Logan M&M
No case details, just the take home points.
If you have to intubate a patient who has pulmonary hypertension or RV failure consider using push dose pressors to optimize BP prior to intubation and do an awake intubation with ketamine instead of RSI.
If a trauma patient says, “ Don’t let me die!” that usually portends badness. Be aggressive in managing these patients.
Be disciplined when doing your secondary survey. Even examine the patient’s mouth. You have to be very careful not to miss other injuries.
Always have a back-up plan when intubating a patient. Have all the tools you need to perform both your primary plan and your back up plan ready to go at the bedside.
Remember that narcan can cause your patient to vomit.
NALOXONE (NARCAN)
Naloxone is a pure opioid antagonist that works by competitively inhibiting narcotics at the opioid receptor. Intravenous administration reverses the respiratory depressive effects of opioids within 1 to 2 minutes. Its clinical duration of effect is approximately 20 to 30 minutes. Long-acting narcotics may cause resedation. The opioids and their metabolites are active longer than the reversal agent. Carefully monitor a patient receiving naloxone for resedation and respiratory depression. The drug can be delivered via multiple routes (i.e., endotracheally, intramuscularly, intravenously, subcutaneously, and sublingually). The administration of 1 to 2 mg intravenously in adults and 0.1 mg/kg in children will reverse most respiratory arrest situations. Administer additional doses every 2 to 3 minutes to a total of 10 mg. Actively seek another etiology of the sedation and respiratory depression, other than narcotics, if the respiratory depression is not reversed after 10 mg of naloxone. Use caution as naloxone can result in opioid withdrawal in those with physical dependence or intoxicated with narcotics.
Small aliquots of 40 µg titrated to effect may be delivered in a situation where the patient is slightly oversedated and rapid full reversal of the narcotic is not desired. Mix 0.4 mg of naloxone with 9 mL of normal saline to produce a concentration of 40 µg/mL. Administer 1 to 2 mL aliquots every 1 to 3 minutes to alleviate respiratory depression yet maintain the narcotic analgesic effect. (Reichman’s Emergency Medicine Procedures)
Don’t be afraid to call for help or back up. Being over-confident and getting in over your head can be problematic.
Be sure to talk with EMS when they drop off the patient in the ED. They can have critical info to give you that will make a difference in your managment.
For pediatric lacerations: LET applied with tegaderm works better than LET applied with gauze. Intra-nasal versed works well for sedation. Child life specialists can be very helpful to distract pediatric patients during laceration repair.
Lovell Procedural Sedation
For procedural sedation, we are usually shooting for moderate sedation. Sometimes we need to go to deep sedation for more painful procedures. Ketamine is in a different category altogether which is dissociative sedation. The patient retains blood pressure and airway reflexes with ketamine.
Moderate sedation is characterized by a depressed level of consciousness and a slower but purposeful motor response to simple verbal or tactile stimuli. Moderate sedation most closely matches the formerly used term "conscious sedation." Patients at this level generally have their eyes closed and respond slowly to verbal commands. Moderate sedation can be used for procedures in which detailed patient cooperation is not necessary, and muscular relaxation with diminished pain reaction is desired. During moderate sedation, the patient is usually able to maintain a patent airway with adequate respirations.9 Depending on the agent, the incidence of hypoxia and/or hypoventilation during moderate sedation is 10% to 30%.10,11,12 Procedures performed using moderate sedation include reduction of dislocated joints, thoracostomy tube insertion, and synchronized cardioversion. Agents used for moderate sedation in adults include propofol, etomidate, ketamine, methohexital, and the combination of fentanyl and midazolam.
Dissociative sedation is a type of moderate sedation. Dissociation is a state in which the cortical centers are prevented from receiving sensory stimuli, but cardiopulmonary activity and responses are preserved. Ketamine is the agent most commonly used for dissociative sedation.13
Deep sedation is characterized by a profoundly depressed level of consciousness, with a purposeful motor response elicited only after repeated or painful stimuli. Deep sedation may be required with procedures that are painful and require muscular relaxation with minimal patient reaction. The risk of losing airway patency or developing hypoxia or hypoventilation is greater with deep sedation than with moderate or minimal sedation.10,14,15 Examples of ED procedures sometimes requiring deep sedation are reducing fracture dislocations, open fracture reductions, and burn wound care. Deep sedation generally is achieved in the ED with the same agents as moderate sedation, but with larger or more frequent doses. (Tintinalli 8th edition)
Remember that propofol and etomidate do not provide analgesia. Propofol tends to have associated hypotension. Etomidate can stimulate vomiting. Etomidate can also cause myoclonus. Etomidate is associated with adrenal suppression but this is not a significant concern for brief procedural sedation.
Procedural sedation has low risk of aspiration. ACEP guidelines say NPO status has no relevance to procedural sedation.
