This 50 year old male presented to the ED folowing syncope. He had sudden onset of severe palpitations associated w/ throat fullness, diaphoresis and nausea. He had a syncopal episode at home and then presented to the ED.
Inital Triage VS:
HR 227
BP 124/86
RR 28
SpO2 100% RA
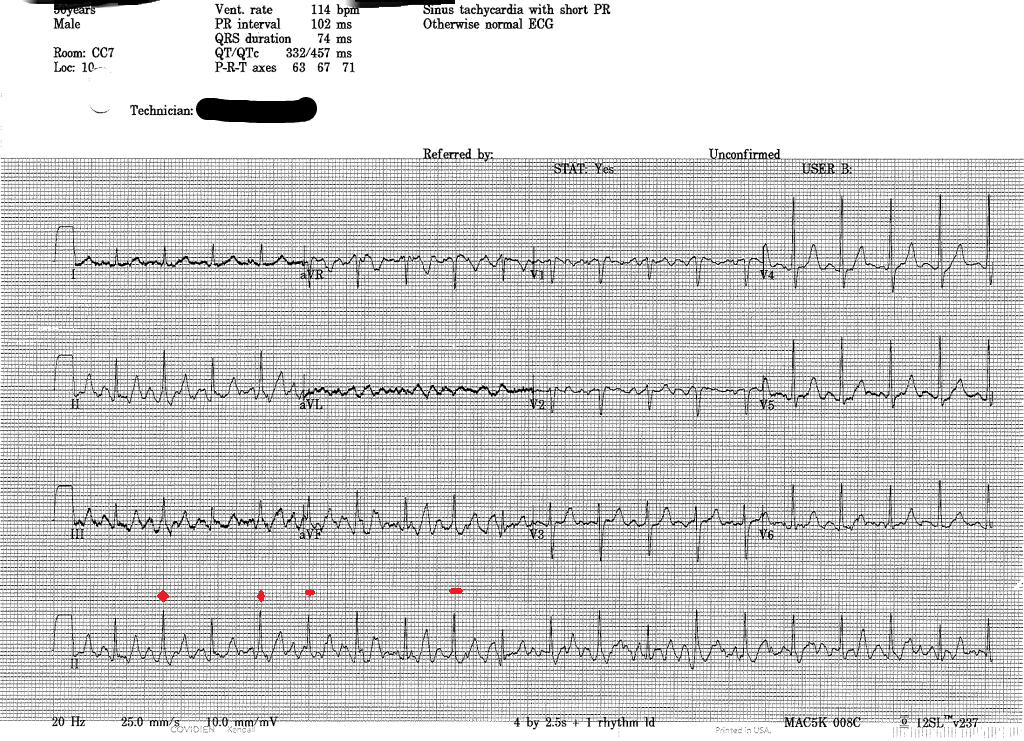
He's roomed immediately, here's the EKG
Very fast, irregular narrow complex tachycardia w/ varying QRS morphologies. Rhythm is atrial fibrillation, with some consecutive beats conducted at a rate of nearly 300 bpm (R-R interval 200 msec), which is nearly diagnositic for the prescence of an accessory pathway--the AV node simply cannot conduct that fast. Atrial Fibrillation w/ WPW, this is the one we train for.
The patient notes a history of Rheumatic Fever as a child, but no other medical problems and no recent stimulant or other drug use. On exam, he's awake and alert and appears uncomfortable and clutching his chest. He denies chest pain or shortness of breath, just very uncomfortable palpitations. On the monitor, there were frequent runs of nonsustained Wide complex beats concerning for immenient degeneration into Vfib.
Management options?
Adenosine?
No! Ineffective at best and could possibly cause increased conduction through the Accessory pathway
Rate Control?
No!
Medical Cardioversion?
Potentially an option for the stable patient. But this patient, while not meeting any of the strict criteria typically used to define 'unstable' in ACLS, was clearly electrically unstable. N.B. The two options typically listed for cardioversion are procainamide and amiodarone, however numerous case reports and been published showing increased ventricular response and even Vfib during infusion of amiodarone have been published, so best to stick w/ Procainamide.
Electrical Cardioversion?
Yes! Undoubtedly the fastest and most efficacious method, it's also probably the safest as well. We sedated the patient using etomidate and successfuly performed syncronized cardioversion w/ 200 J. Upon waking the patient reported complete relief of symptoms.
Post-Cardioversion EKG
A lot of motion artifact, but Sinus Tachycardia with a short PR interval w/ delta waves evident in some of the complexes. Interestingly, these were not seen on subsequent EKGs.