Alumni Feedback from Conference Notes 2 weeks back:
Hey Dan, It's Valerie Merl again. Just want to give some input on peritonsilar abscess treatment in the community. Your note says - peritonsilar abscess : consult ENT to drain. This was the thought when I was in residency also. We don't have ENT at my hospital so I would transfer all of these patients to a hospital that has ENT. Until I found out that the ER doctors at that hospital were draining all of these abscesses and sending these patients home. ENT was only involved as a follow up. So I learned to drain peritonsilar abscesses. In many places this is a skill that is expected of an emergency medicine doctor.
See, someone reads the emails you send out!
Thanks Valerie, really appreciate the feedback! I welcome people’s insights on any of the topics covered in the conference notes. If you send an email, I will put you in the conference notes as well.
Bonder/Ryan Oral Boards
Case 1. 50 yo female presents with chronic back pain and acute dyspnea. CXR is normal. ABG shows respiratory alkalosis and metabolic acidosis. Salicylate level is elevated. Follow up history identifies that patient had been over-treating with ASA for her back pain. Diagnosis is salicylate toxicity. Critical actions: Bicarb drip (3 amps of bicarb in a liter of D5 and run at 250ml/hr), IV fluids, trend ASA levels, and consult nephrology for possible dialysis. Patients can get cerebral hypoglycemia from salicylate toxicity so keep serum glucose over 80. Acetazolamide is contraindicated in salicylate toxicity. Acetazolamide does alkalinize the urine but it also lowers arterial ph which promotes salicylate movement in to the brain.
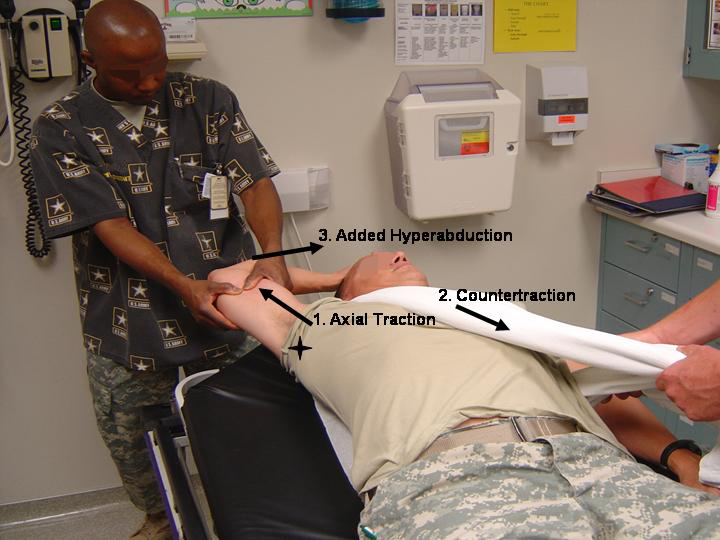
Case 2. 55yo male presents with right shoulder pain. BP 170/90 P 115 R 20 T 37 P/O 99%. Patient fell from tree and his arm is abducted at the shoulder with the elbow pointed to the ceiling and the patient cannot move his shoulder. Diagnosis is luxatio erecta. Critical actions: Pain control, shoulder reduction. Luxatio erecta has a high incidence of axillary nerve and artery injury. However, there is not a recommendation that all these patients require a CT angiogram or ultrasound of the axillary artery after reduction. It is acceptable to just palpate for good pulses proximally and distally in the injured extremity following reduction. If you have higher suspicion based on mechanism or exam then go on to imaging the artery.
*Luxatio Erecta
*Luxatio Erecta
*Luxatio Erecta Reduction
Case 3. 25yo female found by EMS personnel seizing in a park. BP 165/100 P 130 T 37.3Blood sugar=100. Narcan had no effect per EMS. No known PMH. Patient has another seizure in the ED. IV Ativan stops the seizure. Patient appears to be homeless. Thorough physical exam reveals a gravid abdomen. Diagnosis is ecclampsia. Critical actions: IV magnesium, BP control, monitor the fetus, fetal ultrasound, possible delivery of fetus.
