Conference Notes 10-15-2013
Another Great week of conference!
I will be taking three weeks off from doing Conference Notes due to a trip “Down Under”. Conference Notes will start back up the week of November 12th.
In the meantime, be safe out there, and be careful with sharps.
Walchuk/Urumov Oral Boards
Case 1. 37 yo woman who is 35 weeks pregnant presents with RUQ abdominal pain, hypertension, headache, and emesis. Patient had a prolonged seizure after initial evaluation. Diagnosis was Ecclampsia. Critical actions: IV Magnesium and Ativan to initially manage the seizure, IV hydralazine or labetalol for BP control, left lateral decubitus positioning to improve IVC flow, set up fetal monitoring, arrange for delivery.
Case2. 30 yo male hemophiliac presents with headache due to head injury from MVC. Diagnosis was hemorrhagic cerebral contusion . Critical actions: Give factor 8 prior to CT head, correct to 100% of factor 8 level (50u/kg of factor 8), Get CT head, consult hematology/neurosurgery, ICU admission. Andrej teaching point: You can also give FEIBA in this situation especially for patients with Factor 8 antibodies. More Andrej teaching points: Don’t delay administering factor 8 for any reason if a head bleed is in the differential. Gotta give the Factor 8 prior to sending patient for CT head. Easy way to remember Factor 8 dosing: Head bleeds need to correct to 100% so give 50 IU/kg. All other bleeds correct to 50% so give 25IU/kg.
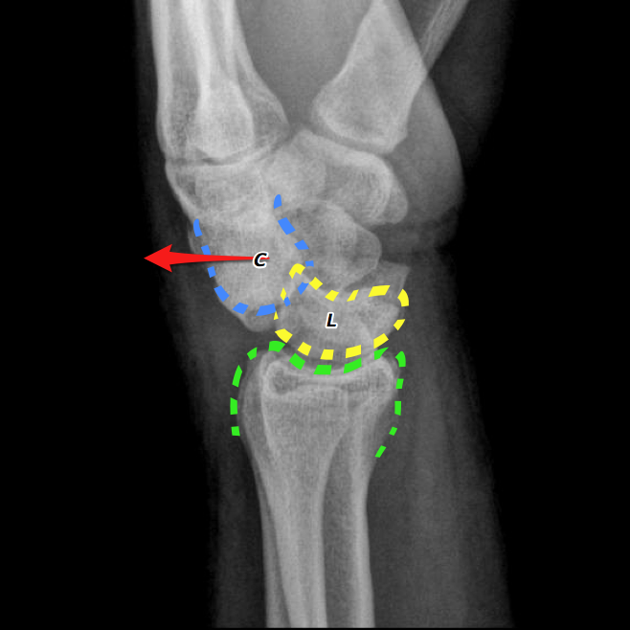
Case3. 38yo male fell from ladder and injured left wrist. Diagnosis was perilunate dislocation. Critical actions: Consult ortho for reduction, do complete neurovascular exam, administer pain medication. Andrej teaching points: One way to help differentiate a scapho-lunate dissociation and a perilunate dislocation is that in the scapho-lunate dissociation there will be no overlapping bones on the AP view. The perilunate and lunate dislocations will have overlapping bones on the AP view. Also use the lateral view to help figure out the radiographic diagnosis.
Scapholunate disociation (Terry Thomas sign/No overlapping bones, Arcs of Gilula are intact)


Perilunate dislocation (AP and Lateral Views, Gilula's Arcs not intact)

Girzadas Selection Committee Meeting
The Breakfast with the RLT lecture was discussed. Unfortunately no breakfast was provided at this lecture. :-) My Bad.
Lambert Aortic U/S
First thing to look for is the spine shadow. It’s your easiest landmark to identify in the transverse view. Aorta is anterior and left of spine. IVC is right and anterior to the spine. First branch off the aorta is the celiac trunk. Second branch off the aorta is the SMA.

