Hey guys,
Been a while, and have 2 more coming.
Superficial thrombophlebitis (ST), aka superficial vein thrombosis
--
Thrombosis of superficial veins has long been considered benign, and deemed a separate entity from venous thromboemolism (VTE)
-- However, multiple studies illustrate a significant association with VTE (DVT and PE).
-- When patient with ST (diagnosed clinically, no ultrasound) are thoroughly evaluated, the degree and the extent of clot are underestimated 75% of the time. Further, such patients are found to have co-existent DVT or PE 25% of the time and/or rapidly progress to DVT 10% of the time.
---- Teaching point: get ultrasounds on all clinical superficial thrombophlebitis
-- The risk factors for ST and VTE are the same, and many argue that ST should be treated the same as VTE.
-- In general,
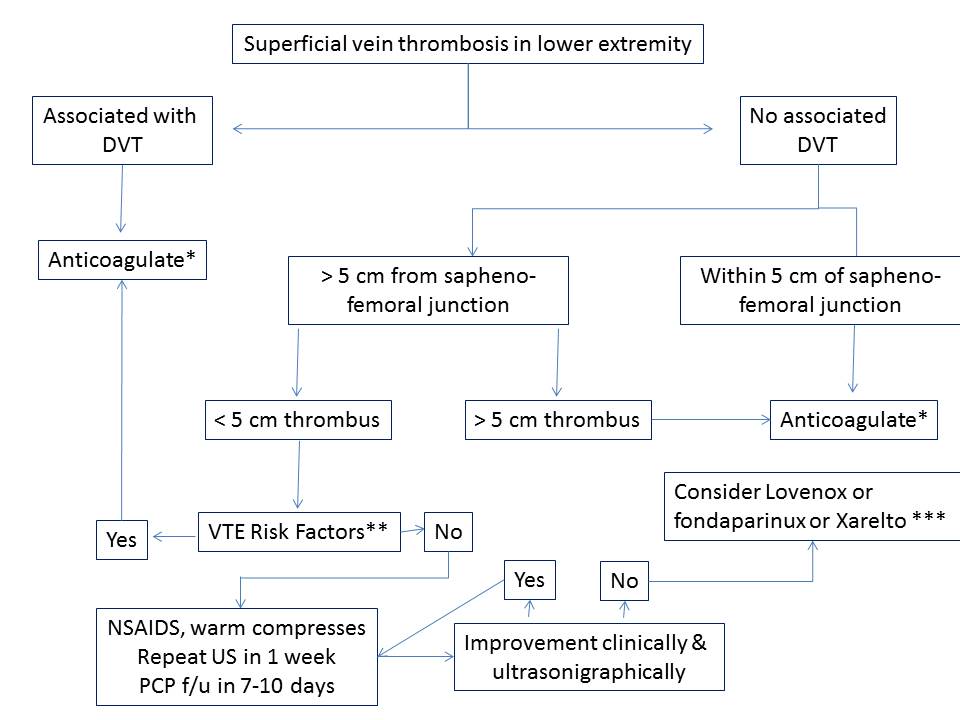
anticoagulate (as you would for DVT) the patient if they have known clotting risk factors, greater than 5 cm of clot, or clot < 5 cm within the sapheno-femoral or sapheno-popliteal junction.
-- Another way to think about it is that a superficial vein thrombosis is a manifestation of a systemic clotting cascade gone awry. To even further simplify things, seems pretty pathologic to have any blood vessel clot; ahh hello, you are clotting off blood vessels.
Below is my treatment algorithm on ST in the lower extremity.
Feedback always welcome.
Josh
References
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3278049/#
CHEST 2012 guidelines
Eur J Vasc Endovasc Surg 2005; 29:10-17.
J Vasc Surg 2003; 37:834-8.
Thromb Haemost 2001 ;86:452-63.
* Full anticoagulation with [a] lovenox 1 mg/kg BID (or 1.5 mg/kg QD) for at least 5 days and until coumadin is therapeutic for at least 24 hours. [b] Xarelto or rivaroxaban15 mg BID for the first 3 weeks, then 20mg daily for at least 3 months. If lifelong anticoagulation planned, would recommend lovenox/coumadin. 2nd reoccurrence consider lifelong anticoagulation but refer to CHEST guidelines for specific permutations. A study by Schulman found a second DVT indicated a need for lifelong anticoagulation and it didn’t matter whether the DVT was provoked or unprovoked. However, provoking factors vary in their risk of recurrence; surgery patients have the lowest risk of recurrence. Patients with unprovoked or idiopathic thrombosis or multiple recurrences with lower risk provoking factors will get long‐term anticoagulation.
** History of DVT or PE, active malignancy (recommend solely lovenox, d/w oncologist), hypercoagulable state. Other risk factors that warrant consideration of systemic anticoagulation include male gender without varicose veins, history of superficial thrombophlebitis, recent surgery, involvement of saphenous vein, and severe symptoms.
*** Lots of variability in dosing.
-- Lovenox: [a] 40 mg daily SC x 4 weeks per CHEST guidelines, [b] 1 mg/kg BID SC x 10 days then 1 mg/kg QD x 20 days per Belgian Society on Thrombosis and Haemostasis.
-- Fondaparinux 2.5 mg SC QD x 30-45 days
-- Xarelto – current trial comparing 10 mg PO QD vsfondaparinux. Xarelto approved for DVT. Would consider using if 1st time on anticoagulation given PO form and no need for INRs, but would discuss with PCP before committing to lifelong use of Xarelto.
****
Deep veins = superficial femoral vein, common femoral vein, deep femoral vein, popliteal vein, anterior tibial vein, posterior tibial vein, peroneal vein.
Superficial veins = Greater saphenous vein, small saphenous vein