*Treatment for pre-ecclampsia/ecclampsia
Harwood comments: Fentanyl dosing is microgram/kg. For an adult male with a shoulder dislocation he probably needs 75micrograms to 100 micrograms for a single dose. For ecclampsia, in addition to giving magnesium, you also need to treat the blood pressure.
Elise comments: If you have a toxicology case on the boards, consult poison control. To optimize alkalinization when treating salicylate toxicity, check the urine ph not the blood ph. Physiologically, the goal is to alkalinize the urine to increase urinary excretion of salicylate.
Berkelhammer Ischemic Disease of the Gut
Congestive Hepatitis is when the liver gets swollen due to acute CHF. This can also cause central zonal necrosis of the liver lobules. AST can be specifically more elevated than ALT in the setting of shock liver/acute CHF liver
You can get hepatitis due to hypoxia and severe anemia as well. Pregnant patients can get catastrophic antiphospholipid syndrome that results in liver infarctions. This syndrome can be difficult to differentiate from HELLP syndrome.
Chronic mesenteric ischemia is called abdominal angina. Patients will get pain shortly after eating. Patients may loose weight due to not eating to avoid pain. Smokers, diabetics and hypertensive persons are at higher risk for abdominal vascular disease. Patients need to have double or triple vessel disease to get abdominal angina. If you do a screening ultrasound or CT angio and the celiac and superior/inferior mesenteric arteries are patent, the patient does not have abdominal angina. Treatment for abdominal angina is angioplasty or endarterectomy.
Acute mesenteric ischemia has pain out of proportion to exam. Labs can be initially normal but as time passes, the WBC will go up, metabolic acidosis will develop, amylase and lipase will increase, and lactate will elevate. If you see air in the portal circulation or in the bowel wall, that is a sign of dead gut.
*Air in the bowel wall (pneumatosis intestinalis)
Think about mesenteric ischemia in patients presenting with abdominal pain in the setting of atrial fibrillation.
Aortic dissection can also cause mesenteric ischemia. The dissection can occlude the celiac and superior/inferior mesenteric arteries.
Arterial mesenteric ischemia tends to give abrupt onset of pain. Venous mesenteric ischemia can be insidious in onset. Predisposing factors for venous thrombosis include portal hypertension, hypercoaguable states, and cancer.
Low cardiac output states can result in non-occlusive mesenteric ischemia. The gut arteries can vasospasm in the setting of hypotension/low cardiac output.
ED Treatment of acute mesenteric ischemia is heparin and vascular surgery consultation.
Ischemic colitis can present as a patient who wakes up in the middle of the night with acute onset abdominal pain and initially multiple brown bowel movements followed by diarrhea followed by bloody diarrhea. Patients will have tenderness over the colon. WBC can be elevated. It can occur in any area of the colon. The vessels perfusing the colon on the side opposite the omentum are prone to vasoconstriction and or occlusion. Young people on vasoconstrictive medicines like sudafed can actually get ischemic colitis.
Ischemic colitis compared to small bowel mesenteric ischemia has less pain, gradual onset, colonic tenderness, bloody diarrhea, less sick. Whereas small bowel mesenteric ischemia has sudden onset severe pain, no focal tenderness initially, no bloody diarrhea until late in the course.
Celiac compression syndrome (median arcuate ligament syndrome) The arcuate ligament can compress the celiac artery in thin patients. They will have pain c/w chronic abdominal angina.
