If you don't see images scroll to bottom and click open in browser.
Carlson Cardiovascular Drug Toxicity
Calcium Channel Blockers
CCB’s impair calcium influx resulting in vasodilation, bradycardia, negative inotropy, and decreased insulin production.
CCB’s break down into 2 groups based on their mechanism of action:
Verapamil/Diltiazem block conduction.
Nifedipine/Amlodipine dilate smooth muscle causing low BP.
However, in large overdoses this distinction is lost.
Calcium channel blockers are highly protein bound and are not dialyzable.
Patients suffering from CCB toxicity present with hyperglycemia. Hyperglycemia correlates with severity of overdose. Hyperglycemia correlates with the need for pressors, need for pacing, and for death.
Early decontamination is a key management issue. Andrea said that if you get a patient with a massive ingestion within the first hour, go ahead and perform gastric lavage. This is the one overdose that she would recommend gastric lavage. Patients can die from CCB toxicity and if you get a chance to intervene to decontaminate the gut early before the patient is symptomatic, it could be life-saving. You should only perform gastric lavage if the patient is not bradycardica and not already hypotensive.
Activated charcoal is also indicated and likely beneficial.
Next step is to battle the toxin. Andrea cautioned us that with CCB poisoning, sometimes you can do everything right to fight the toxin and the patient still dies.
Use a multi-modal approach to counter CCB toxicity. It is considered the most effective option. Below are listed the indicated therapies. You should use as many as you need to stabilize the patient.
Calcium: Its effect is short lived. It improves BP more than heart rate. 1 ampule of Calcium Chloride or 3 ampules of Calcium chloride as a single dose. Give 1 dose every 20 minutes. These are relatively large doses of calcium. After 3 or 4 doses check an ionized calcium level with an ABG.
Atropine is the initial therapy for bradycardia.
Pressors: Andrea’s first choice would be norepinephrine. Epinepherine would be next. Vasopressin may be a reasonable adjunct due to it’s effect of increasing intracellular calcium. There are a couple of case reports touting the combination of vasopressin and norepinephrine. Andrea felt this combination was a reasonable option. Harwood comment: Vasopressin is not a stand alone option for a pressor. You also need to use norepi or epi in addition to vasopressin. Andrea agreed.
Glucagon can be tried at 5mg over 30 seconds. If the initial dose is not effective, try 10mg over a couple of minutes. If either dose results in improvement, start a glucagon drip. If no effect, move on to other modalities.
Pacing is indicated for symptomatic bradycardia or conduction block.
Amrinone is another reasonable modality
High dose Insulin/Glucose has an inotropic effect by delivering metabolic fuel to a carbohydrate-dependent myocyte. High dose insulin should be the initial therapy for calcium channel blocker overdoses. Give 1 unit/kg of insulin as a bolus then start a drip at 0.5 unit/kg/hr. You can titrate up on the drip. Supplement glucose and potassium as needed.
Intralipid is also a recommended therapy
ECMO may be an effective advanced therapy. Contact your intensivist early to start the ball rolling for a severely unstable patient who is not improving with the above multi-modal approach..
Disposition: For sustained release CCB ingestions and amlopdipine ingestions admit the patient for 24 hours. For all other immediate release CCB ingestions, patients can be observed for 6 hours and if asymptomatic can be medically cleared.
Jamieson Eye Trauma
Case 1. 30yo male was transferred to ACMC with a left orbital floor fracture and elevated IOP. On arrival at ACMC, Patient had large subconjunctival hemorrhage. No hyphema. EOMI. Visual acuity was normal. CT showed small hemorrhage in retro-orbital region and an orbital floor fracture. Tonopen measurement of eye pressure at ACMC was normal. Trauma service thought that that probably the eye pressure was measured in the area of the subconjunctival hemorrhage and the outside hospital get a falsely elevated pressure. You have to take the tonopen measurement on the cornea not the sclera/conjunctiva.
