Conference Notes 4-8-2015
If you don't see images, scroll to bottom and click on "open in browser"
Gore Orthopedic Fracture/Dislocation Description

*Bennett (2 syllables, 2 fragments)
*

*Mallet finger
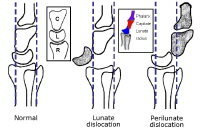
*Lunate/Perilunate dislocations
*Montaggia Fx/Dlx
*Galeazzi Fx/Dlx
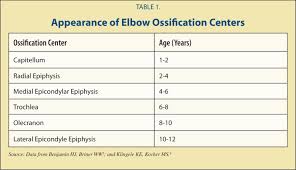
*Pediatric Elbow Ossification Centers
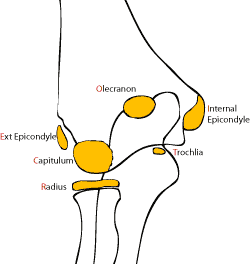
*Pediatric Ossification Centers
*Abnormal Pediatric Elbow Fat Pads
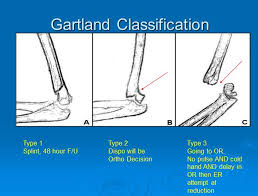
*Gartland Classification of Supracondylar fractures
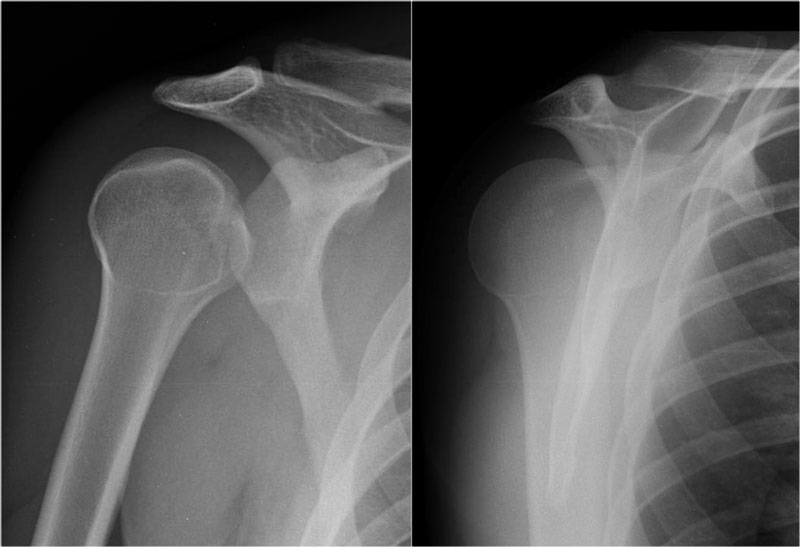
*Posterior shoulder dislocation
Lovell PE or not PE Step-wise Approach to Diagnosis
Step 1. Assess the patient’s pretest probability using gestalt, Wells score, or Geneva score. This is a critical step that gets overlooked frequently.

*Wells Score 4 is the score that dichotomizes likely vs. unlikely. Less than 4 is low risk. 4-6 is moderate risk. Over 6 is high risk.
Step 2. Is the pretest probability high, moderate, or low? If high, go directly to CT or VQ. If moderate order a d-dimer. If it is low then use PERC rule. If no risk then stop the work up right here.
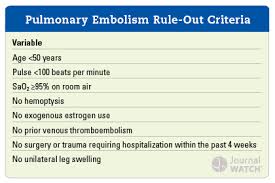
*PERC rule. The PERC rule research excluded cancer patients, and hypercoaguable patients.
Step 3. If PERC is positive do a d-dimer. If PERC is negative stop the work up right here.
Step 4. If d-dimer is positive do a CT or VQ. If d-dimer is negative you can stop. D-dimer sensitivity may be adversely affected in patients on anti-coagulation and those who have had symptoms for more than 14 days.
D-dimer interpretation can use age adjusted cutoffs= age X10 if the patient is over 50 yo.
D-dimer is reliable in pregnancy if a patient has a low pre-test probability and PERC is positive.
Pregnancy does not by itself make a positive Wells score or PERC rule. You can use both tools in pregnant patients.
