Conference Notes 7-16-2013 Todays’ focus: ED CODEs
There are images in this document. If you don’t see them, scroll to the bottom and click “read in browser”
McKean Intial Mangement of Sick Patients
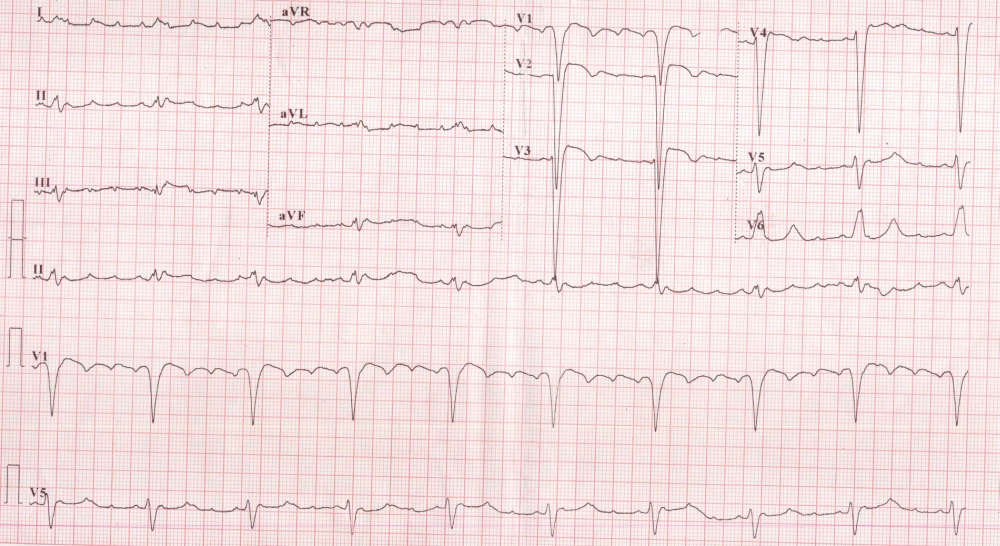
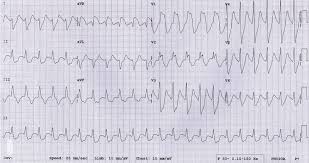
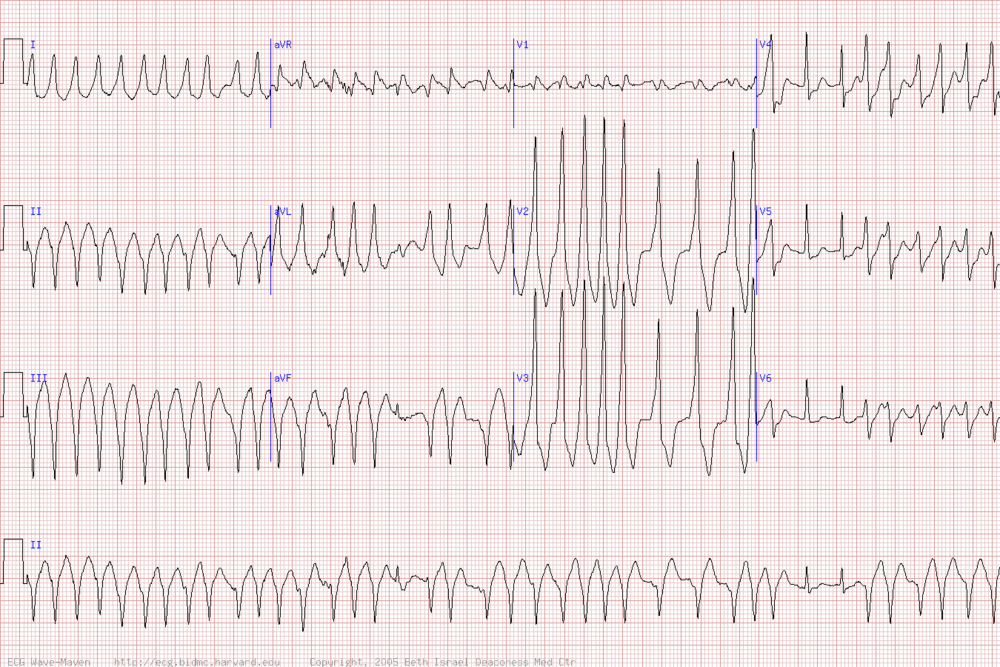
Case 1 Hyperkalemia most rapidly identified on EKG. Treat with calcium, insulin/glucose, bicarb, kayexelate
Hyperkalemic EKG
Case 2 Decompensated CHF Girzadas comment: I follow Harwood’s Maxim that if you are intubating an acute CHF exacerbation patient you have failed. These are patients that if you aggressively treat with sublingual and hi dose IV ntg, bipap and alittle bit of diuresis you can turn them around in 30-60 minutes. Harwood agreed.
