Conference 2-4-2015
Airway Day
Patel Approach to the Difficult Airway
“Prior Planning Prevents Piss Poor Performance”
Have a plan for your intubations before you start giving drugs. Specifically have an initial approach laid out and 1-2 back up/rescue plans if that initial approach fails.
4 Dimensions of a difficult airway
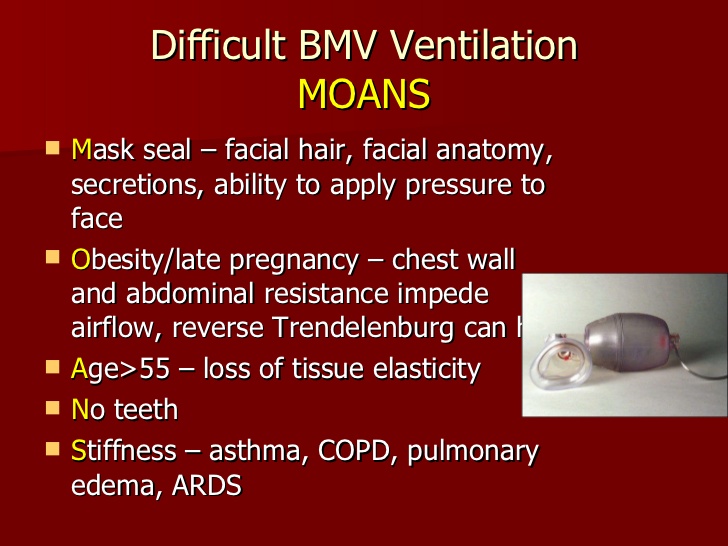
1. Difficult BVM
*MOANS
Pregnant women in the third trimester commonly have an edematous airway
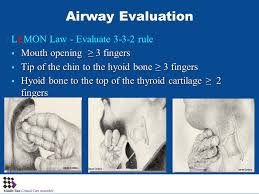
2. Difficult Laryngoscopy
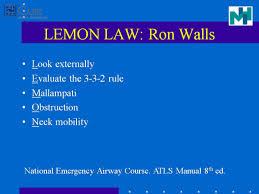
*LEMON
*332 Rule=3 fingers in an open mouth, 3 fingers from the hyoid to the chin,
2 fingers from thyroid notch to hyoid. If the patient does not fit these measurements, expect a difficult airway.

*Mallampati score
If the patient has a mallampati score of 1 you can pretty much feel comfortable that you will get a decent view of the cords. Any other mallampati score is a crap shoot. With mallampati 2-4 scores you can get anywhere from a class 1-4 view of the cords.
Asian patients tend to have difficult airway
3. Difficult Cricothyrotomy can be assessed by visual inspection of the neck
Prior to intubation it is critical to pre-oxygenate the patient to saturate the hemoglobin, create an oxygen reservoir in the lungs and de-nitrogenate the lungs.
To optimize pre-oxygenation, use a tight fitting mask and open the oxygen wall device to as high as it will go. Wide open O2 provides a higher O2 concentration than 15 liters/min. In addition, keep a nasal cannula on the patient using a second oxygen wall device set at 15liter/min during the entire intubation procedure to provide passive oxygenation during intubation. You can also use very high flow oxygenation cannulas to provide even more passive oxygenation.
Pre-oxygenation should be done with the patient sitting up. It improves the effectiveness of preoxygenation due to less ded space and less weight on the thorax.
Cricoid pressure (Sellick maneuver) tends to displace the airway laterally. It can compress the airway and distort the laryngeal view of the intubating physician. There is controversy whether this maneuver is helpful/indicated and it has tended to fall out of favor.
BURP/External Laryngeal Manipulation maneuver may improve the laryngeal view. The intubating physician moves the larynx into optimal view and the assistant holds the larynx in that position while the intubating physician places the tube.
*ELM External Laryngeal Manipulation
Line up the external auditory meatus and sternal notch in all patients prior to attempting intubation. This positioning was initially recommended for obese patients but probably is useful for all patients.
*External auditory meatus to sternal notch position
Use Ketamine to perform DSI (delayed sedation intubation). This is sedation with preservation of respiratory drive to optimize oxygenation during intubation. After ketamine, give 2-3 minutes of Bipap prior to attempting intubation.
Lovell Airway Devices
In a high stakes, stressful airway scenario you have the best opportunity for success using a device that feels familiar to you. That’s why video laryngoscopy devices are our usual go-to rescue devices. They have a very similar mechanical use and feel to direct laryngoscopy.
Supraglottic devices like an LMA can serve as great rescue devices because they are fast and can be done blindly. They are not definitive airways because they do not provide a tube through the cords. However, they can serve as a bridge device until you are able to pass a tube through the cords.
This is what you need in your armamentarium to manage airways: Bougie, LMA, direct laryngoscope, video laryngoscope, fiberoptic/COMS scope, and surgical airway technique. You need to have access to and be facile with one device from each of these categories to be fully prepared to handle all potential difficult airways.
There is some controversy about teaching direct laryngoscopy to residents when we have video laryngoscopy available. We (ACMC EM) still think direct laryngoscopy is important for current residents in training. There can be instances when the video laryngoscopic device either is not available or is working sub-optimally due to fogging or blood/secretions in the airway.
For cardiac arrest, 2010 ACLS guidelines advise initially placing an LMA in the airway so as to not interrupt chest compression. Proceed to intubation after you obtain ROSC if the patient remains unconscious.
Be sure to use airway devices (bougie, video laryngoscopy, fiberoptic/COMS) on easy airways when working in the ED so that you are comfortable using all these advanced devices when you need them for a difficult airway.
When doing a cricothyrotomy the biggest error is waiting too long to start making the cut. When you have a difficult airway, start prepping the neck as the intubating physician is working is attempting to visualize the airway Be ready to start cutting as soon as the intubating physician identifies that intubation is not possible.
Age cutoff for cricothyrotomy is 8 years. Below that age, you will need to do a trans-tracheal jet ventilation.
Elise walked us through the commonly used advanced airway devices and discussed their use in specific cases.
Airway Workshop
The Airway Hands-On Work Shop was fantastic! Thanks to Drs. Bolton, Putman, and Tekwani for organizing this year’s event. Thanks also to the over 20 faculty members who taught the workshop. Thanks to all our faculty members who covered the ED during the Work Shop!