Retrobulbar hematoma if large can develop into an ocular compartment syndrome. Treatment for ocular compartment syndrome with decrease in visual acuity is emergent lateral canthotomy.
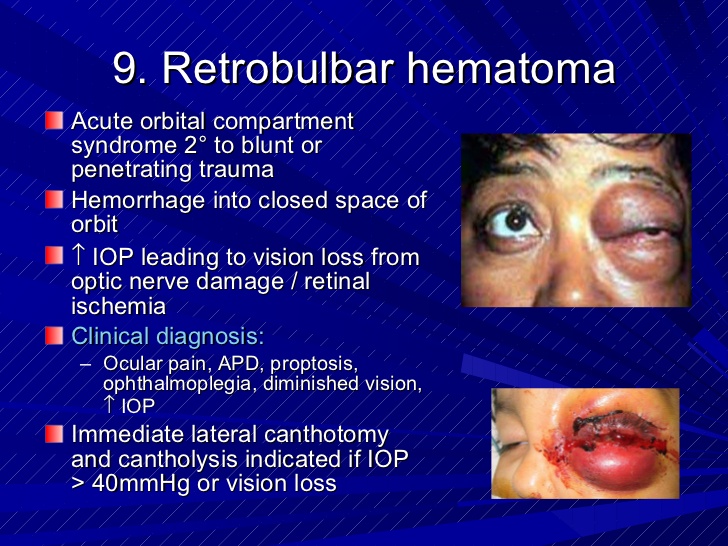
*Occular Compartment Syndrome
Case2. 21 yo female presents with facial injuries due to air bag deployment. Patient had left periorbital hematoma and a hyphema. Visual acuity was impaired in the left eye.
Hyphema is associated with other eye injuries including ruptured globe.
Treatment of hyphema includes daily pressure monitoring, limited physical activity, head elevation, steroid drops and beta blocker drops. Get ophthalmology consult while patient is in the ED.
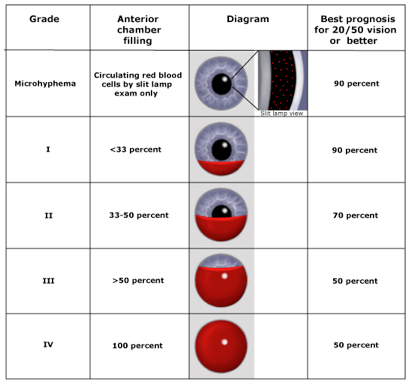
*Hyphema
*Hyphema Grading System
Case 3. 34 yo male brought in by EMS with GSW to right face. Patient can’t open right eye and has no vision with right eye. CT shows bullet had obliterated the orbit.
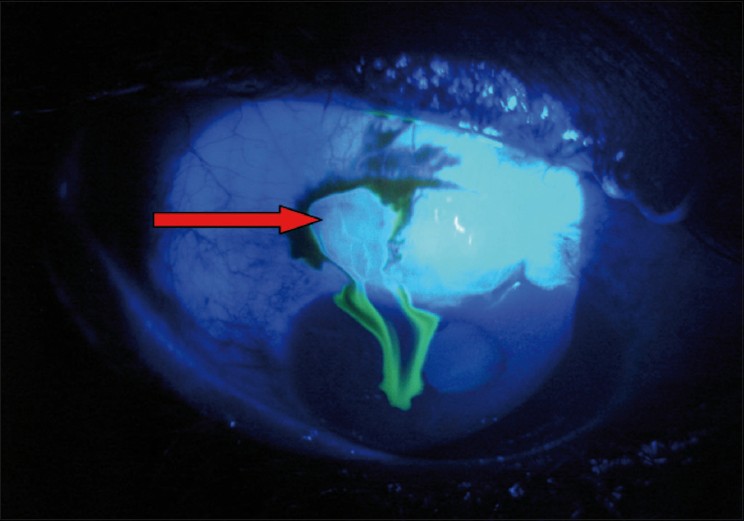
All the following can indicate a ruptured globe: decreased vision, teardrop/deformed pupil, hyphema, subconjunctival hemorrhage, intraocular contents protruding from eye, and positive seidel’s test.