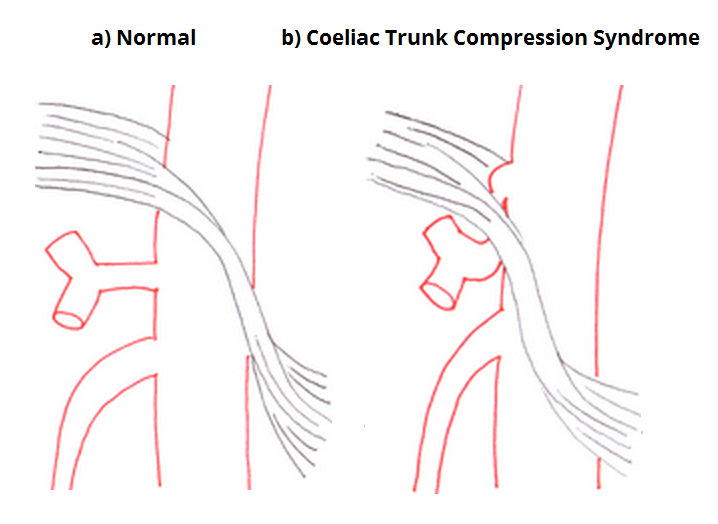
*Celiac Compression Syndrome
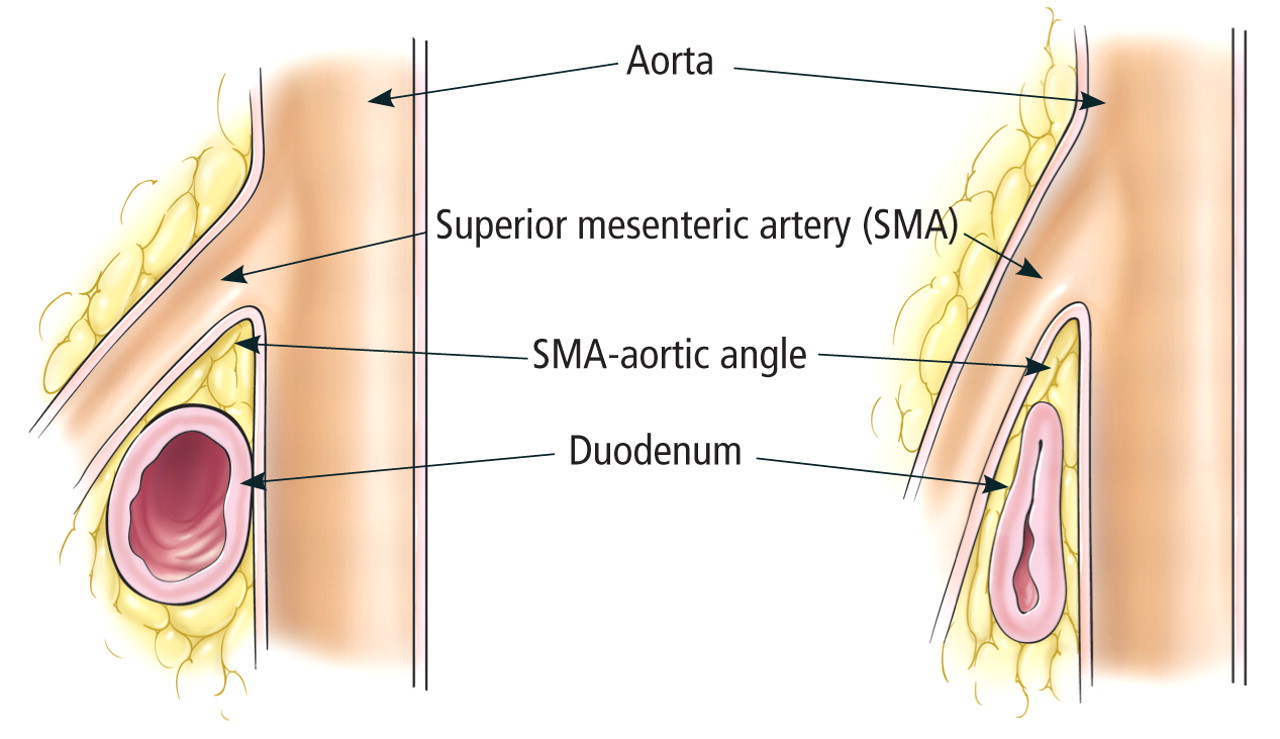
SMA syndrome occurs in patients who have lost a large amount of weight (like 100 lbs). The loss of omental fat squeezes the duodenum between the SMA and aorta. The patient has basically a gastric outlet obstruction from this compression and they will vomit after eating.
*SMA syndrome
Remke Management of Traumatic Arrest
Case 1. 25 yo male with multiple GSW’s to abdomen and chest. Patient lost vitals in the field.
