resuscitate and optimize your patient’s hemodynamics prior to intubation. Positive pressure ventilation will decrease venous return to the heart and patients who are hemodynamically unstable to start with are at risk for cardiovascular collapse/arrest. You can use push dose pressors in this situation. Epinephrine can be used. Simple way to do this: Put 1ml of cardiac epinephrine in a syringe with 9ml of saline. You can give 1 ml every few minutes to optimize hemodynamics.
When approaching a difficult airway, give yourself your best chance for first pass success. If you fail on your first attempt, the potential for bad outcomes increases significantly. Ken Dodd says your best chance for success on first attempt is video laryngoscopy using a standard mac VL blade and intubating with a bougie and then placing the tube over the bougie. Have a LMA as back up. Be prepared for a surgical airway. Consider using ketamine sedation and topical anesthetic and avoiding neuromuscular blockers when managing a difficult airway.
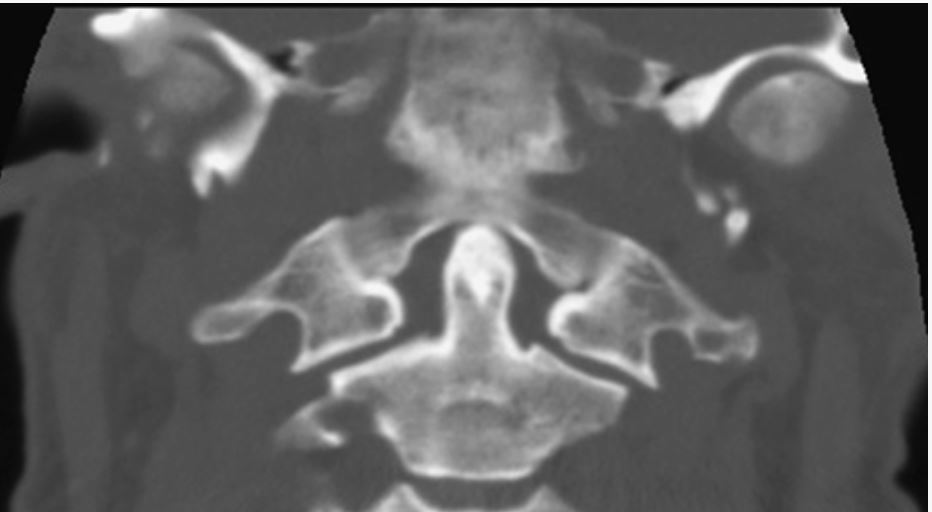
Jefferson Fracture can be tough to diagnose.
Jefferson Fracture of C1
Note the lateral masses of C1 extend beyond the lateral borders of C2. That signifies Jefferson burst fracture. In a normal C-spine the lateral borders of C1 and C2 should line up pretty much perfectly.
Associated C2 fractures occur in approximately one half of patients.
This fracture rarely leads to spinal cord injury since the fractured fragments have a tendency to fall outward away from the canal and brainstem. (The Atlas of Emergency Radiology)
Patients with multiple ED presentations for the same episode of back pain are at high risk for serious diagnoses.
Patients with new onset psychosis may benefit from CT imaging of the brain.
Don’t attempt to replace a g-tube if it has been placed within the last 4 weeks. If a new g-tube (less than 4 weeks) has fallen out, just admit the patient and consult gen surg or GI.
Sickle Cell Disease is a risk factor for rhabdomyolysis. A marker for rhabdomyolysis in a sickle cell patient is an abnormal AST or ALT.
McKean/Kishi Oral Boards
Case 1. 43yo male with leg pain and redness. Patient had a fish hook injury to his leg recently in salt water. Skin exam shows severe cellulitic changes, bullae and crepitence.
Vibrio Vulnificus infection
Labs c/w sepsis with elevated WBC and lactate. X-rays show show soft tissue air. Diagnosis was soft tissue infection from vibrio vulnificus. Treat with 3rd Gen Cephalosporin and Doxycycline or flouroquinolone.
