Conference Notes 5-14-2014
Balogun/Collins Oral Boards
Case 1. 30yo male, s/p mvc with head injury. Transient LOC. Patient has headache On further history patient is found to have hemophilia. CT shows ICH. Critical Actions: Give Factor 8 prior to CT. You want to get to 100% activity by giving 50u/kg of Factor 8. Get stat CT head. Consult hematologist & neurosurgeon.
Case 2. 30yo female with 1 day of left shoulder and flank pain. Patient had syncopal episode yesterday and fell down some stairs. Patient is hypotensive. Pregnancy test is negative. FAST scan shows fluid in Morrison’s pouch. Patient had splenic rupture. Critical actions: Resuscitate with IV fluids and PRBC transfusion. Consult surgery. Admit to ICU. The spleen is the most common organ injured in blunt abdominal trauma.
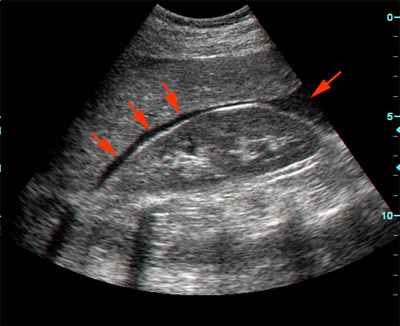
*Fluid in Morrison’s pouch (google image)
Case 3. 30yo male firefighter is SOB and confused after being pulled from building fire. Patient has burns on trunk and face, singed nasal hairs. Critical Actions: Intubate based on likely airway burns. Administer parkland formula IV LR. Patient had elevated CO level and needed hyperbaric therapy. Indications for hyperbaric therapy: syncope, altered mental status, seizure, pregnant with level >15%, blood level>25%, or myocardial ischemia.
*Parkland Formula (google image)
For pediatric patients less than 20kg, add maintenance fluids to the calculated Parkland fluid dose.
Christine comment: It is critical to give Factor 8 prior to sending hemophiliac patients with head injury to CT.
Girzadas comment: Consider inter-personal violence as an underlying cause of women and children presenting with trauma. Know the Parkland formula for adults and remember in kids less than 20kg you have to add maintenance fluids to the calculated Parkland Fluid volume.
Herrmann/Ketaneh STEMI Conference
Case 1. 67yo female presents with flank pain. She has a history of CABG. First EKG does not have STEMI criteria. Patient developed chest pain in ED. 2nd EKG shows LBBB with lateral ST depression. Silverman comment: Patient is tachycardic on second EKG and LBBB could be rate-related. I would slow her rate with a beta blocker and see if EKG improves. Labs show elevated Cr and potassium= 6.4. Troponin is 0.16. Interventional cardiology did not take patient to cath lab initially. They preferred to treat potassium and treat pain. 3rd EKG shows tachycardia and LBBB. Cardiologists in audience comment: They generally felt hyperkalemia is the issue and the risk of catheterization in the setting of hyperkalemia and elevated creatinine is dangerous. A STAT echo looking at the anterior wall motion would be helpful in determining if the LBBB was due to STEMI. 4th EKG shows resolution of LBBB with peaked anterior t waves and lateral ST depression. Patient still has chest pain. Code STEMI called by the ED physician and patient had a thrombectomy of saphenous vein graft and stenting of another vessel. Cardiologists in the audience did not feel that a Code STEMI should have been called. Cardiologist comment: To call a STEMI in the setting of a LBBB, the patient needs to have ischemic chest pain and have a clinical picture of ACS. Most would not have taken patient to cath lab with hyperkalemia and elevated creatinine.
Case 2. 69yo female presents in respiratory distress. She was initially treated for COPD exacerbation. Initial EKG shows non-specific changes and is made more difficult to interpret due to a lot of baseline artifact. Patient had respiratory acidosis on ABG. Patient was intubated. Repeat EKG shows tachycardia, lateral Q waves and ST elevation. Cardiologists in audience felt the 2nd EKG did not make sense with the clinical picture or in comparison to first EKG. They questioned whether lead placement was different. Q waves don’t usually develop in 2 hours. Cardiologists in the audience looked at the first EKG again and felt there was subtle ST elevation in V6. Takasubo’s Cardiomyopathy can present in this fashion.