What to set up prior to patient arrival: Airway equipement including a back up device. Have pneumothorax decompression needles and chest tube kits available. Have a central line and IO kits ready. Have a thoracotomy tray in the room as well. Then get other physician and nurse help assembled.
When the patient arrives: Get an airway, needle decompress or place chest tubes bilaterally, make sure you have adequate vascular access. Use bedside echo to identify pericardial fluid, cardiac activity, and intra-abdominal fluid. Consider ED thoracotomy. ED thoracotomy is probably only for penetrating trauma. You only do ED thoracotomy for blunt trauma if you personally witness loss of vital signs. Dr. Omi comment: I don’t do ED thoracotomy for blunt trauma even if the patient looses vital signs in the ED. Cardio-pulmonary arrest in blunt trauma patients is usually due to head trauma or aortic injury or massive intra-abdominal bleeding. You can’t fix those problems with an ED thoracotomy.
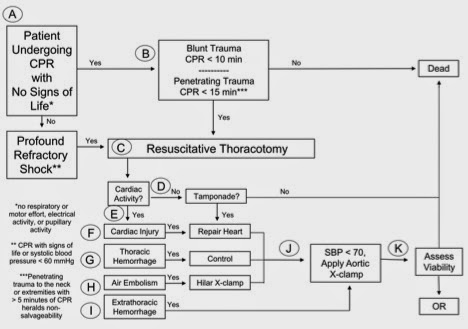
*Thoracotomy Indications
Don’t do ED thoracotomy in a patient with multi-system blunt injuries, severe head trauma, or unwitnessed loss of vital signs.
Down sides to ED thoracotomy is risk of blood exposure to staff, neurologically decimated survivors, uses up your time and staff resources in a busy ED.
When you make your cut for an ED thoracotomy, make the cut at the nipple line in men and at the infra-mammary fold in women. Dr. Lee comment: There are 4 things you can accomplish with an ED thoracotomy, release of a pericardial tamponade, repair a cardiac injury/control bleeding, provide internal cardiac massage, and cross clamp the aorta.
If you get ROSC get the patient blood and get them to the OR. If you don’t get ROSC, carefully find and dispose of all sharps, suture up the procedural wounds before the family sees the patient, and change out of any bloody scrubs before you talk with the patient’s family.
Paik LVAD’s
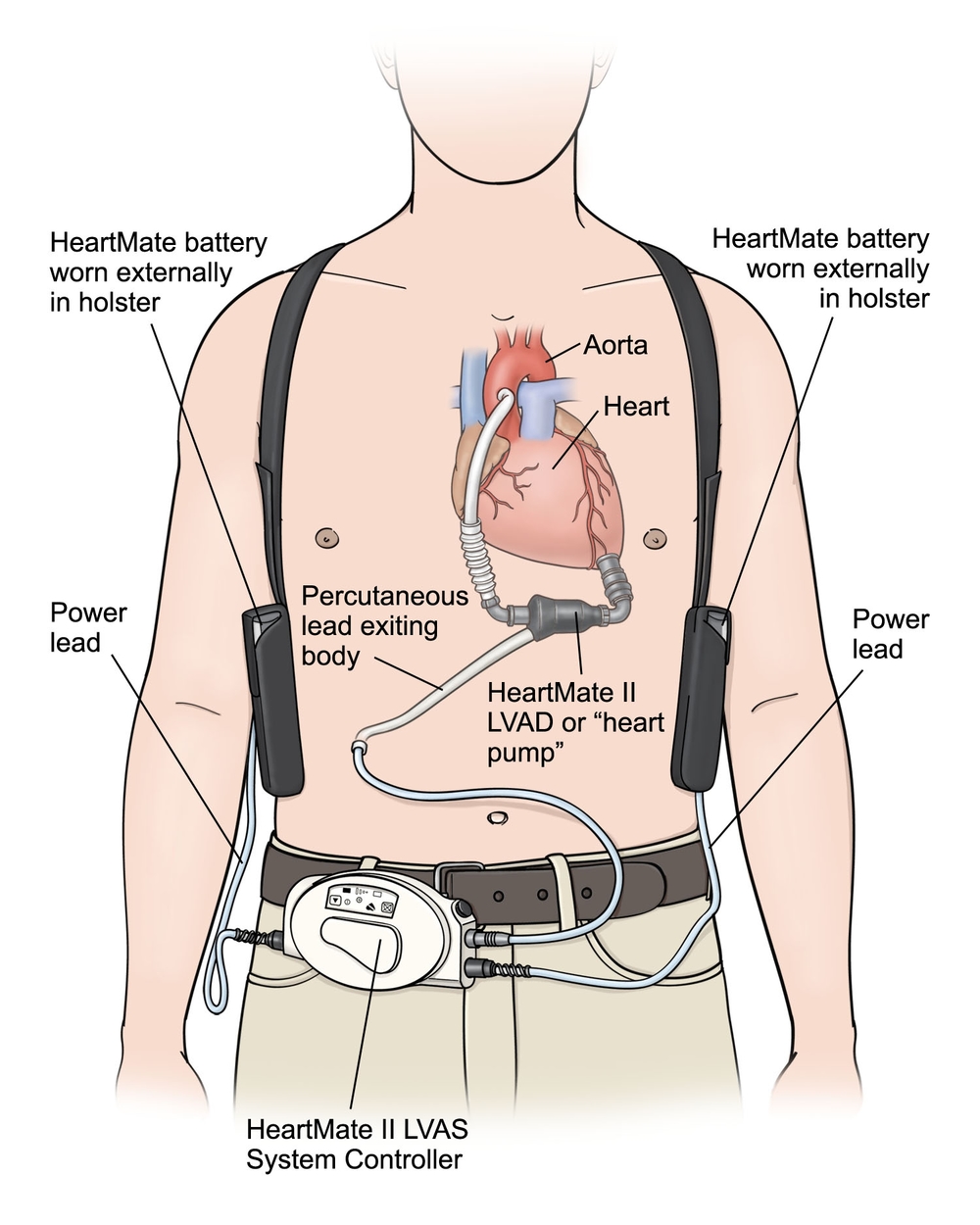
*LVAD Device
Alarms
Low Battery indicates need to replace battery.