Dr. Lovell point: Think Vibrio vulnificus with salt water source infection and Aeromonas for fresh water source infection. You can treat both with flouroquinolone.
Case 2. 16 yo male with syncope and facial contusion. Patient had syncope after swimming and injured his mouth. EKG showed short PR interval. Patient had Lown-Ganong-Levine syndrome Short PR interval with no delta wave.
The Lown–Ganong–Levine (LGL) syndrome is now believed to be due to enhanced AV nodal conduction. The proposed mechanism is an intranodal bypass tract or atrionodal tracts formerly known as James fibers. This diagnosis has been largely abandoned in the era of electrophysiology. Syndrome diagnostic criteria classically have been: a short PR interval (less than 0.12 s) and a normal QRS complex on ECG, and the clinical history of intermittent palpitations or episodes of paroxysmal SVT, atrial flutter, or atrial fibrillation.
The most important differential diagnosis is that of the WPW syndrome that has a specific treatment. The ECG finding that differs is the delta wave leading into the QRS complex seen with WPW; this is not found in LGL. (Atlas of Cardiovascular Emergencies)
LGL EKG
Case 3. 31yo male presents with elbow pain. Patient was recently scuba diving. Vitals and physical exam of the elbow are normal. Xrays of the elbow are normal. Labs are normal. Arthrocentesis was done and the joint fluid analysis was normal. Diagnosis was the decompression sickness. Treatment is hyperbaric O2.
Dr. Lovell point: Decompression sickness and arterial gas embolism are both indications for hyperbaric oxygen.
Regan Emergency Preparedness
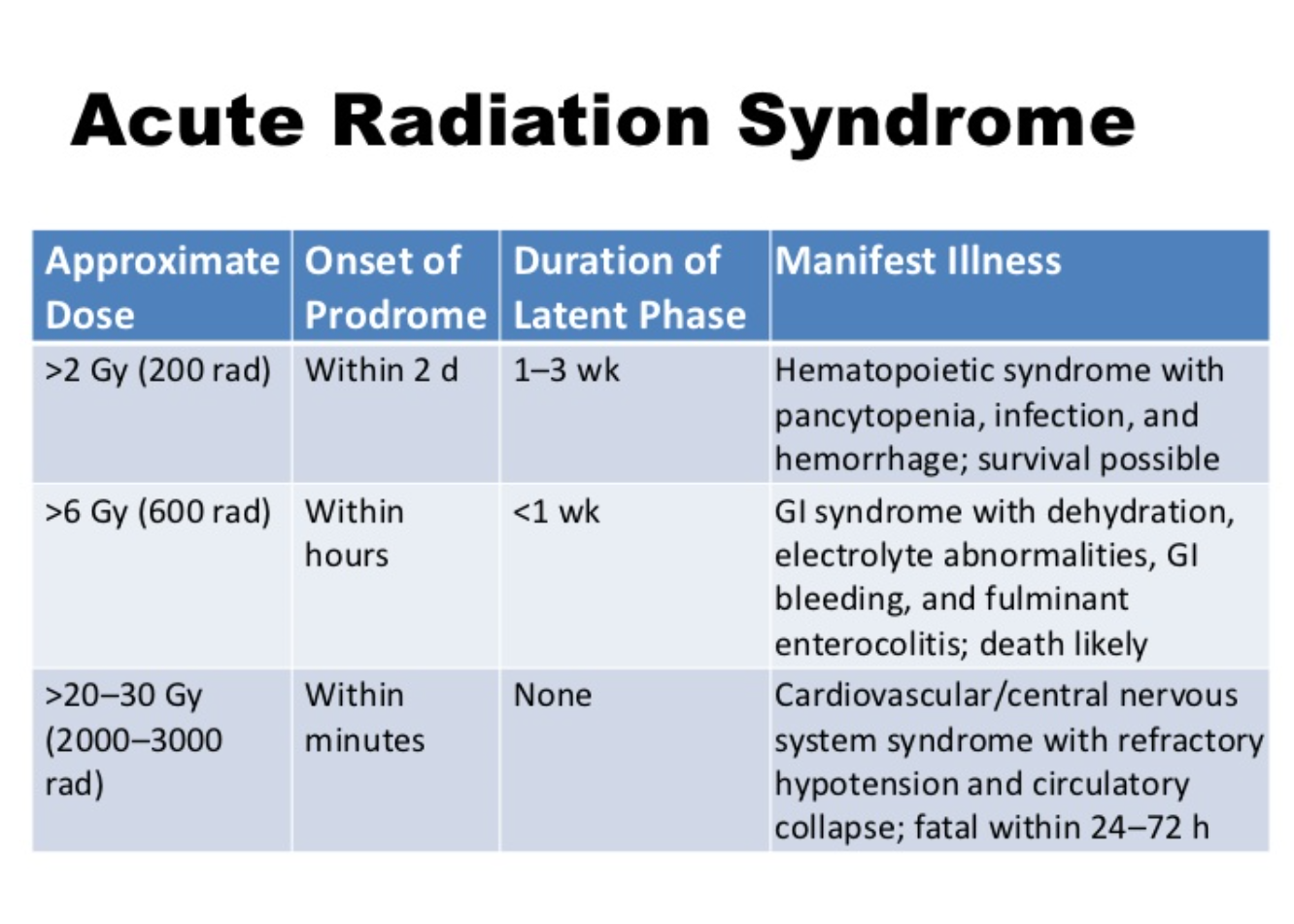
Dr. Regan discussed radiation physics. Here is my attempt at a descriptive analogy. Think of a Gray as 1 dollar. Think of a rad as a penny. There are 100 rads in a Gray. (100 pennies in a dollar). When a rad hits the body it is then measured as a miliseivert. Think of this as taking your dollar and bringing it to a currency exchange to purchase euros. 1 rad will buy 10miliseiverts. 300 rads or 3000 miliseiverts of radiation exposure is very dangerous. 600rads/6000 miliseiverts is almost always fatal.
