Conference Notes 10-29-13
Today's guest for conference notes is Elise Lovell. Don't worry, only one more Tuesday until Dan's back.
Bonus, a tox lecture by alumni and tox fellow Janna Villano.
00 am Orbital Trauma/Oculoplastics-Dr. Hassan Shah; he’s happy to be involved with any Oculoplastics questions!
Ruptured Globe: How to tell? Peaked/irregular pupil, full hyphema, 360 degree subconjunctival hemorrhage, low IOP.
Most important reason to fix orbital fractures? Prevent diplopia.
What does optho need to know about intraocular foreign body? High pressure à systemic steroids. Ruptured or not ruptured. Visual acuity.
Blunt eye injury: “Blown pupil” actually not helpful to tell if optic nerve injured...can have temporary pupil dilation simply due to blunt injury. APD however IS a sign of optic nerve dysfunction. If APD, high pressure, loss of vision, need to perform lateral canthotomy/cantholysis. Dr. Shah believes cantholysis important; simple canthotomy usually not enough, and most common mistake is to think you’ve relieved the pressure but you haven’t done enough. He can fix any eyelid laceration that you cause!
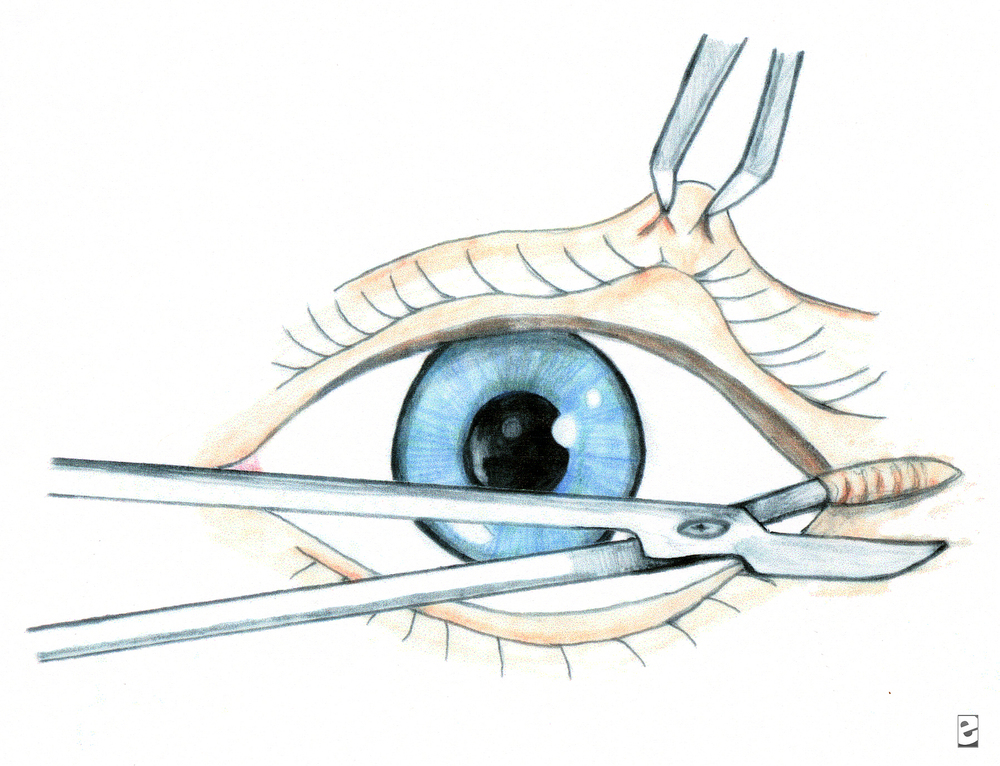
This is lateral canthotomy. You also need to cut up and down (3 total cuts) for complete cantholysis.
Be sure to cover the eye in the setting of eye trauma. Use ointment, try to bring lid back down over eye. Best covering for globe is the conjunctiva.
