Conference Notes 3/19
Conference Notes 3-19-2013
Please consider donating to our EM Foundation to benefit resident education/development. Thanks for your consideration/generosity.
/em-foundation/
Badillo Ultrasound
Sorry, I missed this lecture.
Lovell Study Guide Sedation/Analgesia/Local anesthetic
5 ways to decrease the pain of local infiltration of anesthetic: small guage needle (Harwood uses insulin syringe initially followed by larger meeting), bicarb buffering, warm the anesthetic (Anneken method: put it on the computer CPU at the beginning of your shift),inject anesthetic into the wound not through intact skin, slow injection.
Etomidate causes myoclonus up to 30% of the time when used for sedation/induction.
Toxicity of local anesthetics is CNS toxicity (paresthesias followed by seizures) early followed by cardiovascular toxicity (arrhythmias). Bupivicaine is a great local anesthetic but has the highest risk for toxicity. Treat seizures with benzos and treat arrhythmias with amidarone. There is also some case reports on lipid infusions for local anesthetic toxicity. It has been very effective in some case reports. Risk for local anesthetic toxicity is greater in kids so be careful of dosing and risk also higher if you accidentally inject into an artery/arteriole.
Sedation levels: Minimal (anxiolysis), moderate (airway reflexes intact), deep (airway reflexes may not remain intact), general anesthesia (airway and cardiovascular issues).
- Analgesia – Relief of pain without intentionally producing a sedated state. Altered mental status may occur as a secondary effect of medications administered for analgesia.
- Minimal sedation – The patient responds normally to verbal commands. Cognitive function and coordination may be impaired, but ventilatory and cardiovascular functions are unaffected.
- Moderate sedation and analgesia – The patient responds purposefully to verbal commands alone or when accompanied by light touch. Protective airway reflexes and adequate ventilation are maintained without intervention. Cardiovascular function remains stable.
- Deep sedation and analgesia – The patient cannot be easily aroused, but responds purposefully to noxious stimulation. Assistance may be needed to ensure the airway is protected and adequate ventilation maintained. Cardiovascular function is usually stable.
- General anesthesia – The patient cannot be aroused and often requires assistance to protect the airway and maintain ventilation. Cardiovascular function may be impaired.
- Dissociative sedation – Dissociative sedation is a trance-like cataleptic state in which the patient experiences profound analgesia and amnesia, but retains airway protective reflexes, spontaneous respirations and cardiovascular stability. (up to date)
EMLA is an acronym for eutectic mixture of local anesthetics.
Simple rule: If you want to be cautious, Patient to be sedated should be NPO for 3 hours for any liquid or solid. If situation is emergent/urgent, you can shorten that time period. It is controversial whether NPO status does anything to protect patient from aspiration.
Safe dosing for : Lidocaine 4mg/kg plain/7mg/kg with epi Bupivicaine 3mg/kg plain/5 mg/kg with epi
Can’t use nitrous oxide (NO) in patients with high oxygen requirement, SBO, pneumothorax, altered mental status. Nitrous oxide will expand gasses in closed spaces. Pt’s need normal mental status to cooperate with NO sedation. Balloon tipped catheters in the body may also expand with the use of NO.
Oral opioids in increasing order of strength: Codeine, morphine, hydrocodone, oxycodone, hydromorphine. Harwood comment: 100micrograms of fentanyl=1.5mg of dilaudid. 25microgram doses of fentanyl are too small. Start with 1microgram/kg of fentanyl as a rule of thumb.
Complex regional pain syndrome: Pt s/p traumatic injury who is getting worse a couple of weeks later. Painful area may be edematous, allodynia present, diaphoretic, possibly mildly erythematous. Treat by removing cast, low dose steroids, better pain control, consult orthopedist/trauma.
Benzocaine (hurricane spray, teething gel) and prilocaine can cause methemoglobinemia.
There is research showing that you can treat benign headache with local injections 2 cm bilat laterally to C7, 2 cm deep. Use 1.5 ml of bupivicaine with each injection. (65% effectiveness for complete resolution of pain)
Abstract:
OBJECTIVE: The primary objective of this retrospective chart review is to describe 1 year's experience of an academic emergency department (ED) in treating a wide spectrum of headache classifications with intramuscular injections of 0.5% bupivacaine bilateral to the spinous process of the lower cervical vertebrae. BACKGROUND: Headache is a common reason that patients present to an ED. While there are a number of effective therapeutic interventions available for the management of headache pain, there clearly remains a need for other treatment options. The intramuscular injection of 1.5 mL of 0.5% bupivacaine bilateral to the sixth or seventh cervical vertebrae has been used to treat headache pain in our facility since July 2002. The clinical setting for the study was an academic ED with an annual volume of over 75,000 patients. METHODS: We performed a retrospective review of over 2805 ED patients with the discharge diagnosis of headache and over 771 patients who were coded as having had an anesthetic injection between June 30, 2003 and July 1, 2004. All adult patients who had undergone paraspinous intramuscular injection with bupivacaine for the treatment of their headache were gleaned from these 2 larger databases and were included in this retrospective chart review. A systematic review of the medical records was accomplished for these patients. RESULTS: Lower cervical paraspinous intramuscular injections with bupivacaine were performed in 417 patients. Complete headache relief occurred in 271 (65.1%) and partial headache relief in 85 patients (20.4%). No significant relief was reported in 57 patients (13.7%) and headache worsening was described in 4 patients (1%). Overall a therapeutic response was reported in 356 of 417 patients (85.4%). Headache relief was typically rapid with many patients reporting complete headache relief in 5 to 10 minutes. Associated signs and symptoms such as nausea, vomiting, photophobia, phonophobia, and allodynia were also commonly relieved. CONCLUSION: Our observations suggest that the intramuscular injection of small amounts of 0.5% bupivacaine bilateral to the sixth or seventh cervical spinous process appears to be an effective therapeutic intervention for the treatment of headache pain in the outpatient setting.