Erik Kulstad comments: d-dimer has a better negative likelihood ratio than CT PE. You can make the case that you can use d-dimer in high risk patients as well. However this is not universally accepted. Elise felt high risk patients should get a CT or VQ scan.
Harwood comment: Do a d-dimer in all the pregnant patients whom you are considering doing a CT. The dimer is good enough to rule out PE and you will save a good number of pregnant patients radiation exposure.
Later generation CT scanning has the lowest radiation exposure for pregnant patients and is equal to VQ or perfusion only scanning.
Don’t do CT PE in patients with severe contrast allergy, renal insufficiency, multiple myeloma, or paraproteinemia.
Harwood comments: Beta blockers can blunt tachycardia and obscure the diagnosis of PE. Travel is an independent risk factor for PE. Testosterone and estrogen are also risk factors for dvt/pe. VQ scan is not equivalent to the CT scan for diagnosing PE. With VQ you frequently get results that are indeterminate.
Remke Protocol for Ordering VQ studies on off-hours/weekends/holidays
High probability patient by Wells score goes right to VQ without a d-dimer. You need to discuss the case with the radiologist.
Low or moderate probability patients get a d-dimer and venous dopplers of the lower extremities. If lower extremity dopplers are negative and dimer is positive then page the VQ technician to order the test. You don’t need to discuss the case with the radiologist. If there is enough isotope at the hospital, the technician will do the scan at that time. If there is no isotope left for that day, the VQ will be done first thing the next morning.
Elise comment: You only have to discuss the case with a radiologist if you do not order a d-dimer. If you have a positive d-dimer and negative ultrasounds you don’t need to contact the radiologist. You can just contact the nuclear medicine technician.
Parker ED Handoffs to Observation Service
Case1. 75 yo female with weakness and somnolence. Multiple co-morbidities. Work up in ED found a UTI. Patient received IV antibiotics in the ED. Plan was to put patient in observation rather than full admission. Patient’s family arrived later in ED course and informed ED team that patient had been hypercapnic previously. An ABG was ordered by the ED team just prior to signout. If the ABG showed hypercapnea, the patient would be a full admit. If the ABG was normal, the patient could go to observation. The ABG showed hypercapnea. However, the patient still was sent to the observation unit. The patient spent multiple days in the hospital and was not a suitable candidate for observation. Multiple issues at this transition of care were considered during this lecture.
Protocoled handoff processes decrease errors. A standardized handoff tool has been shown to be useful in decreasing missed information.
Following up on patients you have received in handoff is critical to avoid errors.
Patients inappropriately placed in the OBS Unit can take up a bed for days. That OBS bed then is not available for another patient who is appropriate for observation.
Meyers Trauma Lecture Cricothyrotomy
Patient with multiple blunt trauma was flown in by the helicopter. Patient had a cricothyrotomy placed in the helicopter. In the ED, the Trauma team had concerns about the stability of cricothyrotomy. Their initial approach was to attempt was to place an endotracheal tube. They took a look with the glidescope. There was very poor visualization due to blood and edema.
A lot of faculty comments: You could have placed a bougie through the tracheostomy tube and then achanged out the tracheostomy tube for an ET tube over the bougie through the cricothyrotmy incision.
The Trauma team was able to place a bougie through the cords under direct laryngoscopy. This was verified using a fiberoptic ambuscope through the cricothyrotomy.
*Ambuscope
Faculty comments: You could use the ambu scope through the cricothrotomy incision to verify the cric is in the appropriate position. Then Brian Febbo suggested that because the ambuscope is disposable, you can cut the handle off the fiberoptic cable and use the fiberoptic portion as a tube exchanger. Everyone thought this was a great idea.
Case 2. 70yo male with GSW to neck. King airway tube was placed in the pre- hospital phase. The tube became dislodged in the ED. Intubation attempts were unsuccessful. A decision was made to perform a cricothyrotomy.
The only contraindication to cricothyrotomy is age. Don’t do a cricothyrotomy in kids under age 8.

*Cricothyrotomy
Harwood comment: In a person who does not have neck trauma the Melker technique is totally reasonable.