Blow out fractures. Adults almost never needs to be repaired emergently. Even if “entrapment”, usually due to soft tissue swelling. Usually wait for one week before repair to allow swelling to resolve. Big fractures much less likely to get true entrapment than small fractures. Big fractures = lots of swelling, but also room for movement. For kids, they get “greenstick” type fractures of the orbit; softer bones, the fracture is often very small, with mild swelling, but with restricted ROM up and down due to trapped muscle àthis is case for same day surgical repair. If you don’t have diplopia on Day 1, you will not develop it!
Facial fractures and antibiotics: He doesn’t usually give antibiotics unless contralateral sinus disease, but there is controversy, not one correct answer. He has never had an infection.
9:00 am Janna Villano: - Tox-Uses of Sodium bicarb, and some controversial Antidotes
Most important 4 things in Tox: Vital signs, Mental Status, Skin and Neuro exam
Many Sodium Channel blockers out there: TCAs, cocaine, some antiepileptics, dysrhythmics...lots of others.
3 Uses for Sodium Bicarb: Cardio toxicity, Prevent acidosis, Urinary alkalinization
Bicarb: Treat cardiotox: helps with prolonged QRS, wide complex tachycardia, hypotension. Give 1 to 2 meq/kg bolus over 1-2 minutes. Boluses better than infusions. Give boluses and sit there watching for QRS to narrow.
Bicarb: Prevention of academia: maintain pH >/= 7.4. Prevents drug distribution, may be useful peri-intubation of tox patients.
Bicarb: Urinary alkalinization: enhances elimination. Maintain pH 7-8.5, ion trapping, must maintain normal K levels for this to work-aggressive K replacement!
Anticholinergics: antihistamines, TCAs, vertigo meds, antipsychotics, Jimson weed...etc.
Physostigmine: To treat anticholinergic toxicity. Will allow history when patient’s mental status clears. Should see nearly complete resolution of symptoms in order to attribute presentation to anticholinergic toxicity. Allows diagnosis, limits workup. Can cause seizures, GI distress/rest of cholinergic symptoms. Reports of physostigmine associated with cardiac arrest , but these in patients with TCA OD, also cases of seizure in patients with prior seizure disorder. If giving physo, watch for bradycardia/heart block, seizure, cholinergic side effects. Give 0.5 mg over 2-5 minutes, may repeat up to 3-4 doses. If necessary can “reverse” physo with atropine. ***Janna doesn’t give in patients with known seizure disorder, patient who took pro-convulsant, or patients with sodium blocker OD (eg TCA)***
Flumazenil: Don’t use drug screen to help you decide whether or not to give it-drug screen misses many benzos. Some studies have shown avoidance of intubation. Why not to use it in a documented benzo OD? Inconsistent clinical response, precipitation of benzo withdrawal (rare, and can give benzos), may precipitate seizures (seen in pts who took proconvulsant, or in patients using benzos for sz disorder), maybe risk of complications outweighs harm from OD.
Pick the right patient-no seizure disorder, pro-convulsant use, not if chronic benzo users, not for undifferentiated coma or prophylactically. Often used in kids, pure benzo OD, procedural sedation. If patient has seizure after flumazenil, then just flood patient with benzos (competive inhibitor).
10:00 am Dr. Khatiyar- Chemical Asphyxiants
Fires: Simple Asphyxiants, Chemical Asphyxiants, Chemical Irritants
Carbon Monoxide: from partial combustion: broken furnace, blocked car or boat exhaust, grilling in a garage, heating homes with gas ovens, car idling in garage...etc. Also from Methylene Chloride, in degreasers/lacqueer thinner, bathrub refinishesàmetabolized to CO.
CO toxicity: high affinity for hemoglobin forming CO-Hgb, but there are other toxic effects as well. Also binds to myoglobin (heart tox, rhabdo), direct organ toxicity due to increased NO production and lipid peroxidation. CO attachment to cytochrome oxidase (inhibits aerobic metabolism)
Think about it in headaches, “flu” in the fall when heaters turned on, kids with “colic”., gastro, viral syndrome, ..great imitator.
Diagnosis depends on a great history. Ask about recurrent sx, others at home with same sx, time of year, in setting of Headache, flu sx, “hangover” symptoms, chest pain, neuro sx.