*Positive Seidel’s Test
*Ruptured Globe
If you suspect ruptured globe, give vancomycin and ceftazidine, shield the eye and call ophthalmology for surgical management.
This patient had an unsalvageable eye. His injured eye was enucleated to avoid sympathetic ophtalmia. This can occur days to years after trauma. It is uncommon, but is thought to be an autoimmune mechanism that causes intraocular inflammation of the uninjured eye.
Harwood comment: Hyphemas tend to settle into the lower portion of the anterior chamber due to gravity. You need to limit the patient’s activity and elevate their head to allow the blood to remain in the inferior portion of the anterior chamber. This will keep as much of the anterior chamber clear as possible.
Lambert comment: Topical steroids are used to decrease the incidence of adhesions within the anterior chamber.
Lambert Occular U/S
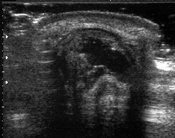
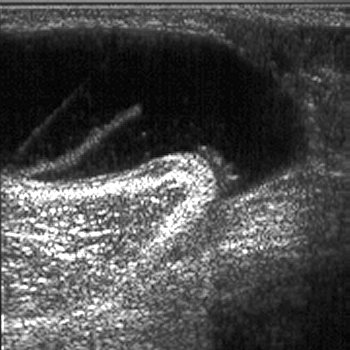
To perform ultrasound of the eye, have the patient close the affected eye. Place a lot of gel on the eyelids of the affected eye. Use the linear probe on the closed, gelled eye.

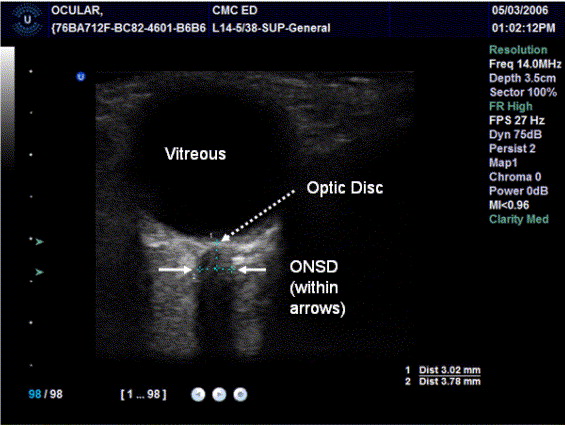
*U/S image of eye
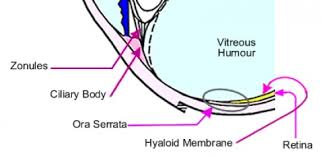
The retina is attached in the area of the optic nerve and ora serrata.
*Ora serrata

*Retinal Detachment
Retinal detachments can be either with the macula still on or with the macula off. Tell the ophthalmologist that the macula is on. Some ophthalmologists feel that if the macula is off, the detachment is no longer an emergency. So if you want the ophthalmologist to deal more urgently with the situation, say “macula on”
Vitreous detachment can look like retinal detachment but the vitreous is not tethered at the optic nerve or ora serrata. So the detachment may include these two areas. Differentiating this from a retinal detachment by ultrasound may be beyond the pay grade of an ER doc.
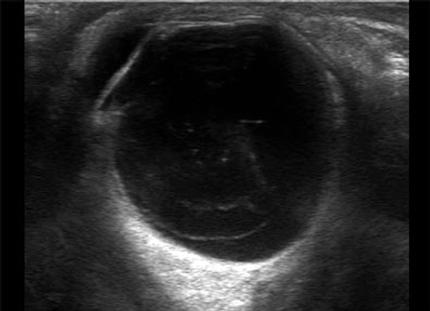
*Vitreous Detachment

*Vitreous Hemorrhage
*Globe Rupture
*Elevated Intracranial Pressure Measurement by Measuring the Optic Nerve. You measure 3 mm from the retina. If the nerve is more than 5mm, it corresponds to an ICP >20.