You will need to apply slow steady pressure with the probe onto the abdomen to move away bowel gas . Angle the probe inferiorly slightly. Keep the indicator on the probe oriented to the right.
Differentiating the Aorta from the IVC; get transverse images first. Make sure the indicator on the probe is toward the patient’s right side. Look for arotic branch vessels. Look for color and pulse waves. Non-compressibility and thick walls favor aorta. Compressibility and thin walls favor IVC.
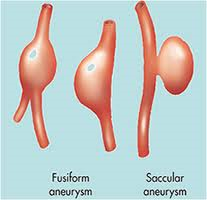
Transverse images will pick up both fusiform and saccular aneurysms. The longitudinal image can miss saccular aneurysms.
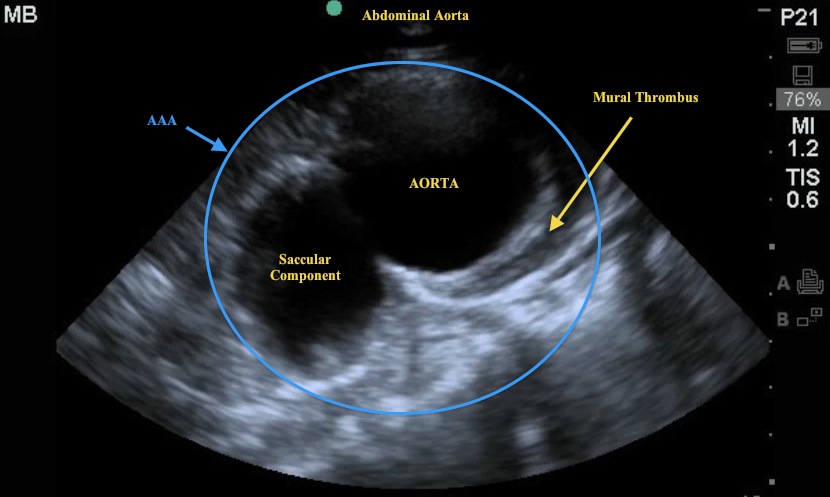
Hypodense round area within spine shadow is the spinal canal. Don’t confuse that with aorta.
Measure the aortic diameter from outer wall to outer wall using a transverse view. Longitudinal views may underestimate the true diameter of the aorta.
Mike said he never found a case where someone was looking for AAA and missed it. These usually are not subtle.
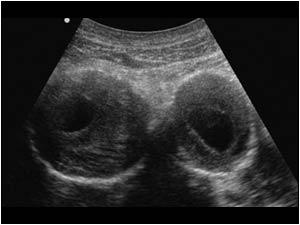
Iliac artery aneurysms can present as groin pain. All the iliac aneurysms Mike has found have been in octogenarians. If an older patient has groin pain, he scans down below the aortic bifurcation.
Bilateral iliac artery aneurysms
Tips for more difficult patients: Use liver as an acoustic window for proximal aorta. Apply firm steady pressure to compress bowel gas. You can try the decubitus position to displace bowel.
Lambert Cardiac U/S
Mike presented a case of a young adult patient presenting with weakness and hypotension. Echo showed pericardial effusion and plump aortic root (3.4cm). Maybe had some RV collapse. Pt responded to IV fluids. Pt went to CT and was found to have aortic dissection. Pt never had any pain. As noted in last week’s Conference Notes, Diagnosing aortic dissection is a bitch!
Bedside Echo changes the management of many patients.
Indications: cardiac arrest, near arrest, call an arrest, PE, pericardial effusion, tamponade, severe LV dysfunction, valvular heart disease.
Use the probe with a small footprint to get a sound beam between the ribs. The phase array probe has 2.5-3.5 frequency and gives you better contrast and has a high frame rate so you can see motion better.
B mode is brightness mode. M mode is motion mode. Basically, M mode drops an ice pick image through the bright mode image and shows that specific area repeatedly over time. With M mode you can measure fetal heart tones or mitral valve motion.
Standard Bedside Echo Images: Subcostal, parasternal, apical. Apical is the least important.
In subcostal view, start looking right at the liver under the right costal margin and then sweep medially. When Mike says sweep he doesn’t move the probe on the abdomen but angles the probe toward the left shoulder.
Parasternal Long view: Keep probe in the plane between the right shoulder and the left elbow. Mike said he doesn’t care if the indicator is oriented to the right shoulder or left elbow. In a heart with good contractility the LV wall and the septum should move pretty close together mid chamber and the mitral valve should come close to slapping the septum.
Parasternal long view probe positioning
Parasternal Short view: keep probe in the plane between the right shoulder and left elbow. Orient the probe indicator to the left shoulder.
PE on echo will have a proportionately larger RV than LV.
PE in a Parasternal Short Window. Note large RV in relation to normal size LV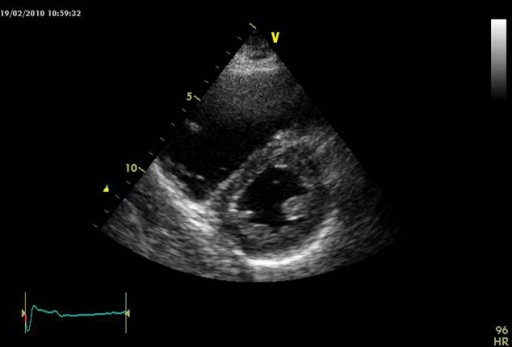
Lambert /Chastain/Chan/Villalba Aorta and Echo Scanning Workshop
Have a great week everyone!