Conference Notes 7-9-2013
Conference Notes 7-9-2013
There are 5 images in this document. If you don't see them, scroll to the bottom and click on "Read in Browser"
This Tuesday was an Ultrasound Workshop with 2 hours of didactics and 2.5 hours of hands-on workshop.
Lambert U/S Knobology
Center your image on the screen and adjust the depth of the image to maximize its size on the screen. Depth of image is key to making the important objects on the screen best visible.
Every Ultrasound probe can be toggled through 3 modes:
High frequency =high resolution mode
Low frequency=deeper penetration mode
Intermediate frequency= general mode
The toggle switch is at the inferior portion/right side of screen
Visualize your target organ or area in 2 planes to define the boundaries of the object. If you don’t define the outer boundaries, you can miss things like gallstones or IUP’s.
Lambert 7Up Scan Sonographic Approach to Investigating Shock/PEA
Why? EP’s correctly identify the cause of shock only 24% of the time. Healthcare providers often do not correctly identify a carotid pulse. U/S is accurate for determining intravascular volume.
How do you do it? RUQ> Subcostal>IVC>Aorta>pelvis>parasternal long axis of heart>Lung
Morrison’s pouch is second lowest area of supine abdomen. Suprapubic area of pelvis is lowest but it has a small volume and fluid there may escape detection. So Morrison’s pouch is called by sonographers the “Money Pouch”.
UCG positive female with fluid in Morrison’s pouch has nearly 100% specificity for ruptured ectopic pregnancy.
Subcostal view should include the liver and the heart.
Hypovolemia will cause the heart to have a small/collapsing RV and a hyperdynamic LV.
Poor overall contractility suggests cardiogenic shock. Large RV suggests PE. Specifically the RV will bow out toward the LV and be of similar size to LV or larger than the LV in a patient with shock from PE.

Hyperdynamic LV function in setting of shock is likely to indicate sepsis as the cause of shock.
Proximal IVC views are helpful for gauging volume status. Hypovolemia causes decrease in IVC diameter >50% with inspiration.
Landmarks for aorta views are spine/IVC/aorta. Aorta diameter >3cm =aneurysm. The larger the aneurysm the more likely it is to be ruptured. In a patient in shock without abdominal or back pain and a 3cm aorta. The AAA may not be the cause of shock. Smaller aneurysms are less likely to rupture.
On Parasternal long view, good contractility is identified by seeing the anterior mitral valve leaflet strike the ventricular septum.
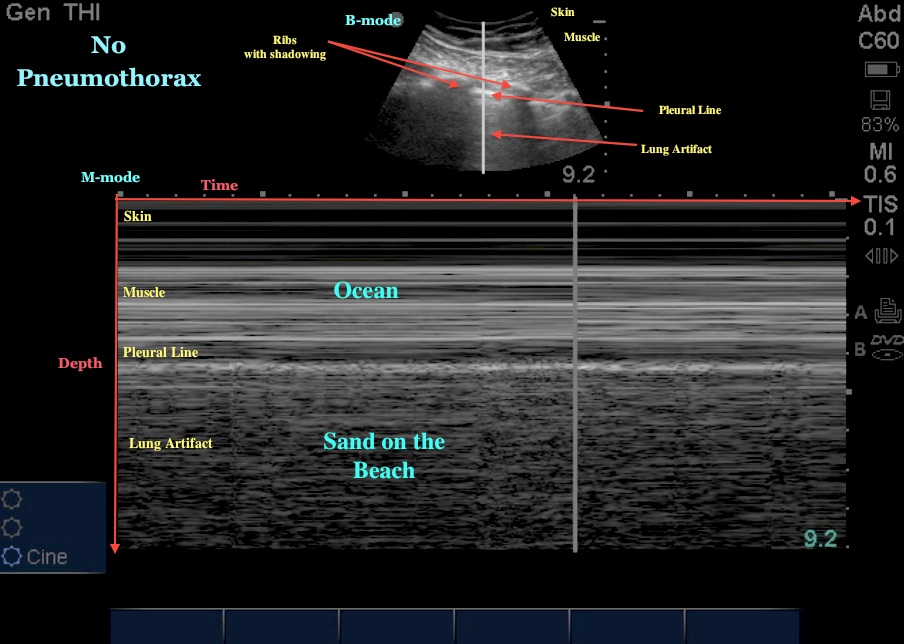
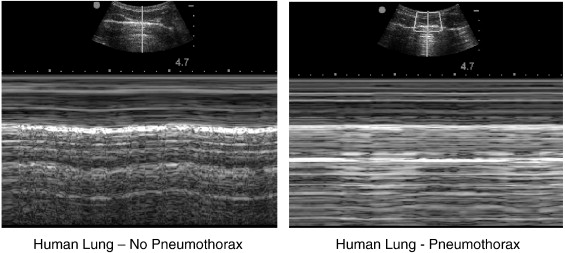
Lung views can help identify pneumothorax or chf. Pneumothorax shows no sliding of pleura and no moving comet tails. With M mode, normal lung has sky/beach appearance. With pneumo, M mode shows no beach.
Large comet tails “headlights in the fog” is a good sign of CHF. Girzadas comment: I find the “headlights in the fog “ sign very specific for CHF. Mike agreed with this.

Please consider donating to our EM Foundation to benefit resident education/development. Thanks for your consideration/generosity.
/em-foundation/