Wing M&M
No case details, just a few take home points.
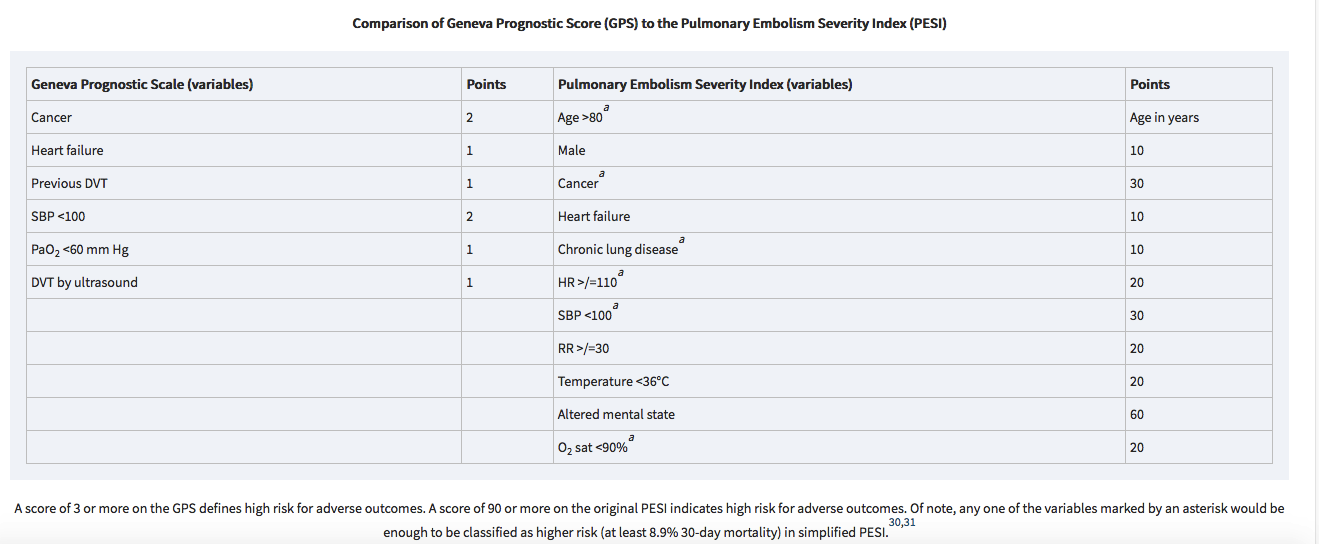
If a patient has signs of cardiac strain from PE or has other high risk factors (PESI score), consider admitting patient to the ICU or Step-down rather than the floor.
The reported sensitivity and specificity of CT in demonstrating right heart dysfunction are around 81% and 47% respectively 5.
Described features include:
abnormal position of the interventricular septum 1 flattening of the interventricular septum paradoxical interventricular septal bowing, i.e. towards the left ventricle
right ventricular enlargement (right ventricle bigger than the left ventricle)
pulmonary trunk enlargement (bigger than the aorta)
features of right heart failure: inferior vena caval contrast reflux, 1 dilated azygous venous system, dilated hepatic veins +/- with contrast reflux
D sign of LV
McConnell’s sign
All the above indicators should prompt consideration of admission to a higher level of care (Step down or ICU)
Putman HEENT Study Guide
Don’t try to close lacerations near the medial canthus on either the upper or lower eyelids. There can be an injury to the tear duct. Consult Ophthalmology.
TRAUMATIC IRITIS
Patients with posttraumatic iritis usually present 1 to 2 days after blunt trauma to the eye, complaining of photophobia, pain, and tearing. They often have marked blepharospasm and perilimbal injection (ciliary flush). Test for pain on accommodation by having the patient first look across the room at a distant object and then quickly focus on the examiner’s finger held several inches away. If near gaze causes pain, there is a high probability of iritis. The pupil may be large or small. Posttraumatic miosis develops secondary to spasm of the pupillary sphincter muscle, whereas posttraumatic mydriasis results when sphincter fibers are ruptured. Slit lamp examination will usually reveal cells in the anterior chamber, the hallmark of iritis.
Treat with a long-acting topical cycloplegic, such as 5% homatropine, four times a day for 1 week, oral anti-inflammatory medication, and dark sunglasses to decrease pain. Symptoms may persist for up to 1 week. Although ocular steroids decrease inflammation, prescribe them only after consultation with the ophthalmologist who will see the patient in follow-up.
