Velamati/Lorenz Oral Boards
Case 1. 3 yo male presents with bloody diarrhea. Patient has abdominal pain and dark urine. Multiple family members had diarrhea after eating at a BBQ. Patient has elevated blood pressure to 118/80. On exam patient has some extremity edema, abdominal tenderness, and a palpable liver edge. Labs c/w hemolysis, and abnormal renal function tests.
Diagnosis is HUS. HUS presents about 3-7 days after ingestion of contaminated food.
Shiga-toxin HUS usually does not need plasmaphoresis.
Harwood comment: Atypical HUS can be treated with monoclonal antibody eculizmab.
Detailed graphic differentiating TTP, atypical HUS, and Shiga-Toxin HUS
Case2. 30 yo female with right leg pain and inability to walk. Vitals are normal. Patient was playing soccer when she felt her leg buckle. Since then she can not bear weight on right leg. Patient has a history of lupus and steroid use. On exam, right knee has large effusion and patient cannot extend right knee against gravity. Neurovascular status intact distal right lower extremity.
Left image is normal position of patella. Right image is a superiorly displaced patella due to rupture of patellar tendon.
Diagnosis is patellar tendon rupture. Management is knee immobilizer and crutches and orthopedic consultation for operative repair.
Case 3. 12 yo male presents with confusion and difficulty walking. Accucheck is 59. Vitals are significant for hypotension. Patient was given D25 rapidly. Skin is bronze colored. Labs showed hyponatremia and hyperkalemia.
Diagnosis was adrenal insufficiency. Patient was treated with IV hydrocortisone. CT head was negative. Vitals improved with IV fluids and IV hydrocortisone. For severe hyponatremia and neurologic signs, treat with hypertonic saline. Consult endocrinology.
Yapo Non-Accidental Trauma
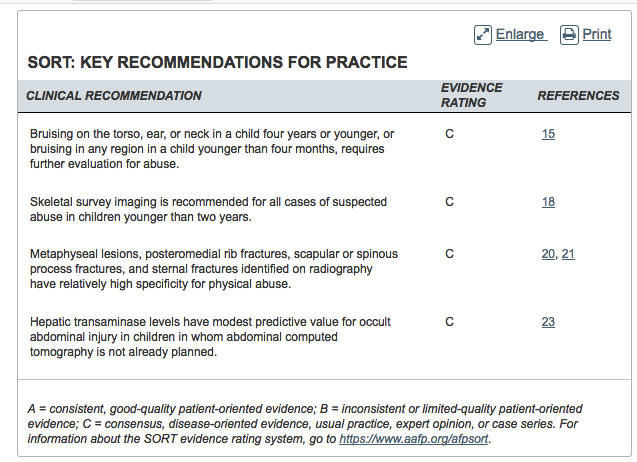
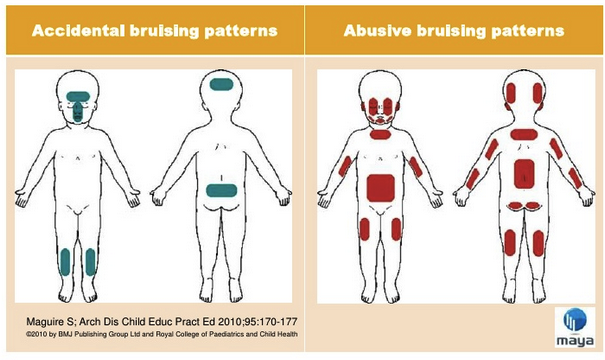
Bruising on ears or neck in a child under age 4 is concerning for abuse.
Slate grey macules (Mongolian spots) are not signs of abuse.
Only about 12% of abusive abdominal injures will have abdominal bruising. Intra-abdominal organs are more susceptible to injury due to pediatric anatomic differences from adults (less abdominal wall musculature, more pliable ribs, horizontal diaphragm). Abusive injury to the abdomen has higher mortality than non-abusive injuries. Abdominal injuries present 3.5 days after trauma. Symptoms will be vague. Non-abuse related falls do not usually cause intra-abdominal injury.
The duodenum is susceptible to abusive trauma because it has both fixed and mobile portions.
The liver is the most common solid abdominal organ injured from abuse.
Pediatrics 2009 LInberg: If AST or ALT is >80 you have to consider intra-abdominal injury. The liklihood ratio for AST or ALT>80 for identifying intra-abdominal injury is 4.3. Draw this lab in patients under 5 years of age in whom you are screening for non-accidental trauma. If ALT or AST is over 80 get abdominal imaging. Draw ALT and AST if a patient has fracture, head injury or other injury raising suspicion for abuse.
Skeletal survey is manadatory in age <2. Case by case basis for skeletal survey in ages 2-5. No utility of skeletal survey in children over age 5.