FASTING STATE
There is no primary evidence that the risk of aspiration during procedural sedation is increased with recent oral intake.24,25,26 Current guidelines regarding the safe fasting period prior to procedural sedation were developed by expert consensus,27 and the American Society of Anesthesiologists guidelines for fasting prior to general anesthesia are of limited relevance to the risk of aspiration with ED procedural sedation.25 Thus recent food intake is not a contraindication.27 If the risk of aspiration is concerning, waiting 3 hours after the last oral intake before performing procedural sedation is associated with a low risk of aspiration, regardless of the level of sedation.27 (Tintinalli 8th edition)
Critical Questions and Recommendations
Question 1: In patients undergoing procedural sedation and analgesia in the ED, does preprocedural fasting demonstrate a reduction in the risk of emesis or aspiration?
Level B recommendations: Do not delay procedural sedation in adults or pediatrics in the ED based on fasting time. Preprocedural fasting for any duration has not demonstrated a reduced risk of emesis or aspiration when administering procedural sedation and analgesia. (ACEP Guideline)
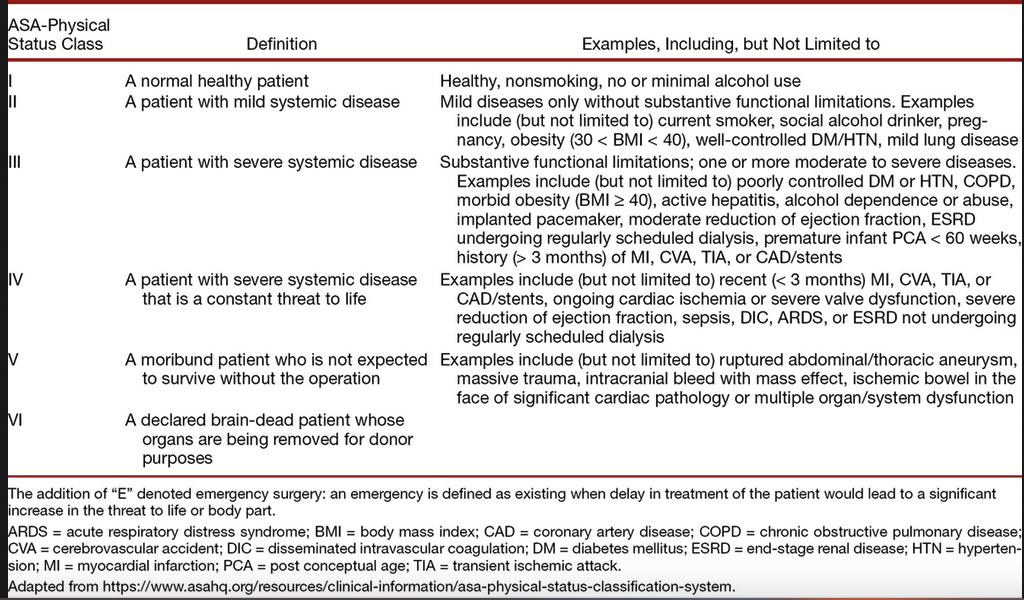
Complications are primarily determined by the interaction of the depth of sedation and the patient's current medical condition. A common tool for assessing the patient's underlying medical condition is the American Society of Anesthesiologists' physical status classification system.16 The risk of a significant complication from ED procedural sedation and analgesia in American Society of Anesthesiologists class I (healthy normal patient) and II (patient with mild systemic disease) is low, usually less than 5%.1,5,6,7,8 The risk of an adverse procedural sedation and analgesia event is correspondingly higher in patients with an American Society of Anesthesiologists class of III (patient with severe systemic disease) or IV (severe systemic disease that is a constant threat to life).17,18 (Tintinalli 8th edition)
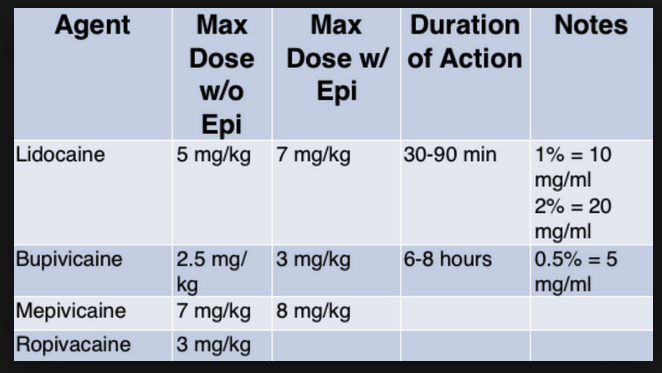
If you get over these doses, toxicity will manifest as either CNS symptoms/signs or Cardiovascular toxicity. Treat toxicity with benzos for seizures, ACLS medications for shock, and intralipid.
EM Faculty Sedation Workshop
Putman/DenOuden Sedation Debrief
Do a formal Time-Out with every sedation. Use the time-out to go over your mental checklist assuring you have everything you need (suction, ambu bag, capnometry, medications, reversal agents, rescue devices, etc).
Whatever sedation agent you choose, be prepared for the possible side effects and complications known for that medication.
After sedation is complete and the patient is awake, inform the patient of how the sedation went and whether there were any difficulties such as apnea or need for assisted ventilations or hypotension.
Patient can go home following procedural sedation if they score a 9. Basically, normal mental status, normal vitals, can walk, talk, and cough.