We commonly associate HSV keratitis with a dendritic pattern on the cornea
HSV keratitis on the surface of the cornea
If HSV involves the deeper layers of the cornea, you can also see a disciform HSV keratitis.
Disciform HSV keratitis
Malignant otitis externa can be seen in diabetic patients. The most common complication is paralysis of the 7th cranial nerve.
Walchuk/Robinson Oral Boards
Case 1. 61yo female brought in by EMS with “stroke” symptoms. Dexi=155. Patient is altered and has slurred speech. Last time patient was normal is unclear. On further history, patient states she has been dizzy for a week. Patient is on phenytoin for seizures. Her phenytoin level is markedly elevated to 63. Treatment of phenytoin toxicity is supportive. Very severe toxicity may benefit from dialysis.
Phenytoin has a long and erratic absorption phase after oral overdose, so the decision to discharge or medically clear a patient for psychiatric evaluation cannot be based on one serum level. After acute ingestions, serum level should be measured every few hours. Patients with serious complications after an oral ingestion (seizures, coma, altered mental status, or significant ataxia) should be admitted for further evaluation and treatment. Those with mild symptoms should be observed in the ED and discharged once their levels of phenytoin are declining and they are clinically well. Mental health or psychiatric evaluation should be obtained, as indicated, in cases of intentional overdose. (Tintinalli 8th edition)
Case 2. 61 yo male brought in by EMS after a motorcycle crash. It was low speed accident and patient struck his head on the other vehicle. Patient has bilateral hand weakness. CT head and CT cervical spine show no acute abnormalities. MRI of the cervical spine shows:
Central Cord Syndrome is the most common spinal cord syndrome. It is seen most commonly in elderly patients with hyper-extension cervical spine injuries.
Signs of Central Cord Syndrome
The patient required C-spine stabilization and Neurosurgery consultation. Steroids are no longer recommended for central cord syndrome.
Case 3. 18yo male with right wrist injury from playing football.
Distal Radial-Ulnar Joint (DRUJ) dislocation should be suspected with any widening of the space between the distal radius and ulna. The lateral view shows to distal ulna displaced posterior to the radius.
Treatment is closed reduction, splinting the wrist, and orthopedic follow up. In some cases surgery is required.
Davis/Shroff/Friend ED BounceBacks
No case details, just a few take home points.
3 cases were presented. Each patient returned to the ED with a change in clinical picture. If the patient has an unclear diagnosis (belly pain, vague neurologic symptoms, back pain) and you are discharging them home, be sure to give clear discharge instructions describing signs/symptoms that should prompt return to the ED.
Dr. Williamson comment: These cases demonstrate the importance of communication with the patient. You want the patient to feel totally comfortable about returning to the ED for further evaluation.
Dr. Ryan comment: I tell the patient, “if your pain is getting worse, or you get a fever, or some new problem develops, that should not be happening. If it does happen, that is a sign that something is wrong and you need to come back to the ER.” Also give patients a time frame on when they should be feeling better. If they are not feeling better by then, they need to return for further evaluation.
Ebeledike/Johns Safety Lecture Choosing In-Patient Level of Care
Choosing the appropriate level of inpatient care for a specific patient (Floor, Telemetry, Step Down, or ICU) can be challenging.
Examples of diagnoses suitable for telemetry: Stable NSTEMI, syncope presumed to be cardiac, arrhythmia/heart blocks, pacemaker or ICD problem.
Examples of Patients suitable for Step-Down: Patient on a single pressor, chronically ventilated patients, patients requiring a high level of nursing care, and patients with significant risk of deterioration.
In general, if you are concerned that a patient may deteriorate or decompensate, strongly consider placing them in Step-Down rather than the floor.
If the patient is critically ill put them in the ICU.
Dennis Ryan comment: Consult with the ICU attending to collaborate on whether a patient belongs in Step-Down or the ICU to better determine level of care.
Editor’s comment: Suggested simplified algorithm. Stable patients go to the floor/med-tele/telemetry. If you are worried the patient may deteriorate consider Step-down. Critically ill patients go to ICU.
Lorenz/Shroff Visual Diagnosis
The Chiefs presented multiple clinical pictures for pattern recognition. This outstanding presentation moved too fast for me to capture.