Case 3 Septic/hypotensive patients need aggressive IV fluids 30ml/KG in short order. IV antibiotics are also needed. Elise comment: In septic patients do a complete exam for possible sources. Look specifically for pneumonia/uti/abdominal infectious process/cns infectious signs/skin pressure ulcerations or cellulitis or necrotizing fasciitis. Tekwani comment: make sure you get 2 blood cultures.
C Kulstad comment: For all these really sick patients make sure your attending is in the room with you. These patients require aggressive care including the ED attending at bedside.
Kettaneh Intraosseous Lines
IO lines are fast, they work 97% of the time, cost is about $100 and you can give fluids and medications and get blood samples. It can be a bridge access device prior to getting a central line. Consider in status epilepticus and in sepsis patients with access problems. IO lines give access to central circulation.
Contraindications: Proximal fx, overlying cellulitis, previous IO line in the same bone
Pain with infusion is a common side effect. 2.0 ml of 2% of cardiac lidocaine infused into the IO line can make Infusions less painful.
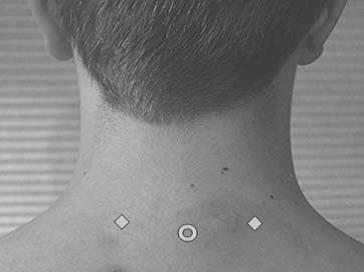
Proximal humerus access site: Technique to find best site is put pt’s hand on umbilicus. Palpate for notch on the humeral head. Lovell and Girzadas comment: It’s ok to just palpate for boney prominence of humerus that has the least soft tissue overlying it. This is not rocket science, the goal is to get access in the bone. It doesn’t have to be in a perfect position.
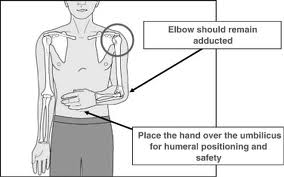

Proximal Humerus SITE/Angle for IO Line
Proximal tibia access site: 2 finger breadths below tibial tuberosity on medial aspect.
There is some data to suggest the proximal humerus site has more rapid access to the central circulation. However, the proximal tibial site has rapid transport to central circulation also. Probably should choose access site based on ease of access.
Lines on the IO needle are at 5mm demarcations. You should get needle to surface of bone prior to drilling into the bone. When needle is on bone surface, you should have at least one line on the needle visible outside the skin. Seeing that line assures you that you have enough needle length to successfully access the bone and make sure it is secure.
Aspiration of blood confirms IO placement. Kasia comment : No blood back on first aspiration does not necessarily mean you are not in the bone. Harwood comment: You can use this aspirated blood for labs such as type and screen/HGB/Bun and Cr. Elise comment: You don’t always need to numb up the skin in urgent situations. 2.0 ml of 2% of cardiac lidocaine infused into the IO line can make Infusions less painful. Elise comment: 2-3 ml from an amp of lidocaine should do the trick. Painful infusion can be mistaken for improper IO placement but it really means that you are infusing into the bone and it is painful. You need to infuse lido as described to decrease pain. Bone pain with infusions is actually a sign you are in the bone properly in an awake patient. Flush lines prior to infusions. You may need pressure bag to get fluids/drugs infused.
Potassium WBC, Platelet and bicarb are not reliable to test with IO obtained blood.
You can give virtually any med or fluid or transfusion through IO. You can even give pressors and TPA.
IO lines are recommended to be removed by 24 hours. Remove by hooking up a 10ml syringe. Turn the needle clockwise and pull back gently.