Diagnosis: Breath sampling, CO level: VENOUS just as good as ARTERIAL blood gas. Don’t use O2 sat! Check renal function, pregnancy test as changes management dramatically. CPK, cardiac monitoring. CO levels also can be unreliable, depending on treatment with O2, time since ingestion. Levels: < 10% no biggie, > 50% likely fatal, everything in between open to discussion.
Delayed neuro sequelae: days to weeks later, incidence variable (1% - 47%), needs cognitive testing (think mini mental status) and re-testing on followup.
Red flags: pregnant women, kids, cardiac patients.
Half life 4-6 hours on room air, 60-90 minutes on 100% O2, 20 minutes with HBO.
Treatment: HBO controversial: but if level > 25%, any neuro issues/syncope, coma, Cardiac sx, abnormal cerebellar exam, symptomatic pregnancy or pregnancy with fetal distress à call HBO chamber and discuss with specialist. Put patient on 100% O2 as soon as you suspect CO. Local chambers: Advocate Lutheran General or Loyola, LCOM, Illinois Masonic, others.
Cyanide: neuro sx, acidosis, seizures. House fires, burning plastics, Nipride (sodium nitroprusside), certain foods-cassava, apple seeds, fruit pits, Laetrile.
Toxicity: Neurotoxin, Enhances NDMA receptor activity, inhibits aerobic energy metabolism (blocks cytochrome oxidase).
Diagnosis: Symptoms between 3 – 24 hours if oral, few minutes with gas exposure, sicker with premorbid conditions, kids, and dose dependent.
Presentation: LOC/AMS, metabolic acidosis, GI, SOB, CV instability. Be worried with rapidly developing coma, lactic acidosis, CV instability, symptomatic industrial worker/chemist.
Treatment: decontamination (clothing, skin decon), 100% O2. Old antidote: Lilly cyanide antidote kit (amyl nitrate, sodium nitrite to cause methemoglobinemia which will bind cyanide, sodium thiosulfate to form thiocyanate which will be excreted in urine). This kit usually available in ED, and this toxicity very time sensitive. Cons: causes hypotension, methemoglobinemia, multiple steps.
New antidote: Hydroxocobalamin binds with cyanide, conversion to cyanocobalamin (vitamin B12): safe, no methemoglobinemia, no hypotension, can penetrate to tissues. Does cause flushing./urine discoloration. Will mess up color change sensitive testing for hours. Not available in ED but we have it in pharmacy.
11:00 am : Dr. W.A. Bret Negro - Cold Weather exposure/Hypothermia:
Core Temp < 35 degrees
Causes: exposure, EtOH, sepsis, burns, massive resuscitation, metabolic problems (low sugar, low thyroid/adrenal), CNS causes
Mild > 34 degrees: shivering, “responsive” stage, trying to generate/maintain heat
Mod 30-34 degrees: depressed CV function, stupor, afib with slow ventricular response is classic
Severe < 30 degrees: low BP, no shivering, coma
Cardiac tox: sinus tach àsinus bradycardia à slow afib à vfib/asystole. Heart very sensitive, can cause dysrhythmias with central line placement and tip in heart/rough handling of patient. Also less responsive to ACLS meds/electricity. Shock once if T < 30 C, then just remarm until T > 30 before shocking again or giving drugs. May want to extend intervals between drug dosing. ECG Osborn wave.
Respiratory depression, messed up ABG values-to keep simple just treat as normothermic when making vent decisions.
Metabolic cold diuresis, rhabdo, ARF, hypokalemia from ion shifts (don’t over correct), pancreatitis, CNS alteration.
Treatment: remove from environment, dry patient. Take your time finding a pulse, may be extremely bradycardic. Don’t start CPR unless absolutely necessary due to cardiac irritability. Warm fluids (can warm IVF in microwave), warm O2, forced air blanket, Arctic Sun vest/Alsius Icycath central line devices (same devices used to cool patients, but set for warming). Warm gastric lavage, DPL, Foley fluids, 2 chest tubes with warm fluids, Bypass or thoracotomy as last resorts.
Rewarming shock: external heat àperipheral dilation, relative hypovolemia and hypotension.
No firm guidelines on treatment.
