23y/o F presents form EMS with "SEVERE ASTHMA". Patient is hypoxic satting 78% on 15L NRB in the rig. Patient is obtunded on presentation diaphoretic and cyanotic. Her sats are in the low 80s on an ambubag at this point.
What would you do?
This patient weighs approximatel 260lbs, and is clearly in distress. She is barely moving air and is extremely tight. Here's what we did: 4g magnesium, ambubag with PEEP valve and 2LNC for increasing PEEP. 150mg of IV ketamine and 2mg of IV versed. Ventilator to the bedside and get her sats up. With the NC and ambu bag sats come up to 100%, color returns patient is clearly anxious fighting and agitated, rather than obtunded now. She will NOT tolerate bipap.
Decision is made for intubation but she is obese. RAMP positioning (thanks dr. g), head is elevated 30 degrees. Nasal cannula is left on DURING the intubation as patient is RAPIDLY desaturating when the BVM is taken off face (she has no cardiopulmonary reserve, due to her intrinsic lung disease and reduced FRC). Patient gets an awake look(this was right after ketamine and versed were given) to see what airway looks like and after cords are visualized patient begins to gag, decision to push paralytics is made. Patient intubated and initial vent settings are!?
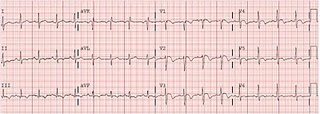
AC 8/450/100%/0
We are now hearing air move patient is no longer auto-peeping, she is not hypoxic and her end-tidal is about 70 on waveform capnography (dont forget to change settings to see the graph suually only goes as high as 50).
But about 6 minutes after paralytics are pushed patient is getting agitated here rr increase to 18 and her sats come down. her PCO2 begins to drop and her peak pressures SKY ROCKET to the 80s, clearly she is under sedated.
An insp hold for plateau pressure is completed and a sickening SIGH and wheeeze is heard from the ET tube as the patient expires all the auto peep. Boluses of fentanyl and versed are given while we attempt to paralyze patient with nimbex in order to gain complete control of resp status. BUTTT we cant give nimbex in the er because nurses are NOT trained apparently in this. So instead a bolus of rocuronium was given to buy time with high doses of propofol were given for sedation (BP was very elevated from sympathetic response).
Initial ABG after propofol and a push of rocuronium is: 7.0/102/406/25, clearly a resp acidosis.
We decide bicarb drip is the way to go and allow her to increase rate to 10 with repeat gas of
7.1/96/87/29 on AC 8/450/50%/5
In the ICU managemnet is continued with train of fours for sedation on nimbex, and patient is given heliox 20/80. Patient doing well much improved day one in ICU.