Elise comment: In a code situation with 1or 2 failed peripheral IV attempts go right to IO line before central line.
Purnell ABG’s
3 step approach
- Calculate the anion gap (identify an anion gap acidosis) AG=Na –(Hco3 +CL). NL AG=15. Lithium or low albumin can shrink the gap. In that light, an end-stage cirrhotic with normal or high gap is in metabolic trouble.
- Calculate the delta gap (identify hidden metabolic abnormalities). Change in the AG should equal the change in HCO3. For every 1 change in AG, the HCO3 should go down by 1. Normal AG=15, Normal HCO3=24. They should both normall change in a 1:1 ratio. If not, some metabolic derangement is going on. If bicarb is too high you have a primary metabolic acidosis. If bicarb is too low then you have a non-anion gap metabolic acidosis.
- Apply the rule of 15 (identify respiratory acidosis/alkalosis) HCO3 + 15 should= pCO2 +/-2 and also equal the last two digits of the ph. If not, another primary respiratory problem is going on. Pco2 too high=respiratory acidosis, Pco2 too low=respiratory alkalosis.
Examples: Ph of 7.25 HCO3=15 PCO2=25 NA=140 Cl=105
Step 1: 140- (105+15)=20 Thus there is an anion gap acidosis
Step 2: Change in AG from normal is 5. Change in bicarb from normal is 9. Bicarb went down more than expected, thuse we have a non-ion gap acidosis.
Step 3: 15+ 15=30 The PCO2 is too low, thus we have a respiratory acidosis.
We just diagnosed a triple acid/base disorder.
DDX of different acid base abnormalities
High AG Acidosis: CAT MUDPILES is the mnemonic. CO/CN, AKA, Toluene, Methanol, Uremia, DKA, Paraldehyde, INH?IRON, Lactate, Ethylene glycol, ASA
Non AG Acidosis: HARDUP Hyperventilation, addisons/acetazolamide, RTA, diarrhea (by far the most common reason), ureteral diversion, P(missed the P in the mnemonic)
Metabolic Alkalosis: dehydrated, cushing syndrome
Respiratory alkalosis: hyperventilation, salicylate poisoning, pregnancy, brain tumors, anemia, high altitude
Respiratory acidosis: Obesity, copd, insufficient ventilation
Herrmann Non-Invasive Ventilation
Bipap decreases intubations and hospital length of stay. Non-invasive ventilation means the interface between O2 and patient is a mask, not an ET tube.
EPAP=PEEP=CPAP
IPAP=pressure support
BIPAP= EPAP +IPAP= CPAP +PS
Funny analogy: CPAP is positive end expiratory pressure which functions basically as a hair dryer in your mouth.
Idications: COPD, CHF, Asthma, pneumonia, atelectasis, neuromuscular disease, palliative care. Can be considered in any dyspneic patient.
Absolute Contraindications: need for intubation, decreased level of consciousness, vomiting or copious oral secretions, facial deformity.
Ventilation improved by IPAP. Oxygenation improved by EPAP.
BIPAP improves CHF by decreaseing preload and afterload. Forces fluid out of alveoli. CPAP reduces in-hospital mortality. BIPAP and CPAP reduce intubation with no increased risk of MI.
In COPD, BIPAP improves laminar flow, stents open collapsing airways. Reduces mortality and intubation.
AVAPS: Averaged volume assured pressure support. Gives a specified tidal volume, pressure regulated non-invasive ventilation. Consider in hypercapnic respiratory failure.
Settings: Standard 12 IPAP/ 5 EPAP, COPD 15 IPAP/5 EPAP or AVAPS,
Elise comment: RT’s are not totally comfortable with AVAPS. Good time to use AVAPS is with the hypercapneic COPD’ers. It gives them better tidal volumes.
PUtman STEMI
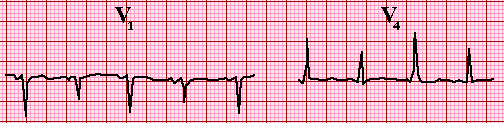
Posterior MI: Posterior leads only require 0.5mm ST elevation to meet STEMI criteria.