Non-freezing cold weather injuries: Trench Foot in military, direct injury to soft tissues, blistering/anesthesia, treat with heat/dry feet. Prevent with dry socks/well fitting boots. Chilblains/pernio: kids, Raynaud’s, uncomfortable inflammatory lesions of skin by longterm intermittent exposure to damp/nonfreezing ambient temp. Hands/ears/toes. Panniculitis: mild necrosis of subcut fat. Cold urticaria-sensitivity.
Freezing injuries: Frostbite, usually < 4 degrees F, frozen tissue, most damage from endothelial damage during thawing. Clinical diagnosis, warm them up and AVOID RE-FREEZING. No rubbing-will cause more damage. Also do not re-warm out of hospital. Aloe, NSAIDS, tetanus, no antibiotics. TPA after rewarming to reduce digit amputation. Heparin/HBO don’t work. Amputations delayed until final demarcation.
11:30 am: Dr. Dennis Ryan – MSK Study Guide
Too much fun to take notes
00 am Orbital Trauma/Oculoplastics-Dr. Hassan Shah; he’s happy to be involved with any Oculoplastics questions!
Ruptured Globe: How to tell? Peaked/irregular pupil, full hyphema, 360 degree subconjunctival hemorrhage, low IOP.
Most important reason to fix orbital fractures? Prevent diplopia.
What does optho need to know about intraocular foreign body? High pressure à systemic steroids. Ruptured or not ruptured. Visual acuity.
Blunt eye injury: “Blown pupil” actually not helpful to tell if optic nerve injured...can have temporary pupil dilation simply due to blunt injury. APD however IS a sign of optic nerve dysfunction. If APD, high pressure, loss of vision, need to perform lateral canthotomy/cantholysis. Dr. Shah believes cantholysis important; simple canthotomy usually not enough, and most common mistake is to think you’ve relieved the pressure but you haven’t done enough. He can fix any eyelid laceration that you cause!

This is lateral canthotomy. You also need to cut up and down (3 total cuts) for complete cantholysis.
Be sure to cover the eye in the setting of eye trauma. Use ointment, try to bring lid back down over eye. Best covering for globe is the conjunctiva.
Blow out fractures. Adults almost never needs to be repaired emergently. Even if “entrapment”, usually due to soft tissue swelling. Usually wait for one week before repair to allow swelling to resolve. Big fractures much less likely to get true entrapment than small fractures. Big fractures = lots of swelling, but also room for movement. For kids, they get “greenstick” type fractures of the orbit; softer bones, the fracture is often very small, with mild swelling, but with restricted ROM up and down due to trapped muscle àthis is case for same day surgical repair. If you don’t have diplopia on Day 1, you will not develop it!
Facial fractures and antibiotics: He doesn’t usually give antibiotics unless contralateral sinus disease, but there is controversy, not one correct answer. He has never had an infection.
9:00 am Janna Villano: - Tox-Uses of Sodium bicarb, and some controversial Antidotes
Most important 4 things in Tox: Vital signs, Mental Status, Skin and Neuro exam
Many Sodium Channel blockers out there: TCAs, cocaine, some antiepileptics, dysrhythmics...lots of others.
3 Uses for Sodium Bicarb: Cardio toxicity, Prevent acidosis, Urinary alkalinization
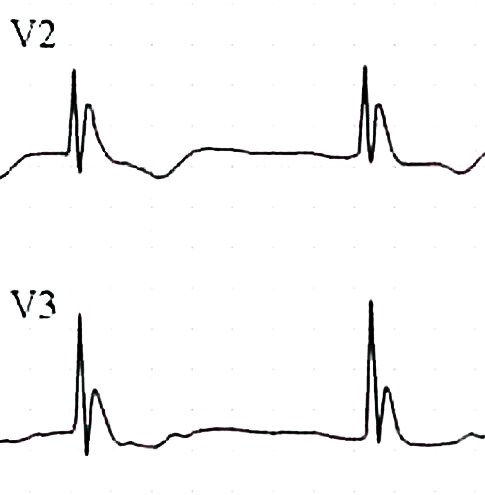
Bicarb: Treat cardiotox: helps with prolonged QRS, wide complex tachycardia, hypotension. Give 1 to 2 meq/kg bolus over 1-2 minutes. Boluses better than infusions. Give boluses and sit there watching for QRS to narrow.
