Gore/Konicki Oral Boards
Case 1. 30yo female with sore throat. Patient is 5 days post partum. No fever. On exam pt has an enlarged uvula. Diagnosis was idiopathic angioedema. Treatment is H1 blocker, H2 blocker, steroids. Consider EPI if necessary. Lovell/Motzny/Girzadas comments: This is uvular hydrops or Quinke’s disease. Treat with steroids, histamine blockers, racemic epi nebulizer treatment, cold fluids or ice/popsicles at home. Check for strep. Don’t overdo the work up. No need for CT or xrays in these patients.
Quincke's Disease/Edema
Case 2. 57yo male with marked jaundice and abdominal pain. Light colored stools/dark urine. No fever. Pt has history of ulcerative colitis and is on an azole drug. Diagnosis was cholestasis. Can be due to impaired processing or obstruction. Pt had primary sclerosing cholangitis. Primary sclerosing cholangitis is associated with inflammatory bowel disease. Image the liver and GB with U/S or CT. Consult GI. Main thing is to rule out acute cholangitis.
Case 3. 40 yo male with crush injury to right hand. Pt had open finger fracture. Critical actions: digital block for pain management. Opioid pain medication, Neuro-vascular exam. Tdap, prophylactic antibiotic, irrigate wound, splint, cover open wound. Elise comment: Be specific and clear what you want the consultant to do.
Febbo Pearls and Pitfalls in the Emergent management of HTN
Treat asymptomatic HTN cautiously or not at all. You want to avoid overshoot hypotension and possibly cause a stroke or MI.
Hypertensive Emergencies have end organ dysfunction.
Hypertensive urgencies and malignant hypertension are terms that have fallen out of favor. Papilledema was thought to be a marker of malignant hypertension but this has more recently been found to be unrelated to end organ dysfunction from HTN.
BP stabilizes in a patient at about an hour into an ED visit. This may be the optimal time to get a blood pressure reading.
End Organ Damage: Encephalopathy, pulmonary edema, acute kidney injury, preeclampsia, aortic dissection, acute coronary syndrome, ICH, CVA.
What testing is required: Screening tests (Labs, CXR, EKG, CT) don’t help. You should do targeted testing for specific symptoms or signs. Normal urine dip predicts a normal creatinine. ACEP Guidelines recommend against routine screening. In selected patients, Cr screening may be indicated.
There is no evidence to suggest any benefit of lowering BP acutely in the ED. There are many case reports that describe iatrogenic negative effects due to acute overtreatment of assymptomatic HTN.
Elise/E Kulstad comment: We have both seen patients who have developed stroke symptoms stemming from over-zealous BP lowering. Motzny comment: Most patients have some symptoms like headache or weakness. We have to decide on these patients whether to work them up. There was then a discussion among the attendings about who needs a CT head for headache. Most agreed that the higher the BP, the older the patient, and possibly the more concerning the headache symptoms the more likely they would be to do a head ct. This was a grey zone for everyone though.
Hypertensive Emergencies: Encephalopathy, pulmonary edema, aortic dissection, acute kidney injury, preeclampsia. Most patients with severe hypertension are volume depleted. Volume depletion can make patients very sensitive to BP treatment and make them more likely to become hypotensive. IV fluids can be used to treat a patient if they become hypotensive due to BP management. The one exception to this is pulmonary edema.
Go-to med to most hypertensive emergencies is Nicardipine. Start at 2.5mg/hr and titrate by 2.5 mg/hr Q 15 min.
Labetalol is second choice. Dosing is 20mg q10 minutes up to 300mg. Avoid this drug in patients with a history of asthma/bronchospasm/COPD
NTG has a niche use for acute pulmonary edema.
Esmolol is good for rate control but not indicated for BP control. Can be used as combined therapy with nicardipine to reduce wall stress in aortic dissection.
Fenoldopam: Peripheral dopamine agonist that maintains renal perfusion. Dosing is 0.1mg/kg/min to start. It is pretty expensive.
Agents to avoid: Hydralazine, clonidine, ace-inhibitors, nitroprusicsside.
Aortic dissection: Pain meds, esmolol, nicardipine
Preeclampsia: Magnesium +/- hydralazine or nicardipine. Hydralazine is falling out of favor.
Ischemic stroke: If thrombolytics are being given get bp less than 180/110. If no lytic being given, don’t treat BP if less than 220/120.