Girzadas comment: If you do a surgical cricothyrotomy, it should be considered a blind technique. You have to be able to feel the cricothyroid membrane and puncture it and put a bougie through it without visualizing it.
There was some faculty discussion about whether surgical cricothyrotomy or seldinger cricothyrotomy had an advantage.
Girzadas reference regarding the issue of surgical vs. Seldinger cricothyrotomy
It is unclear whether they are speaking of only needle crics or seldinger crics as well. I think after doing a mini lit search on this topic, it is unclear if one techneique is superior over the other.
British Journal of Anesthesia 2011
Needle cricothyroidotomy had an unex-
pectedly high failure rate. It has been widely discussed as
to whether needle or Seldinger or surgical approaches to
direct tracheal access are best and it may be argued that
this project provides evidence that needle cricothyroidot-
omy has a high failure rate and therefore should be aban-
doned, particularly as surgical approaches were generally
successful (even when following failed needle cricothyroi-
dotomy). There are several reasons to be cautious about
such a conclusion. The NAP4 project specifically studied
events with poor outcomes and although we did seek
reports of all airway complications requiring emergency
surgical airway, it is possible that a dispr
oportionate number of successful rescue needle cricothyroidotomies
were not reported. Even if this explanation is not correct,
it is not reasonable to abandon the needle cricothyroidot-
omy technique without a much more robust explanation
of failures, which may have been due to failures of training,
use of inappropriate equipment, design problems with
appropriate equipment, or technical failures during use.
Examples of each of these observed in NAP4 include cepha-
lad placement of the device, use of an i.v. cannula for cri-
cothyroidotomy, mechanical failures of a Ravussin
cannula, and successful passage of a fine bore needle fol-
lowed by unsuccessful (and inappropriate) attempts to ven-
tilate with a low-pressure gas source.
Emergency surgical airway is the ‘final common pathway’
for all difficult airway algorithms. While much emphasis is
placed on the choice of device and technique, there is rela-
tively little written about the decision-making process and
timing of emergency surgical airway. An anaesthetic litiga-
tion review found that 42% of 179 difficult airway cases ter-
minated in CICV.
4
Errors of technique were frequent causes
of failure, particularly failure to ventilate with a high-pressure
source when a narrow cricothyroid cannula was inserted.
36
Of equal importance, persistent attempts at intubation
occurred before rescue techniques and the authors noted
that ‘our data suggest the rescue ability of (supraglottic
airways) may have been reduced by the effects of multiple
preceding attempts at conventional intubation’ and that ‘in
2/3 of the claims where CICV occurred a surgical airway
was obtained but was too late to avoid poor outcomes’. In
NAP4, there were also cases, in anaesthesia and also in the
ICU and ED, where persistent attempts at intubation
perhaps precipitated CICV, likely led to failure of rescue tech-
niques and definitely delayed emergency surgical airway.
Navarette/Bolton Oral Boards
Case1. Infant brought in by mom with increased fussiness. Infant had some signs of trauma on torso. History reveals child was with his father over the weekend. Diagnosis was non-accidental trauma with intracranial hemorrhage . Critical actions were: identify non-accidental trauma, perform a complete exam to identify ecchymoses, obtain a CT head and skeletal survey, attempt a fundoscopic exam, consult neurosurgery and admit to the PICU. You also need to notify DCFS. It is important to explain to the parent your concerns about abuse and that you are going to notify DCFS.