Bicarb: Prevention of academia: maintain pH >/= 7.4. Prevents drug distribution, may be useful peri-intubation of tox patients.
Bicarb: Urinary alkalinization: enhances elimination. Maintain pH 7-8.5, ion trapping, must maintain normal K levels for this to work-aggressive K replacement!
Anticholinergics: antihistamines, TCAs, vertigo meds, antipsychotics, Jimson weed...etc.
Physostigmine: To treat anticholinergic toxicity. Will allow history when patient’s mental status clears. Should see nearly complete resolution of symptoms in order to attribute presentation to anticholinergic toxicity. Allows diagnosis, limits workup. Can cause seizures, GI distress/rest of cholinergic symptoms. Reports of physostigmine associated with cardiac arrest , but these in patients with TCA OD, also cases of seizure in patients with prior seizure disorder. If giving physo, watch for bradycardia/heart block, seizure, cholinergic side effects. Give 0.5 mg over 2-5 minutes, may repeat up to 3-4 doses. If necessary can “reverse” physo with atropine. ***Janna doesn’t give in patients with known seizure disorder, patient who took pro-convulsant, or patients with sodium blocker OD (eg TCA)***
Flumazenil: Don’t use drug screen to help you decide whether or not to give it-drug screen misses many benzos. Some studies have shown avoidance of intubation. Why not to use it in a documented benzo OD? Inconsistent clinical response, precipitation of benzo withdrawal (rare, and can give benzos), may precipitate seizures (seen in pts who took proconvulsant, or in patients using benzos for sz disorder), maybe risk of complications outweighs harm from OD.
Pick the right patient-no seizure disorder, pro-convulsant use, not if chronic benzo users, not for undifferentiated coma or prophylactically. Often used in kids, pure benzo OD, procedural sedation. If patient has seizure after flumazenil, then just flood patient with benzos (competive inhibitor).
10:00 am Dr. Khatiyar- Chemical Asphyxiants
Fires: Simple Asphyxiants, Chemical Asphyxiants, Chemical Irritants
Carbon Monoxide: from partial combustion: broken furnace, blocked car or boat exhaust, grilling in a garage, heating homes with gas ovens, car idling in garage...etc. Also from Methylene Chloride, in degreasers/lacqueer thinner, bathrub refinishesàmetabolized to CO.
CO toxicity: high affinity for hemoglobin forming CO-Hgb, but there are other toxic effects as well. Also binds to myoglobin (heart tox, rhabdo), direct organ toxicity due to increased NO production and lipid peroxidation. CO attachment to cytochrome oxidase (inhibits aerobic metabolism)
Think about it in headaches, “flu” in the fall when heaters turned on, kids with “colic”., gastro, viral syndrome, ..great imitator.
Diagnosis depends on a great history. Ask about recurrent sx, others at home with same sx, time of year, in setting of Headache, flu sx, “hangover” symptoms, chest pain, neuro sx.
Diagnosis: Breath sampling, CO level: VENOUS just as good as ARTERIAL blood gas. Don’t use O2 sat! Check renal function, pregnancy test as changes management dramatically. CPK, cardiac monitoring. CO levels also can be unreliable, depending on treatment with O2, time since ingestion. Levels: < 10% no biggie, > 50% likely fatal, everything in between open to discussion.
Delayed neuro sequelae: days to weeks later, incidence variable (1% - 47%), needs cognitive testing (think mini mental status) and re-testing on followup.
Red flags: pregnant women, kids, cardiac patients.
Half life 4-6 hours on room air, 60-90 minutes on 100% O2, 20 minutes with HBO.
Treatment: HBO controversial: but if level > 25%, any neuro issues/syncope, coma, Cardiac sx, abnormal cerebellar exam, symptomatic pregnancy or pregnancy with fetal distress à call HBO chamber and discuss with specialist. Put patient on 100% O2 as soon as you suspect CO. Local chambers: Advocate Lutheran General or Loyola, LCOM, Illinois Masonic, others.