ICH: Nicardipine
Sympathomimetics (cocaine, crystal meth): Benzos
Pheochromocytoma: Use phentolamine
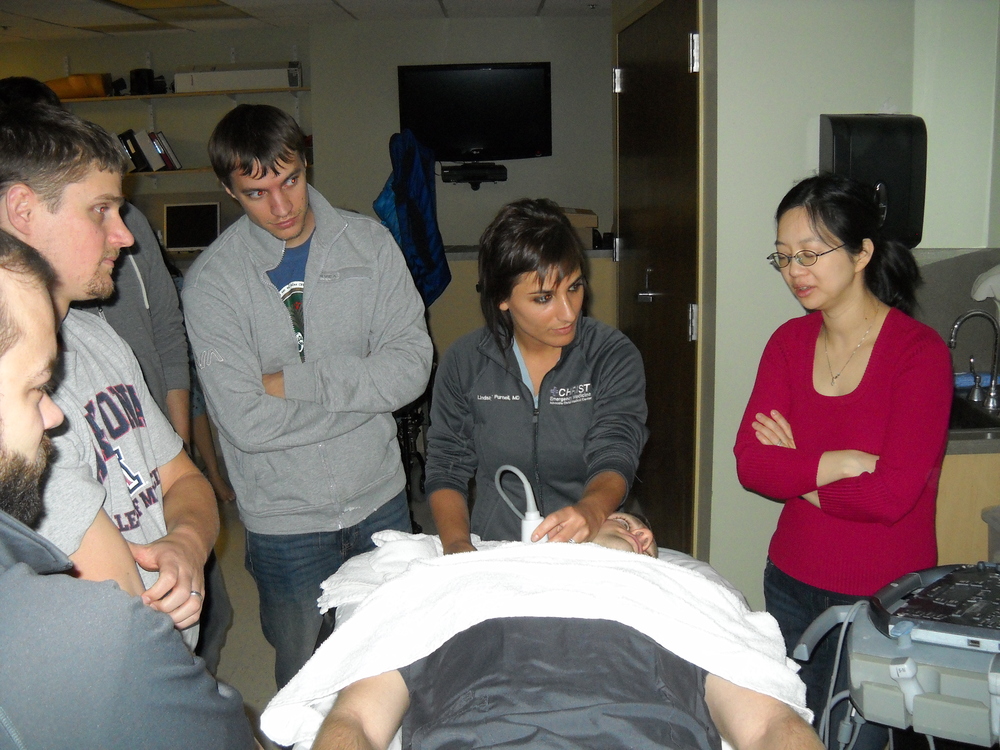
Lambert Vascular Access Workshop
High frequency linear probe is the optimal choice for vascualar access procedures. It gives higher resolution with less depth penetration. That performance profile is usually best for visualizing vessels. You want optimal resolution of the vessel usually at a shallow depth beneath skin.
IJ Placement: When the operator is working from the head of the bed to place a line, keep the indicator of the probe pointed to the operator’s left. Visualize the IJ in the transverse orientation and center it on the screen. Be sure the vessel is compressible to rule out a thrombus. Puncture skin at a 45 degree angle. Your puncture point should be the same distance from the probe as the depth of the vessel on the screen. A trick to this procedure is identifying where the tip of the needle is on U/S. As the needle tip tents the vessel wall, you have to jab the needle through the vessel wall.
Peripheral IV Placement: Look for a shallow, large vein in the medial aspect of the upper arm. The basilic vein is usually most superficial. Make sure it is thin walled and compressible and go for it. Elise comment: We are limited by the catheters we have. Mike response: Yes, you need a longer peripheral catheter to do this procedure. Usually need a 2cm length catheter or longer.
U/S for DVT: You just need to scan the proximal and distal segments of the femoral vein. Isolated mid-femoral clots are very rare. In the popliteal view, the popliteal vein is closest to the skin. (POP on TOP) In the femoral view, the vein is deep to the artery. The femoral/popliteal vein should be completely compressible. If not, it is either the artery or a DVT in the vein. Clot is not always echogenic, so a clot may be present if the vessel is not compressible but you don’t see echogenic material in the vessel. Also, you can see baker’s cysts in the popliteal fossa. The primary criterion for a DVT is non-compressibility of the vessel.

"Pop on Top"

The Proximal Femoral Vein tends to lie deep to the Artery in Contrast with the Popliteal Vein
Hands-On Vascular Access Workshop