Takotsubo cardiomyopathy, also known as transient apical ballooning syndrome,[1] is a type of non-ischaemic cardiomyopathy in which there is a sudden temporary weakening of the myocardium. Because this weakening can be triggered by emotional stress, such as the death of a loved one, a break-up, or constant anxiety, it is also known as broken heart syndrome.[3]Stress cardiomyopathy is a well-recognized cause of acute heart failure, lethal ventricular arrhythmias, and ventricular rupture
The typical presentation of takotsubo cardiomyopathy is a sudden onset of congestive heart failure associated with ECG changes mimicking a myocardial infarction of the anterior wall. During the course of evaluation of the patient, a bulging out of the left ventricular apex with a hypercontractile base of the left ventricle is often noted. It is the hallmark bulging out of the apex of the heart with preserved function of the base that earned the syndrome its name "tako tsubo", or octopus pot in Japan, where it was first described.[5]
Evaluation of individuals with takotsubo cardiomyopathy typically includes a coronary angiogram, which will not reveal any significant blockages that would cause the left ventricular dysfunction. Provided that the individual survives their initial presentation, the left ventricular function improves within 2 months. Takotsubo cardiomyopathy is more commonly seen in post-menopausal women.[6] Often there is a history of a recent severe emotional or physical stress. Wikipedia

Takotsubo cardiomyopathy (google image) Notice how the apex does not contract as well and in effect balloons out. Sorry for wandering off into takotsubo cardiomyopathy when it is really not relevant to this case.
3rd EKG in ICU shows Inferior/Lat ST elevation and subtle ST depression in 1 and AVL. Patient wen to cath from ICU and found to have a 90% occlusion of left main (not takotsubo’s). Balloon pump was placed. Patient developed multi-system organ failure and died. Cardiologist comment: Do bedside echo looking for wall motion abnormalities to help you figure out these cases. Sometimes if the patient is too sick to go to Cath Lab, you need to document your decision making to not go to the Cath lab. If you need a rapid read on a STAT echo during daytime hours call 41-5555 to notify the Cardiologist of the urgency of the case.
Teaching Points: ST elevation in AVR is concerning for ischemia. If you identify ST elevation in AVR with associated diffuse ST depression in 6 or more leads this identifies left main occlusion and is considered to be a STEMI criteria by the AHA. ST elevation in AVR is also seen in LAD occlusion, triple vessel disease, and sub endocardial ischemia.
Prominent T wave in V1, V1>V6 suggests early ischemia as well.
Gore Trauma Lecture
Kasia gave multiple pointers for pre-resuscitation preparation when you are on the Trauma service and awaiting the arrival of a patient via EMS. Talk with the ED nurses prior to arrival of the patient to get an idea of how severely injured the patient is. Think ABC’s: Prepare the resuscitation room for intubation. If you have any info from prehospital personnel that the patient may need a chest tube or thoracotomy, etc., prepare for those as well. For circulation support prepare for venous or bone access. First choice line is 2 large bore IV’s. Second choice line is Cordis placement. Whatever IV access you obtain, shorter/large bore catheters are preferred over longer/smaller bore catheters. The shorter and larger diameter catheters allow for much higher flow rates based on poiseuille’s law.

*Poiseuille’s Law (google image) Note that Radius (r4) decreases resistance to flow to the 4th power and length increases resistance to flow.
Omi comment: I prefer not to use IO lines because I have seen osteomyelitis following IO line placement and large volume infusions thru IO lines is painful. We manage mostly young adult trauma patients in whom IV access is usually not a problem.
If you have concerns about moving the C-Spine during intubation, one option is to leave the patient in the collar and use the glidescope to intubate while the patient is immobilized in the collar.
Discussion about standard “go-to” RSI drugs for the trauma patient: etomidate and succinylcholine or rocuronium where the first choices. Dr. Omi did not feel the risk/time/benefit ratio favored using fentanyl, lidocaine in addition to the basic two drug RSI regimine nor did it favor a sedated look (ketamine/topical anesthetic). Omi was strongly against propofol due to risk of hypotension. Shayla comment: There is virtue in keeping your RSI plan simple. Many ED’s don’t have multiple drug options available and they are not used to giving drugs other than for example, succinylcholine for neuromuscular blockade.
Chest Tube Placement: Kasia showed a video of chest tube placement. One thing I learned from Dr. Omi is that when she anesthesizes the chest wall prior to procedure, she actually enters the pleural space with the needle. She will advance the needle until she aspirates air or blood. Then she withdraws the needle until she no longer is getting air or blood and then injects local anesthetic to numb up the pleura. She states the pleura is the most painful structure when placing the tube.
Shayla comment: Be diligent to look for the second GSW. Patients frequently don’t realize they have been shot more than once. They are focused on the most painful or visible injury.
Case 1. 36 yo patient in MVC. Patient was tachycardic and tachypneic with flail chest with paradoxical movements of left chest wall and subQ crepitence.