Scan an infant's head for any alteration in mental status, any sign of abuse in a child less than 6 months of age, and any child with suspicion for shaken baby syndrome. Dr. Yappo said that you should strongly consider getting a CT head in a child less than 6 months with any evidence of abusive injury even if there is no sign of head injury.
Mullen 5 slide Follow Up
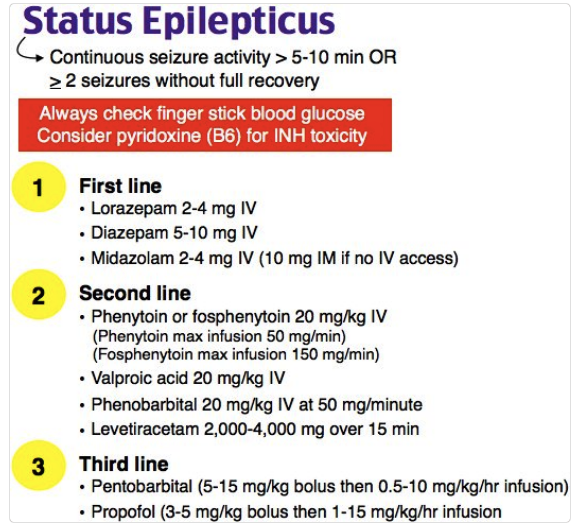
If a patient is unresponsive after a seizure, consider sub-clinical status epilepticus. If you have a suspicion of sub-clinical status epilepticus you should get an EEG to assess for ongoing seizures.
Management of Status Epilepticus. If you have to intubate, consider succinylcholine rather than rocuronium to keep the time of neuromuscular blockade as brief as possible. You don't want to obscure seizure activity with neuromuscular blockade.
Ebeledike 5 Slide Follow Up
Male patient with groin pain. Dr. Ebeledike discussed hernias.
Adlington Care of Sexual Assault Patients
If sexual assault occurred within 7 days of ED presentation we have to offer evidence collection, date rate drug testing, STI testing, emergency contraception, and HIV prophylaxis.
If sexual assault occurred more than 7 days prior, evaluation is done on a case by case basis.
There is a macro in our FirstNet power chart in the medical decision making section (**sexual assault) that covers all the areas of required documentation.
Legal Definition of penetration: Any contact between the the labia even if minimal/superficial is considered penetration.
New concept (at least for me) avoid the word "alleged"in your documentation. It may convey a negative connotation to the patient's history. We had a discussion about the challenges of avoiding this term in documenting the H&P and diagnosis. (editor's note) It may be challenging in certain circumstances to find an acceptable alternative term. The presenter said she would send us suggested coding alternatives.
New concept (at least for me) In pre-pubescent children, do not interview them about what happened. That interview needs to occur with the state's attorney and with a trained forensic interviewer.
Any age person can consent to an exam and evidence collection after sexual assault or abuse. Don't do an exam or collect evidence if patient refuses or is resisting exam. If you have to use force or sedation to do an exam, don't do it.
SANE trained nurses can do the entire evidence collection and exam independently. ED nurse without SANE training cannot do the genital or anal exam. The physician will need to perform this portion of the exam. Everyone in the room during evidence collection must have gown, hair covering, shoe covers, and a mask in order to keep examiners/care givers DNA from getting into specimens.
On the forensic documentation form you have to write "no injury identified" in each picture section of any area you examined. If nothing is written in a section of the forensic documentation, the court assumes no exam of that area was performed.
In prepubescent female children the swabs for evidence collection are obtained by lightly touching superficially the mucosal area between the labia.
Hawkins EKG's
Dr. Hawkins reviewed multiple EKG's in a very interactive fashion. I was unable to encapsulate this lecture in these notes.
Chinwala Safety Lecture
Med Tele and Tele have the same nursing ratios for patient care. They have the same monitors. Patients with a cardiac problem (nstemi, cardiac syncope, arrythmia, new-onset CHF) who require monitoring should go to tele. Patients with a medical problem (sepsis, PE, hyperkalemia, CVA, etoh withdrawal, recurrent CHF) who require monitoring should go to med-tele.
Dr. Chinwala also discussed how we triage patients for CT scanning.
Pastore Safety Lecture
Dr. Pastore discussed the CODE 15 process for behavioral health emergencies.
Twanow Safety Lecture
Dr. Twanow discussed active shooter scenarios.
29% of hospital shootings occurred in the ED. 23% of hospital shootings were due to a shooter who took away the security guard's gun.
Active shooter scenarios occur in about 15 minutes and frequently end before police arrive.
Basic plan: Alert those around you. Then RUN>>>>Hide>>>>Fight in that order.
The 4 A's of an Active Shooter situation: Accept that a life threatening active shooter situation is occurring, Assess what you should do, Act for your own and others safety, Alert law enforcement. (editors note: Accept is probably the most important factor. The others will come naturally after that.)
Shroff ICEP Presentation
Dr. Shroff gave a preview of her upcoming ICEP Spring Symposium presentation.