This is a case from the other day I'm still not sure I completely understand and need some help from all of the briliant minds out there.
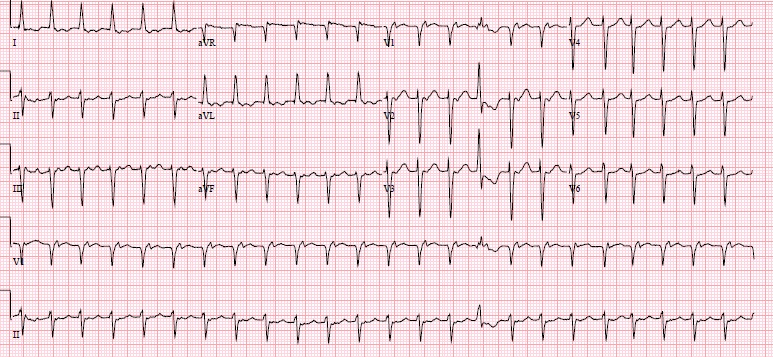
78F, under treatment for multiple myeloma, recently started on hemodialysis, COPD, DM, came to the hospital for an outpatient IR fistula procedure. She was sent to the ER for tachycardia, thought to be a-fib. Pt has had some epigastric tightness for a couple of days and some mild shortness of breath, but no palpitations or real chest pain. Initial EKG below:
Definately not a-fib (too regular, weird p-waves present, look at V1). A few thoughts went through our heads: AVNRT (retrograde P's), a-flutter (ventricular rate is almost exactly 150), SVT....
We went with a-flutter, started on diltiazem 10mg bolus, 5mg/hr drip.
Check on pt a bit later, rate in 80s. Yay, we fixed her! Let's get a repeat EKG!
Uh...WTF is this? Still not a-fib, P's march out regular with single morphology. Does not seem to be an association between Ps and QRS. 3rd degree heart block? Can't be, QRS is narrow so ventricular rhythm orignates above the AV node, also the rate is norma, no bradycardic. Is there a 2nd degree AV node block of some sort? The groupings of QRS complexes are regular.
Cardiologist in ED to see pt. Answer: Uh...WTF is this? Wenkebach? (sigh of relief I'm not the only one that can't figure it out). Let's get an EP consult
EP consult: Atrial tachycardia with AV block suggestive of Wenkebach periodicity. Neg P waves in lateral leads suggest atrial tachycardia, periodicity of QRS suggests Wenkbach
Some more info on Wenckebach:
2nd degree heart block, Mobitz type 1. PR interval gradually increases until there is a non-conducted P wave. P waves tend to be regular. QRS complexes are clustered, usuall in a consistent pattern (P:QRS of 3:2, 4:3, 5:4).
I still don't completely understand this EKG. If you have any thoughts, please comment on this post (click below, don't reply to email) for everyone to see and discuss.
View this video for some inspiration: http://www.youtube.com/watch?v=GVxJJ2DBPiQ
Louis
Update
on 2013-11-29 16:23 by Robert Harwod
Louie-->
Great case, but I'm not sure why you are feeling so out-of-sorts.
EKG#1: A.Flutter @ 143 (Atrial rate=286 best seen/not well in lead III) with a 2:1 block. If you are looking for A. flutter 2:1 block (i.e. regular tachycardia 140-160) look for flutter waves in inferior leads or V1/V2.
EKG#1: You got it! Go head & treat. You did with CCB!
CCB's slow can slow atrial rate & WILL increase AV block. This is why it works so we'll in slowing P.A.Fib & why we use it everyday. It works.
EKG#2: show group beating. Group beating is Wenkebach/type 2 block. 99.9% of the time this is 2nd AV block (0.01% it is SA nodal block, sometimes called Sinus exit block, which is grouped within sick sinus syndromes).
EKG#2: What's the p rate? Before meds it was flutter @ 286. Now it is 123. Could be sinus @ 123, but P wave configuration makes non-sinus atrial tachycardia @ 123.
EKG#2: Examining the lead V1 rhythm strip (2nd from bottom), you see QRS #1, then p#1 with drop (missing QRS). P#2/P#3 conducted with increasingly PR interval until another dropped beat. This 3:2 group beating 2nd HB/Wenkebach continues across the EKG. The is an isolated 4:3 group in the middle of the strip.
EKG#2: PAT with block (classic for dig toxicity, by the way). You got it!
If this was 2 pts with 2 EKG's, you'd be "good." Maybe your discomfort is these 2 EKG's in the same pt?
OK. So go back to the pt. ESRD on HD, MM, COPD. This pt is a train wreck. Even if her K+, Mg++, Ca++ & phos were normal in her serum, do you believe they are are perfect in her heart tissue? Her SA node? Her AV node? Then you give her an IV CCB. It does what it is supposed to do. It slows & blocks. Sherlock Holmes consult? Not really needed.
A final point about P.A.Flutter. This only rarely is a chronic condition; it seems like it is an inherently unstable rhythm. It usually ends up as chronic A. fib or sinus. What rhythm did she end up in with long-term?
-->Harwood