Denk/Traylor STEMI Conference
Case 1. Following resuscitated cardiac arrest, if a patient has hypertension, it may be indicative of impending cardiogenic shock. The post-arrest patient maybe vasoconstricting to compensate for poor cardiac output.
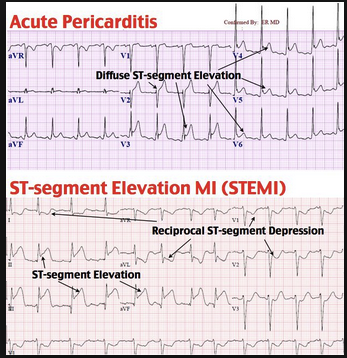
Case 2. If a patient has focal ST depression associated with ST elevation in other leads, you can't call it pericarditis.
Steps to distinguish pericarditis from STEMI:
Is there ST depression in a lead other than AVR or V1? This is a STEMI
Is there convex up or horizontal ST elevation? This is a STEMI
Is there ST elevation greater in III than II? This is a STEMI
Now look for PR depression in multiple leads… this suggests pericarditis (especially if there is a friction rub!)
From Life in the Fast Lane
A Right sided EKG looks for STEMI on right side. If the patient has right sided ST elevation this increases the probablility of RV dysfunction. If the patient has RV dysfunction they potentially will be very preload sensitive to nitroglycerin. Thus, in this setting of right sided ST elevation, nitro can cause hypotension.
Bedside echo can be useful in difficult cases where you are not sure if there is a STEMI. If you see wall motion abnormality or poor squeeze you know you have a STEMI.
Case 3. If you see ST depression in AVL you really gotta look for ST segment elevation in the Inferior leads. The ST depression in AVL may be more eye catching than subtle ST elevation inferiorly.
There is also a thing called Jone's sign which is a straight ST segment which suggests evolving STEMI. Jone's sign will occur prior to full-fledged ST elevation.
Straightening of the ST segment suggestive of STEMI
Case 4. When you see an EKG showing STEMI but the coronaries are clean, and the patient has a low EF, the patient has Takotsubo's.
Takotsubo's is more common in women. If a patient gets it once, they are at higher risk to get it again.
Characteristic apical balloning of left ventricle similar to octopus trap in Japan. Takotsubo's is Japanese for octopus trap.
Menon/Twanow Oral Boards
Case 1. 50yo male with chest pain s/p mvc. Heart rate 120, BP=160/120. Patient has signs of abrasions to left chest. Patient has left abdominal tenderness. FAST is negative. CTA shows aortic injury.
Extreme example of CXR showing widened mediastinum and multiple classic findings of blunt aortic injury.
CTA shows in aortic injury
You want to bring down pulse and BP to manage the shear force on aortic wall. Give esmolol and a vasodilator such as nicardipine or nitroprusside.
Case 2. 21yo male with right shoulder pain. Patient injured right shoulder playing rugby. Vitals are OK.
Posterior shoulder dislocation. Y view on right shows humeral head posterior to scapula and Y.
With posterior dislocation, humeral head looks like golf ball on a tee. With anterior dislocation, humeral head looks like a golf club head.
Posterior dislocations are classically associated with seizures or electrical shock/lightning strike.
Case 3. 7yo with rash and joint pain. Vitals all OK. Rash on lower extremities c/w HSP
HSP rash
HSP is the most common vasculitis in childhood. It is an IGA vasculitis. Patients are at risk for intussusception, renal disease (nephritis), and joint pain. Management is supportive. Steroids can be given to treat severe pain but in general steroids are not indicated. Steroids are not useful for renal disease and they do not shorten course of illness.
Burns/Denk Using Echo to Calculate Cardiac Output and Rescue Echo
Cardiac Output=Stroke volume X heart rate
U/S calculation of stroke volume= Pi (LVOT diameter/2)squared X VTI
Stroke volume is measured with U/S by using parasternal long view. Left Ventricular Outflow Tract (LVOT) diameter is measure the width of LV outflow tract when valve leaflets are open. Measure the width just proximal to aortic valve leaflets. The computer on the machine squares this measurement to come up with the stroke volume. Normal width will be around 2cm.
VTI is calculated by ultrasound machine when using the Apical 5 chamber view.
LVOT diameter normal is 2. VTI normal is 15-20. Normal CO=4-6
editor' s note: This was an outstanding, highly technical discussion of calculating cardiac output with U/S. I had difficulty encapsulating the discussion in these notes. That is based on my own unfamiliarity with the procedure and the math.
Rescue Echo looks for causes of hypotension
Rescue echo utilizes parasternal, subcostal, and apical views.
The critical Rescue Echo diagnoses: LV dysfunction, RV dysfunction, severe valvular dysfunction, systolic anterior motion abnormalities SAM, cardiac tamponade, and hypovolemia.
Katiyar Billing and Coding
Critical care billing gives 6.33 RVU's for first 30 minutes. That's more than a level 5 chart which is 4.9 RVU's.
Critical care requires risk of life threatening deterioration requiring the highest level of physician attention.
The critical charge covers 30-74 minutes of critical care. You cannot include the time you spent performing procedures such as intubation and central line.
Critical care billing requires that the attending physician is giving direct attention to the patient either at the bedside or reviewing diagnostic studies, discussing with consultants and family members, or documenting. The total time does not need to be continuous. You can hit 30-74 minutes of critical care time by caring for a patient intermittently. The time you count towards critical care just has to be focused entirely on that patient and not include procedure time.
You need to document the time you spent and how you spent it. You have to document the risk of deterioration if the patient was not treated. It is beneficial to document all the re-evals you performed on the patient. It is beneficial to document the timeline of when you evaluated, re-evaluated, consulted, reviewed diagnostics, and had discussions, etc.