Decontamination for radiation-exposed patients presenting to the ED is primarily removing their clothing and irrigating them with copious water. You then test them with a Geiger counter. They are OK to go into the hospital when you get their radiation down to 2X the ambient radiation level. You can also Geiger count their urine and a nasal swab to check for internal radiation. Nuclear Medicine Dept has Geiger counters. Get CBC’s on radiation-exposed patients every 2 hours. Personnel doing radiation decontamination have to be specially trained and wear a level C hazmat suit.
Classification of Blast Injuries
High Order explosives like TNT, C4, Semtex create a well-defined pressure wave and cause primary blast injuries. Low order explosives like pipe bombs do not create a well-developed pressure wave and don’t cause primary blast injuries.
Imaging of blast lung injury
Patients exposed to bomb blasts will develop lung finding relatively rapidly so you can order CXR or CT Chest early in ED course.
The lung is very susceptible to primary blast injury. Pulmonary barotrauma is the most common fatal primary blast injury and the most common critical injury in people close to the blast center. Pressure differentials across the alveolar–capillary interface can cause disruption, hemorrhage, pulmonary contusion, pneumothorax, hemothorax, pneumomediastinum, and subcutaneous emphysema…
In general, managing blast lung injury is similar to caring for pulmonary contusion and acute respiratory distress syndrome, except that early recognition of the syndrome may be complicated by initially benign symptoms, especially in the context of hectic mass casualty incident situations. Hypoxia is an almost universal finding.12 Monitoring of respiratory rate and room-air pulse oximetry, as well as serial chest radiographs, may be needed. Fluid administration should ensure tissue perfusion without volume overload... Keep tidal volume to 6 to 7 mL/kg ideal body weight to limit the peak inspiratory pressure and to minimize ventilator-induced lung barotrauma. Often, neuromuscular paralysis and early institution of pressure-limited ventilation (plateau pressures <30 cm H2O),13 with the lowest pressures compatible with adequate ventilation, may be the best strategy. Inverse inspiratory-to-expiratory ratio ventilation may be useful. Permissive hypercapnia is acceptable depending on cerebral perfusion pressure or increased intracranial pressure.13 Aggressive methods of oxygenation, such as extracorporeal membrane oxygenation or intravascular oxygenation, may become necessary within hours of the injury. (Tintinalli 8th edition)
Eydelman ECMO
ECMO is basically a placenta-like form of oxygenation for critically ill patients.