Low Flow Alarm: Use your stethoscope to listen to the chest for the humming sound of the LVAD. If you hear the humming sound that means the pump is working. If the BP is low, try a small fluid bolus of 250ml. If the pump device in the abdomen is warm (place your hand on the upper abdomen to feel if it is warm) or the RPM’s are >15000 then a clot within the LVAD may be present.
Driveline Disconnection: This can cause syncope or death. Reconnect the driveline ASAP! If the patient is unresponsive start CPR while you trouble shoot the driveline.
Neuro complications: increased risk of intracranial hemorrhage, increased risk of emboli, chronic anticoagulation risks, and risk of ICH due to acquired von Willebrand Disease. Acquired vWB disease is due to platelet damage from the pump.
Cardiovascular complications: Arrhythmias (Amiodarone is first line treatment for ventricular arrhythmias). Suction events (pulls intraventricular septum toward the inflow cannula due to low volume. Treat with IV fluids)
GI complications: GI bleeds are common due to anticoagulation and vWB disease.
Infectious complications: All portions of the device and the subcutaneous pocket for the device can get infected. Biofilm producing organisms such as staph, candida, pseudomonas and enterococcus are the most common etiologies.
There was a discussion of LVAD patients presenting in V-Fib. If the patient is alert and mentating, start amiodarone and contact cardiology/LVAD coordinator. You may need to defibrillate the patient but if they are alert and mentating discuss with cardiology prior defibrillation.
If the patient is unresponsive and in V-fib, check if the pump is working by listening for humming with your stethoscope and check a blood pressure. If the pump is not working or the patient has a seriously low or absent BP, start CPR and defibrillate the patient immediately. While CPR is in progress you should trouble shoot the pump. Check first that the driveline is connected. If the pump is working and the BP is low give a 250 ml fluid bolus. It goes without saying, but get Cardiology/LVAD coordinator help right away.
Micheal Cirone comment: In unresponsive patients not in V-fib in whom the LVAD is working, consider other reversible causes of altered mental status like opioid use and hypoglycemia, before you start CPR.