Pt is a 26 y/o G2P2 PPD #2 after an uncomplicated NSVD. Patient had been complaining of bilateral "ankle" pain and was evaluated for and given an extra dose of norco. The patients vital signs included tachycardia to 118 which persisted over a 4 hour period. A trial of a fluid bolus had been given by the resident despite adequate PO intake, for possible underestimated EBL. After 2L of LR the patient became slightly more tachycardiac and now was complaining of dyspnea.
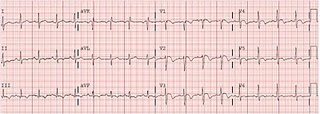
A CXR was obtained and was negative and B/L lower ext dopplers were obtained and were negative. Her EKG is included. Her vitals at the time of the EKG were 118, 22, 100/50, 36.9 and 95%.
WHAT DO YOU SEE??
The EKG finding that is most specific for acute PE is TWI in the anterior AND inferior leads. If there is TWI in lead III and in V1-V3 this is more suggestive of pulmonary embolus than acute cardiac ischemia.
The EKG was initially called non-specific ST and T wave changes, but after the patients tachycardia did not resolve a CT chest was obtained that showed bilateral pulmonary emboli.