Citation:
Treatment of headaches in the ED with lower cervical intramuscular bupivacaine injections: a 1-year retrospective review of 417 patients.
Mellick LB - Headache - 01-OCT-2006; 46(9): 1441-9
MEDLINE® is the source for the citation and abstract of this record
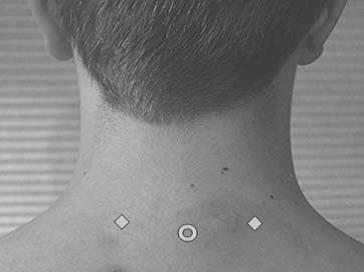 Diamonds are location of injections. Circle is the spinous process.
Diamonds are location of injections. Circle is the spinous process.
Carlson Oral Board Test Review
Case 1: Shaken Baby syndrome with bilat subdurals. Crtitical actions: CT head, get CXR/identify rib fractures, say abuse, take custody of child, consult neurosurgery for subdurals. A lot of residents missed skin exam showing trauma.
Case 2: Complex orthopedic injury with posterior elbow dislocation and lis-franc fracture dlx. Elise comment: nice video youtube by Gromis/Fakhori on how to reduce elbow dislocation. http://www.youtube.com/watch?v=mlAOGgocRnk
Case 3: Acute aortic dissection. Critical actions are: appropriate imaging studies, make diagnosis, control BP and tachycardia (labetalol, nitroprusside with esmolol), and consult vascular surgery. Giving ASA in this case for chest pain is a dangerous action. Dissections involving the ascending aorta are surgical.
Case 4: Kawasaki DZ. Critical actions are: Say Kawasaki, obtain CBC, start ASA, discuss need for IVIG, admit patient. Cardiac involvement with coronary artery aneurysms starts around 1 week of illness. Criteria for Kawasaki’s: Fever for 5 days, conjunctivitis, mucous membrane changes, cervical lymphadenopathy, rash, involvement of fingers/toes with swelling/rash.
Case 5: Testicular Torsion. Common pitfalls were not doing GU exam, and not giving prompt pain medication. Trosion can occur any time during life. 2 peaks: first year and adolescence. Recent EM Rap said don’t do U/S for torsion, go right to surgery. For the boards and probably real life, do an U/S prior to sending patient to OR. Harwood comment: EM Rap is not a peer-reviewed publication. They are giving a lot of opinion. As a practicing EM physician in most places in the country, urologists want an U/S prior to taking a patient to the OR.
Case 6: Myxedema coma. Critical actions: intubate, identify history of under-treated hypothyroidism, give thyroxine, warm patient, treat with antibiotics for infection.
Case 7: CO poisoning. Critical actions: 100% O2 and transfer to hyperbaric O2. CO half life: RA=4 hours, 100%O2=40 minutes, HBO=20 minutes.
Case 8: Ruptured ectopic. Critical actions: IV fluids/prbc’s, consult OB to take patient to OR, give rhogam for A- blood type. Methotrexate is not indicated to treat ectopics who have free fluid or hypotension or pain plus multiple other complications. Girzadas comment: EP’s should have nothing to do with giving or deciding to give methotrexate. Ectopic management with methotrexate is fraught with great medico-legal risk.
Chastain Ocular Ultrasound
Use hi frequency linear probe. Scan the closed eye through lid. Have pt do EOM while you scan.
Papilledema: you can measure optic nerve sheath diameter. Diameter > 5.7 in adults is abnormal. Measure 3 mm from the retina. Harwood comment: can you use this to identify idiopathic intracranial hypertension? Michelle, not sure if there is a report in the literature on this.
Retinal detachment: Retina is always attached at the optic nerve. If it isn’t then it is more likely to be a vitreous detachment. If macula is detached (mac-off) this is more likely to require surgery. Macula is just medial to the optic nerve.
Vitreous detachment: Looks like clothes in a dryer.
Vitreous hemorrhage: layered hyperechoic material in globe.
Negro 5 Slide Follow Up
Elderly man on Coumadin who fell at home. Pt did have a small stroke which likely caused fall. AAA identified on U/S. Ct showed no leak. He had endovascular repair of aneurysm in hospital.
Kmetuk 5 Slide Follow Up
Elderly female with vertigo and vomiting. Abnormal heel to shin exam and nystagmus. CT head negative. Neuro dx’d pt with vertebral-basilar stroke. CT is 26% sensitive for diagnosing cerebellar stroke. HINTS testing: head impulse test suggests stroke if pt keeps eyes on your nose, nystagmus, test of skew (check eye alignment after covering one eye).