Kelly comment: If you are in a community ED with limited staff, just intubate this patient and throw in a chest tube right away.
Patient was intubated and left chest tube was placed. A right side chest tube was also placed based on hypotension and chest wall crepitence. FAST exam was negative. Left chest tube drained 1500ml of blood. (Indications for thoracotomy is 1200ml initially or 200ml/hr for 3-5 hours) CXR showed wide mediastinum. Patient was taken to OR for thoracotomy. Transexamic acid was given in the ED.
Patient eventually died due to multiple severe injuries and coagulopathy.
Shayla Garrett and Ellen Omi comment: If you are working in a rural ED, intubate the patient, place a chest tube, start blood, and helicopter the patient to a Level 1 Trauma Center.
Garrett-Hauser Ethics
POLST Form Physician Order for Life Sustaining Treatment. Intended for persons for whom death within the next year is not unexpected. This form augments but does not replace the power of attorney form.
Case 1. 14 yo female with abdominal pain and vaginal d/c. Patient doesn’t want the ED doc to speak with her parents. Patient refuses treatment for PID. Can she refuse? The key issue is capacity for decision making. If the patient has decisional capacity you could make the case to let the patient decide. Girzadas comment: I would definitely speak with the parent. This case has a high risk of bouncing back with a bad outcome if you don’t discuss with parents and/or treat patient. In retrospect, everyone will question your assessment of capacity. This patient is not an emancipated minor and her ability to understand the long term consequences of her decision is questionable.
Case 2. Jail inmate refused blood transfusion. Patient however had critically low HGB and was judged by ED physician to not have decisional capacity because of the severe anemia. Patient was given PRBC’s against his will. The group veered into a discussion on physicians’ roles in judicial executions and forced feeding of inmates. The AMA states that physicians cannot ethically take part in executions or forced feedings.
Case 3. Police had a court order for a doctor to perform a body cavity search for drugs on a patient brought to the ED. Patient had no medical emergency identified related to drug overdose. Shayla’s advice was to not perform a body cavity search against the patient’s will if there is no medical emergency. A local Indiana hospital is being sued for forcibly obtaining a urine sample to get a drug screen and drawing blood for etoh level for police use despite no medical emergency being present. In Illinois, if police ask you about test results for a patient who is under arrest you can give that info to police.
Case 4. Patient with ruptured ectopic. Patient refuses to consent for surgery. She says this is God’s will that this will kill me. Patient would only consent to blood transfusions. The emergency physician activated psychiatry, risk management, administration to help solve the problem. Psychiatry saw patient and felt she did not have decisional capacity. So surgery was done.
Case 5. Patient is on a liver transplant list. Patient presents to ED following a fall with head injury. Blood alcohol level is 250. Should the emergency physician notify the transplant center that the patient’s alcohol level is 250? In most centers this info will knock a patient off the transplant list. There was a split in the group about what to do. The majority of the group would report the patient to the transplant center. The breakdown was basically along concerns of justice vs. physician responsibility toward the patient. The physician told the patient they were going to consult with the transplant center about their managment. After being contacted, the transplant center asked for the patient to be transferred to them so they could manage and advise the patient.
Jamieson 5 Slide Follow Up
60yo female with altered mental status. Patient found wandering thru neighborhood by a neighbor. Patient had anion gap acidosis. INR was 3.2. ABG showed respiratory alkalosis and metabolic acidosis. ASA level was 106.2.
ASA toxicity clinical picture: tinnitus, vertigo, altered mental status, nausea/vomiting, hyperpyrexia, pulmonary edema, coma. Mixed acid-base disorder with respiratory alkalosis and anion-gap metabolic acidosis.
Treat with charcoal if it can be administered safely and bicarb drip to alkalinize urine. Indications for dialysis: coma, altered mental status, cerebral edema, pulmonary edema, renal insufficiency, clinical deterioration, or serum level >100. Avoid intubation if possible. Mechanical ventilation frequently can’t match human minute ventilation.
Meyers 5 Slide Follow Up
42 yo male with altered mental status and icteric sclera/jaundice. Labs showed markedly abnormal LFT’s. Lactate was 5.9. Prolonged INR. Utox was positive for opiates. Vitamin K was given.
Patient admitted to ICU. Labs showed both Hep B and C.

*Hepatitis Serology (google image)
70% of patients with Heptitis B have a benign anicteric course. 0.5% of patients will have fulminant liver failure. This patient fell into this latter group.
Entecavir is a nucleoside analog that treats acute hepatitis B with severe features (INR>1.5 or bili>10, immunocompromised, elderly, pre-liver transplant)