ECMO gained traction in adults for management of military blast injuries and treatment of fulminant lung injury due to influenza.
Veno-venous ECMO bypasses the lungs but the heart still pumps the blood.
Veno-Arterial ECMO bypasses the lung and the machine pumps the blood. V-A ECMO can perfuse in cardiac arrest.
The literature is not super strong in support of ECMO but it is trending toward better outcomes. A 2016 study showed 50% survival for out of hospital V-Fib arrest who received ECMO therapy.
There are some EM centers doing ECMO for selected cardiac arrest patients. You can also use ECMO for cardiogenic shock. Other indications: electrical storm, heart block, ARDS, severe tox cases, hypothermia/hyperthermia, and blast lung injury.
As emergency physicians, we can advocate on behalf of our patients for doing ECMO in select situations. This means consulting with ICU and CV surgery specialists in the appropriate clinical scenario.
Critical Care in the future may see ECMO replacing intubation and positive pressure ventilation. That is because positive pressure ventilation is so deleterious to patients.
Rehman 5 Slide F/U PCP Pneumonia
No patient details, just the take home lessons.
PCP is the most common opportunistic infection among AIDS patients.21 The causal agent is known as P. jirovecii (previously known as P. carinii). Approximately 70% of HIV-infected patients acquire PCP at some time during their illness, and PCP is often the initial opportunistic infection that establishes the diagnosis of AIDS. This infection is the most frequent serious complication of HIV infection in the United States and the most common identifiable cause of death in patients with AIDS. The classic presenting symptoms of PCP are fever, cough (typically nonproductive), and shortness of breath (progressing from being present only with exertion to being present at rest).
Symptoms are often insidious and accompanied by fatigue. Chest radiographs most often show diffuse interstitial infiltrates (Table 154-3), but negative radiographic findings exist in 15% to 25% of patients with PCP.22 The lactate dehydrogenase level is elevated in patients with PCP, but this test has low sensitivity and specificity, impairing utility. Arterial blood gas analysis usually demonstrates hypoxemia and an increase in the alveolar-arterial gradient. Suspect early PCP if a patient demonstrates a decrease in pulse oximetric values with exercise; even an ED "walk" can detect this exercise desaturation. Presumptive diagnosis of PCP is often made in the ED if there is hypoxemia without any other explanation. Inpatient diagnostics include bronchoscopy with specimen analyses.
Initial PCP therapy is trimethoprim-sulfamethoxazole (Table 154-2) PO or IV for 3 weeks (2 double-strength tablets three times daily). Adverse reactions, including rash, fever, and neutropenia, occur in up to 65% of AIDS patients. Pentamidine is an alternative agent (Table 154-2). Give steroids to patients with a partial pressure of arterial oxygen of <70 mm Hg or an alveolar-arterial gradient of >35 mm Hg, usually oral prednisone starting at 40 milligrams twice daily and tapering over 21 days (Table 154-2).
Seventy percent of patients have reinfection within 18 months; thus, prophylactic therapy is key. Oral trimethoprim-sulfamethoxazole, one double-strength tablet daily, is the preferred agent. Prophylaxis for all patients with CD4+ T-cell counts of <200 cells/mm3 is another common approach to mitigate PCP. Repeat PCP infections are often less responsive to therapy. (Tintinalli 8th edition)
Dr. Lovell comment: Dr. Triteman is an ID specialist here a ACMC who has a HIV Clinic. You can contact him to arrange follow up for newly diagnosed HIV patients who are stable for discharge.
Ahmad Five Slide F/U Back Pain
No patient details, just the take home lessons.
Bowel perforation from blunt abdominal trauma can present to the ED days after injury.
If a patient has bowel perforation from blunt abdominal trauma, you have to consider that the patient may have some underlying bowel pathology such as crohn’s or ulcerative colitis.