Cyanide: neuro sx, acidosis, seizures. House fires, burning plastics, Nipride (sodium nitroprusside), certain foods-cassava, apple seeds, fruit pits, Laetrile.
Toxicity: Neurotoxin, Enhances NDMA receptor activity, inhibits aerobic energy metabolism (blocks cytochrome oxidase).
Diagnosis: Symptoms between 3 – 24 hours if oral, few minutes with gas exposure, sicker with premorbid conditions, kids, and dose dependent.
Presentation: LOC/AMS, metabolic acidosis, GI, SOB, CV instability. Be worried with rapidly developing coma, lactic acidosis, CV instability, symptomatic industrial worker/chemist.
Treatment: decontamination (clothing, skin decon), 100% O2. Old antidote: Lilly cyanide antidote kit (amyl nitrate, sodium nitrite to cause methemoglobinemia which will bind cyanide, sodium thiosulfate to form thiocyanate which will be excreted in urine). This kit usually available in ED, and this toxicity very time sensitive. Cons: causes hypotension, methemoglobinemia, multiple steps.
New antidote: Hydroxocobalamin binds with cyanide, conversion to cyanocobalamin (vitamin B12): safe, no methemoglobinemia, no hypotension, can penetrate to tissues. Does cause flushing./urine discoloration. Will mess up color change sensitive testing for hours. Not available in ED but we have it in pharmacy.
11:00 am : Dr. W.A. Bret Negro - Cold Weather exposure/Hypothermia:
Core Temp < 35 degrees
Causes: exposure, EtOH, sepsis, burns, massive resuscitation, metabolic problems (low sugar, low thyroid/adrenal), CNS causes
Mild > 34 degrees: shivering, “responsive” stage, trying to generate/maintain heat
Mod 30-34 degrees: depressed CV function, stupor, afib with slow ventricular response is classic
Severe < 30 degrees: low BP, no shivering, coma
Cardiac tox: sinus tach àsinus bradycardia à slow afib à vfib/asystole. Heart very sensitive, can cause dysrhythmias with central line placement and tip in heart/rough handling of patient. Also less responsive to ACLS meds/electricity. Shock once if T < 30 C, then just remarm until T > 30 before shocking again or giving drugs. May want to extend intervals between drug dosing. ECG Osborn wave.

Respiratory depression, messed up ABG values-to keep simple just treat as normothermic when making vent decisions.
Metabolic cold diuresis, rhabdo, ARF, hypokalemia from ion shifts (don’t over correct), pancreatitis, CNS alteration.
Treatment: remove from environment, dry patient. Take your time finding a pulse, may be extremely bradycardic. Don’t start CPR unless absolutely necessary due to cardiac irritability. Warm fluids (can warm IVF in microwave), warm O2, forced air blanket, Arctic Sun vest/Alsius Icycath central line devices (same devices used to cool patients, but set for warming). Warm gastric lavage, DPL, Foley fluids, 2 chest tubes with warm fluids, Bypass or thoracotomy as last resorts.
Rewarming shock: external heat àperipheral dilation, relative hypovolemia and hypotension.
No firm guidelines on treatment.
Non-freezing cold weather injuries: Trench Foot in military, direct injury to soft tissues, blistering/anesthesia, treat with heat/dry feet. Prevent with dry socks/well fitting boots. Chilblains/pernio: kids, Raynaud’s, uncomfortable inflammatory lesions of skin by longterm intermittent exposure to damp/nonfreezing ambient temp. Hands/ears/toes. Panniculitis: mild necrosis of subcut fat. Cold urticaria-sensitivity.
Freezing injuries: Frostbite, usually < 4 degrees F, frozen tissue, most damage from endothelial damage during thawing. Clinical diagnosis, warm them up and AVOID RE-FREEZING. No rubbing-will cause more damage. Also do not re-warm out of hospital. Aloe, NSAIDS, tetanus, no antibiotics. TPA after rewarming to reduce digit amputation. Heparin/HBO don’t work. Amputations delayed until final demarcation.
11:30 am: Dr. Dennis Ryan – MSK Study Guide
Too much fun to take notes