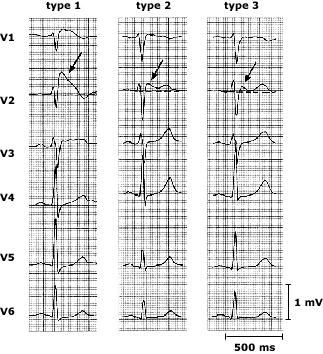
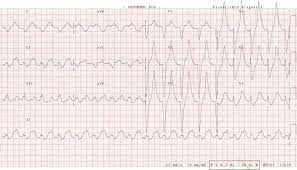
Sgarbossa criteria: STEMI in the setting of LBBB. STE that is concordant, STD that is concordant, STE>5mm that is discordant (less specific)
STEMI management: If you are in an ED without a cath lab, if you can transfer a patient to a hospital with a cath lab in under two hours your should transfer rather than give thrombolytics. Other standard treatment for STEMI: ASA 325 mg. Plavix 600mg. Give unfractionated heparin.
Thrombolytics: Harmful for ST depression alone unless a true posterior MI. If giving lytics, give ASA 325mg, Plavix 300mg or 75mg if patient is older than 75yo. Also give unfractionated heparin.
Beta blockers: Give within the first 24hours unless CHF, shock, heart block, asthma. Probably does not need to be given in the ED unless you need to slow heart rate.
STEMI and Cardiogenic Shock all need Cardiac Cath and balloon pump irrespective of time delay.
Mckean comment: The big STEMI mimic to have your guard up for is aortic dissection. Girzadas comment: The one thing that will kill a STEMI patient in the ED is V-Fib. Be prepared to defibrillate. Elise/Christine comment: Cardiac surgeons are for the most part OK with plavix being given pretty much as a default to our STEMI patients. Mistry comment: Don’t worry too much about the duration of a patient’s symptoms prior to arrival in the ED. You can’t be sure when the angina proceeded to infarct. Documentation of reason for delay to PCI is critical.
Elise’s added info:
1. Alteplase (TPA) dosing for acute MI:
Accelerated infusion of alteplase for AMI consists of a 15-mg IV bolus followed by 0.75 mg/kg (up to 50 mg) IV over 30 minutes and then 0.5 mg/kg (up to 35 mg) IV over 60 minutes. The maximum total dose is 100 mg for patients weighing more than 67 kg.
2. Plavix dosing if patient already on Plavix and presents with STEMI:
I just looked through 2013 AHA STEMI guidelines again, and nothing I can find about folks who are already taking Plavix...like Andrej said, reasonable to re-load them with 600 mg, or can discuss with Cardiology.
3. Sgarbossa accuracy to predict MI in LBBB. Criteria are not equally accurate; there are different points for each criteria, the first one most specific/useful.
The three Sgarbossa criteria used to diagnose infarction in patients with LBBB are:
- · Concordant ST elevation > 1mm in leads with a positive QRS complex (score 5)
- · Concordant ST depression > 1 mm in V1-V3 (score 3)
- · Excessively discordant ST elevation > 5 mm
A total score of ≥ 3 has a specificity of 90% for diagnosing myocardial infarction.
Maletich Post-Arrest Care
Hemodynamic instability is common after resuscitation. Have a pressor like norepi ready to go if needed.
Get them to cath lab. For sure all STEMIs but even 50% of non-STEMI’s wil benefit from cardiac cath after cardiac arrest. Therapuetic hypothermia has been shown by RCT’s to improve neurologic outcome after resuscitation after shockable rhythms. Anyone who is not following commands or GCS <8 should get cooled after resuscitation from cardiac arrest. Cool patient to 33 degrees for 24 hours then rewarm to 37 degrees and control temp for 48 hours.
Give midazolam to control shivering We also use buspirone, magnesium, and Demerol. Bradycardia is expected with cooling. There is cold dieresis. Hypokalemia can develop with hypothermia and it will improve with re-warming. No need to replete potassium if 3.4 or above.
McKean/Elise comment: Can’t prognosticate patients’ neuro status before 72 hours after therapeutic hypothermia. Elise comment: There is time urgency for cooling. Time is brain cells. Get cooling started ASAP after resuscitation. Chintan comment: We can’t improve patients’ pre-arrest neuro status with cooling.
Wise U/S in the Critically Ill Patient
Parasternal long and subxyphoid views are the money shots for evaluating the critically ill patient.