Lambert Soft Tissue Ultrasound
*Cellulitis

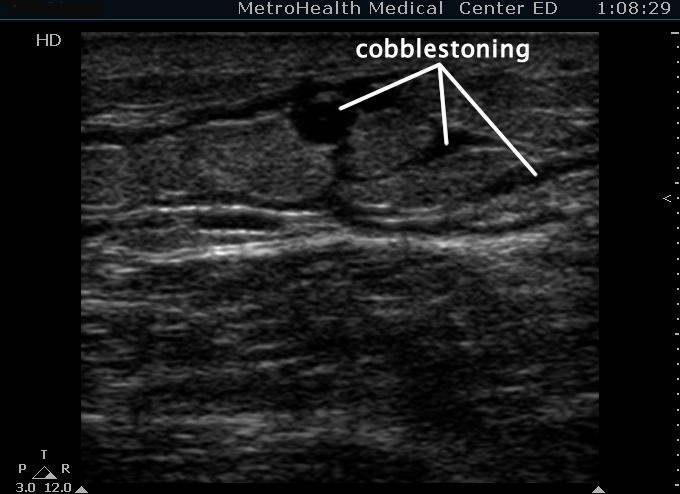
*Abscess with some surrounding cobblestoning
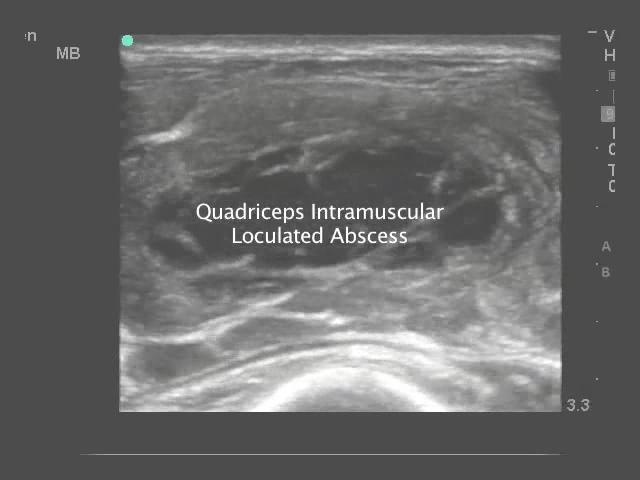
*Pyomyositis is basically an abscess in the muscle. These should go to the OR for drainage.
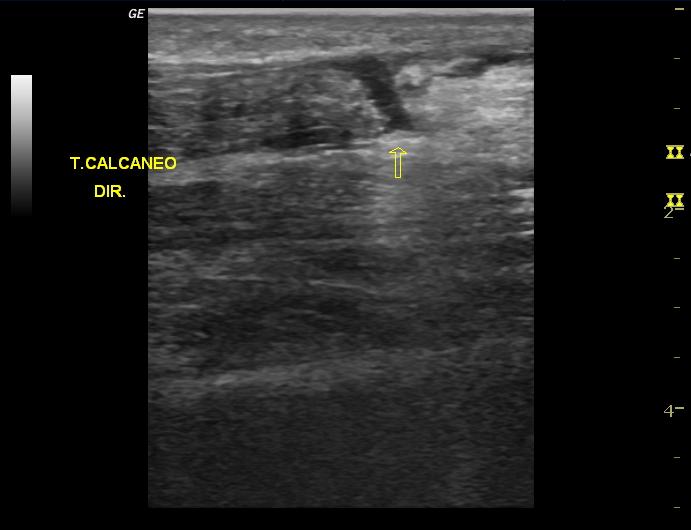
* Achilles Tendon Rupture
*Baker’s Cyst (note the comma shape)

*Supraspinatuous Tendon Rupture (90% of rotator cuff tears are due to supraspinatous tear)

*Enlarged Lymph node, not hypo-echoic outer ring and hyper-echoic center. Well circumscribed outer edge.
Ultrasound Workshop