Conference Notes 7-23-2014
Permar/Lovell Oral Boards
Case 1. 55yo male with SOB for 2 days. BP 100/60. Labs show leukocytosis. CXR shows normal heart size and bilateral infiltrates. Diagnosis is acute pulmonary syndrome due to Hanta Virus. Critical Actions: Recognize septic shock, aggressive IV fluids, Intubation, Broad-spectrum Antibiotics, norepinephrine, ICU admission.
Optimal care would include ID consult and notification of the Public Health Department. Elise comment: First thing is to recognize and rapidly correct vital signs. Management for Hanta Virus Pulmonary syndrome is supportive care. Clinically looks like rapidly progressive non-cardiogenic pulmonary edema. There is no specific treatment for hanta virus.
Harwood and Carlson comments: The diagnosis for this case could have been plague or other uncommon infections. You have to have a broad ddx. Would have been nice to give IV doxycycline or gentamycin in addition to usual CAP coverage to cover plague.

*Rapid Progression of Hanta Virus Pulmonary Syndrome
Case 2. 19 yo male very agitated. 160/110, HR=110. Pt has gun fall out of his pocket. Crystal meth also falls out of his pocket . Urine Tox is positive for amphetamines. Critical Actions: Scene safety/search patient, check blood sugar, check temperature, sedate with benzobiazepines, monitor for normalization of vital signs, assess for psychiatric stability. Optimal care: consider excited delirium (hyperthermic/super-human strength/risk of sudden cardiac death), consider checking CPK, offer rehab information. Methamphetamine acts on dopamine receptors more than serotonin receptors. Scary thing is that methamphetamine actually re-wires your brain and causes permanent neurologic changes.
Andrea & Elise comments: Control violent behavior in this type of patient with high-dose benzos, ketamine or ketafol.
Case 3. 20 yo male with left hand pain due to a snake bite. BP=100/55, HR=115. Patient has spreading edema of hand. Critical actions: CroFab administration 6 vials, IV opioid pain control, IV fluids, ICU admit. Optimal care: monitor for compartment syndrome. If compartment syndrome develops, treatment is administration of more CroFab rather than fasciotomy. First aid is no suction of venom, no incision, no tourniquets. For prolonged transport you can use a constricting band to hinder lymphatic spread of venom. If possible keep the injured extremity at heart level and minimize patient’s activity until they get to the hospital.
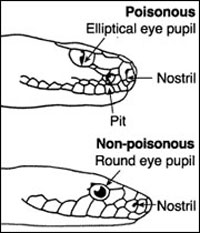 *Pit vipers have a heat sensing pit, elliptical eye, and fangs
*Pit vipers have a heat sensing pit, elliptical eye, and fangs
Harwood comment: For the boards, don’t give Haldol to a patient with a drug overdose. Ice is not recommended for snake bites.
Andrea comment: You can’t go wrong with benzos for the agitated patient.
Mosier (Loyola Burn Center)/Management of Patients with Thermal Injury

*Criteria for transfer to Burn Center
Harwood question: What %age of patients transferred to your burn center can be treated as an outpatient. Answer: >50% are discharged in 1-3 days.
Rule of 9’s is an easy way to estimate burn size in adults.

*Rule of 9’s
Patient’s palm + fingers is @1% of burn size. When calculating BSA affected, do not include areas of first degree burn.
Larger burns cause capillary leak resulting in slow/progressive fluid loss. Fluid replacement goal should be 30ml of urine output per hour.
Parkland formula is indicated for patients with greater than 20% BSA burned: Parkland formula=4ml/kg/%BSA burned. Half the volume is given in the first 8 hours and the second half given in the next 16 hours. Some patients will need more or less fluid than estimated by this formula but it is a reasonable starting point. Clinicians will have to adjust fluid administration to reach goal of 30ml of urine output per hour.
Dr. Mosier showed some horrific pictures of extensive burns. He discussed his thinking on the use of escharotomies to relieve constricting pressure on torso or extremities. Elise question: What is the timing on doing an escharotomy? Answer: most patients can have up to a 6 hour delay to getting an escharotomy. So in most cases it can be done at a burn center. Girzadas question: How do you know if you have cut deeply enough to perform an effective escharotomy? Answer: When you cut deeply enough, the burned skin will spread apart and the tenseness of the tissue will be feel much less.
Carbon monoxide poisioning is the most common cause of death due to inhalation injury. The Upper airway has a great ability to absorb/diffuse heat. Edema due to upper airway burn injury peaks at 12-24 hours.
Singed facial and nasal hair does not=intubation. If a patient is burned from a flash burn lighting a grill or smoking while on oxygen they usually won’t need intubation. Patients with inhalation burns due to closed space fires (caught in a house fire for example) are at much higher risk for airway edema and intubation.
If patient is phonating without stridor they usually won’t need intubation
Dr. Mosier showed some pictures of severe electrical burns. These burns can require larger fluid volumes than suggested by the Parkland formula. These patients may need surgical debridement, fasciotomy and/or amputation.
There are 127 Burn Centers in the US. Only 66 Burn Centers are “Verified or Accredited”. Loyola and U of C are the only 2 Burn Centers in IL that are Verified. There are 3400 Deaths/year in the US from burns. The majority of deaths occur due to residential fires. The total average body surface area burned has decreased over the last 2 decades. Survival rates for all burns is 97% overall. There are better outcomes at Burn Centers.
Don’t forget that you should transfer cases of TEN to a burn center.

*Toxic Epidermal Necrolysis
Kelly comment: Please comment on how to refer a patient to your Burn Clinic. Answer: You can call the Burn Center to arrange a clinic appointment. We are a 5 day/week clinic. We are not open on weekends.
Elise question: What is the preferred dressing for minor burns. Answer: Wash the wound with soap and water. Debride blisters that are on body areas of frequent movement. If the blister is intact on a non-high frequency moving surface you can leave it intact. We still like topical silvadene or other antibiotic ointments on the burns. Silvadene is better for deeper burns. Mepilex sponge is a new silver-eluting dressing that works well. You can actually use silvadene on the face. If it gets in the eyes or mouth it can cause irritation. It is a false axiom that silvadene can’t be used on the face.
When transferring a patient to a burn center just cover the burn with dry sterile sheet or dressing. Don’t use moist or wet dressings, no packing in ice. Just use a dry dressing.
Salzman Tactical Medicine
Dr. Slazman discussed the tactical/EMS response in Sweden to the mass attack/murder of children on an island summer camp. He discussed the difficult decisions of whether to treat a severely wounded patient vs. getting control of scene safety at the outset prior to caring for wounded patients.
Tactical medicine Mnemonic: Call A CAB n’ Go
Call for help. Abolish all threats. Circulation-Airway-Breathing. Neuro Check. Go=transport patient to hospital.
Tourniquets are still useful for halting exsanguination from limb GSW’s.
Average adult has about 5-6 liters of blood. With significant blood loss, the color of the lips (palor) is a sensitive indicator of severe anemia.
Harwood question: How do you function as a physician wearing SWAT-type protective gloves. Answer: It is an issue. We do have black medical gloves that we can put on after we take off our SWAT protective gloves.

*AVPU simple and quick neurologic assessment
ED thoracotomy has the highest success rate for single isolated stab wounds to the chest. If you can relieve the pericardial tamponade and close the heart wound, you can save the patient’s life.
When caring for patients who have suffered a blast injury, be aware of embedded shrapnel in the patient. These foreign bodies can injury you. Wear personal protective equipment and be cautious.
Amputated limbs/body parts are rarely able to be re-attached successfully.
Unfortunately due to meetings, I missed the other excellent lectures this day.