Pericardial effusion: 100ml or less only posteriorly in systole. >100ml you will see posteriorly and anteriorly on parasternal long view.
RV normally should be about 0.5 the size of the LV. If the RV is similar in size or larger than the LV you have to start considering PE.
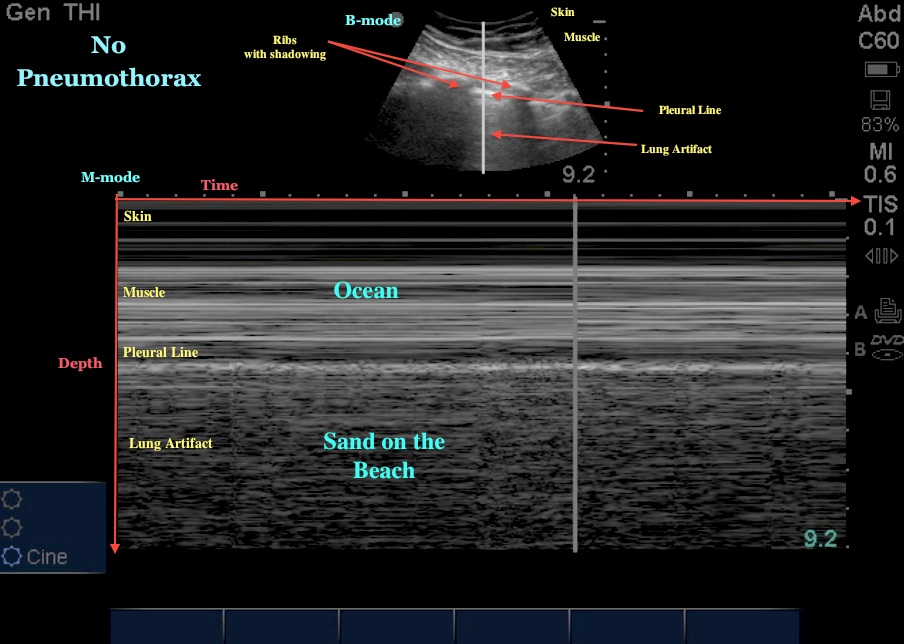
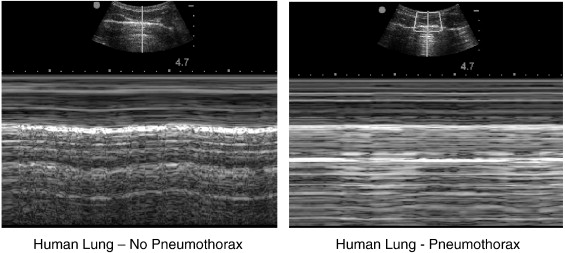
Lung U/S is useful to identify pneumothorax, pulmonary edema, and effusions.
Pneumothorax won’t have sliding pleura on B mode and no “beach” in M mode.
Pulmonary edema is identified with “headlights in the fog” . Copd is identified by increased A lines and no headlights in the fog. Pneumonia will have unilateral or isolated area “headlights in the fog”.
Small Group Workshop EGDT for the SEPSIS Patient
Critical actions:
Early identification of sepsis based on 2 or more SIRS criteria and evidence of infection.
30ml/kg IV fluid bolus within the first hour based on clinical suspicion of sepsis.
Get two blood cultures and lactate in addition to other basic labs
IV antibiotics (Vanco/Zosyn) within an hour
If pt is hypotensive despite fluid bolus or lactate >4 place CVP line. Give fluid boluses up to a CVP of 8-12
If still hypotensive start IV norepinepherine.
Check SCVO2 and trend lactates. If SCVO2 low or lactate not improving consider transfusion to get hgb >7, and consider intubation to improve oxygenation and decrease work of breathing.
If still not doing well, can add dobutamine as an inotrope.
There was a question as to why some clearly septic patients have low lactates. Elise discussion: In his podcast, Scott Weingart discusses caring for patients with minimally bumped lactates who are clinically septic. It's hypothesized that lactate production is driven by surges in catecholamine production, and in some patients, especially the elderly, their ability to produce catecholamines is burnt out, and lactate may not be significantly elevated. Still need to treat them as septic.