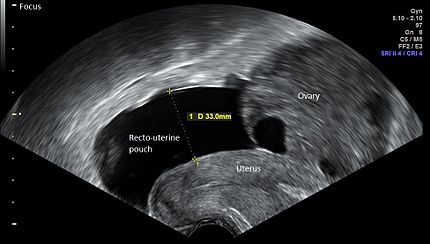
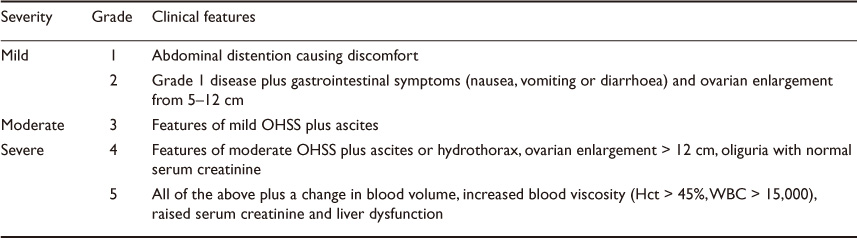
Case 2. 36 yo female with abdominal distension and SOB. HR 110, BP 98/52, RR 25. On history it was learned that patient was receiving fertility treatment. UCG is negative. Pelvic ultrasound shows ascites and bilateral enlarged ovaries with cysts. Chest X-ray show a pleural effusion. Diagnosis was ovarian hyper stimulation syndrome. Critical actions were: Consult OB, admit to hospital, administer O2. IV fluids can also be useful. Patients may need pain control. Patients with pleural effusions should be admitted. There is a risk of torsion due to enlarged cysts. You must be careful when performing an abdominal and pelvic exam to be gentle so as not to rupture the enlarged ovaries.
*Ovarian hyperstimulation syndrome
*Ovarian hyperstimulation syndrome
Williamson comment: These hyperstimulation syndrome patients always are closely followed by their fertility doctors and you should call them as soon as you suspect the diagnosis. They will help you immensely.
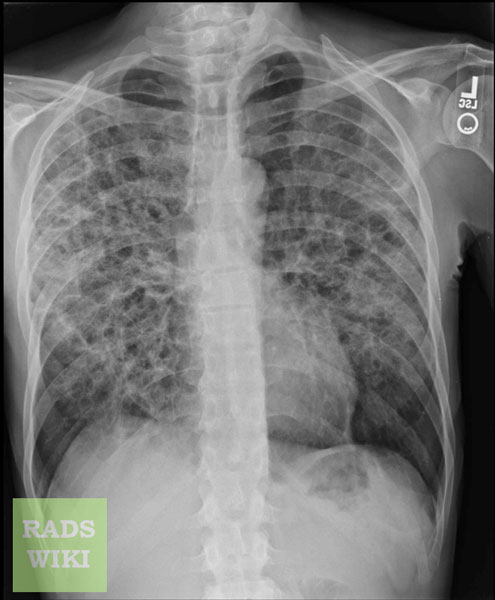
Case 3. 21 yo male with shortness of breath and cough. HR 105 BP 112/56 RR 35. Patient had been treated with a Z-pack but had not improved. History reveals weight loss and night sweats. Chest X-ray shows bilateral diffuse infiltrates. Rapid HIV testing is positive. Diagnosis was PJP pneuonia. Critical actions were: Obtain O2 sat, get history of HIV risk factors, Obtain CXR, give appropriate antibiotics. LDH can be helpful making the diagnosis.
*PJP pneumonia
Elise comment: There is an old adage: If you see a kid on oral boards they were abused. If you see a woman on oral boards they are pregnant. You have to make sure other children in the home are not at risk of abuse as well.
Harwood comment: When taking oral boards tell the examiner what you know. Think out loud. It helps when you don’t know the exact diagnosis. When you do know the diagnosis say it out loud. Explain your thinking.
Hart 5 Slide Follow Up
29yo female, pregnant. Sent in from opthomology clinic for retinal hemorrhages. Patient had headache and blurred vision. No chest pain or shortness of breath. Patient had history of prior pre-ecclampsia. Initial BP was 227/153. Labs showed leukocytes and anemia with no schistocytes.
Patient received labetalol without improvement of BP. Nicardipine drip was started. High Risk OB was consulted and IV magnesium was started. Protein/Creatinine ratio was 8105. Protein/Creatinine ratio >0.3 is diagnostic of pre-ecclampsia. Diagnosis was pre-ecclampsia with HELLP syndrome.
Edema is no longer included in the diagnosis of pre-ecclampsia. It is only hypertension and proteinuria. Protein/Creatinine ratio is a confirmatory test.
Ethics consult recommended c-section of pre-viable fetus to save mom’s life.
Management goal is lowering MAP 20% in the first hour and 25% by 24 hours.
No hypertensive medication has been shown to improve morbidity and mortality from hypertensive emergency.