TOXICOLOGY CASE OF THE MONTH
FEBRUARY 2014
55yoM h/o seizure disorder, Hepatitis C, HTN, DM, CKD, meningioma s/p resection and hepatic encephalopathy presents from assisted living for mental status changes. It is his second visit in the last 48 hours for similar symptoms. He has been difficult to arouse and was noted to have an unsteady gait. He denies fall or intentional ingestion. He is unsure whether he has had any recent medication changes. He complains of generalized weakness and unsteadiness.
Medications: Albuterol, Atorvastatin, Clonidine, Gabapentin, Hydralazine, Hydroxyzine, Insulin, Lactulose, Nifedipine, Phenytoin, Terazosin
Physical exam:
VS 97.2 142/84 69 18 100% RA
General: Awake, alert and oriented x3 though unsure of purpose of hospitalization, no acute distress, cooperative
HEENT: PERRL - 4mm to 3mm b/l, EOMI, + b/l horizontal nystagmus
Neck: supple no asymmetry
CV: RRR no m/r/g
Lungs: CTA b/l
Abdomen: + BS, soft, nontender,nondistended
Extremities: WWP, 2+ pulses in b/l radial, PT, DP, no clonus, no asterixis
Neuro: CN II-XII grossly intact, 5/5 strength in b/l UE and LE, sensation intact b/l UE and LE, wide-based ataxic gait with b/l dysmetria on finger to nose
Skin: warm, dry, no diaphoresis, no rash or lesions
1. What is this patient’s differential diagnosis?
- Non-tox causes: hepatic encephalopathy, infection, incranial mass/hemorrhage, CVA
- Toxicology differential:
- Most likely antiepileptic given presentation - Phenytoin or Gabapentin
- Hydroxyzine can cause somnolence but would expect anticholinergic presentation (elevated temperature and HR, dry skin and mucous membranes, delirium, urinary retention, etc)
- Clonidine can cause somnolence but would expect different toxidrome (opioid-like - MS depression with respiratory depression, + VS abnormalities - hypotension & bradycardia)
2. What is the differential diagnosis of nystagmus in toxicology?
- Many drugs and toxins cause nystagmus - usually horizontal. Here are a few examples:
- Anti-epileptics
- Barbiturates
- Carbamazepine
- Phenytoin
- Gabapentin
- Ethanol
- Scorpion Envenomation
- Isoniazid
- PCP (horizontal, vertical, rotatory)
Labs:
Initial presentation:
- 140/4.4/109/25/44/2.21/214
- AST 30 ALT 41 Bili 0.2 Albumin 2.5
- Phenytoin 14 mcg/mL (ref range 10-20)
- Ammonia 25
Second presentation:
- 136/4.8/107/22/49/2.0/200
- AST 41 ALT 31 Bili 0.1 Albumin 2.5
- Phenytoin 20 mcg/mL (ref range 10-20)
- Ammonia 17
(Creatinine is at baseline)
CT head with no acute change
3. How do these labs change your differential diagnosis? What is the culprit agent?
- The patient's signs and symptoms are consistent with Phenytoin toxicity
- Phenytoin is >90% Protein-bound - level needs to be corrected for serum albumin
- This patient is at risk - hypoalbuminemia due to liver disease
4. What are the clinical characteristics of phenytoin toxicity?
- Mild to moderate: horizontal nystagmus, ataxia, dysarthria
- Less common: nausea, vomiting, diplopia, hyperglycemia, agitation, irritability
- Severe: stupor, coma, respiratory arrest
- Rare seizures have been reported (though should always consider an alternative cause of seizures in a phenytoin-poisoned patient)
- Death extremely rare
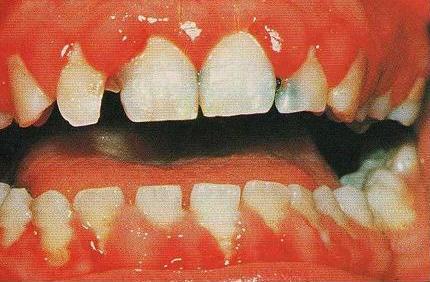
- Gingival hyperplasia is indicative of chronic use - may clue physician into diagnosis
- Reported cause of Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis
- Propylene glycol component in IV preparations can cause myocardial depression - hypotension, bradycardia
- Cardiac toxicity does NOT occur with oral overdose or with fosphenytoin
5. What are the applicable pharmacokinetics?
- Absorption can be slow and unpredictable and in acute ingestion peak effects may be delayed
- 90% protein bound
- Hepatic elimination – zero order kinetics near therapeutic range – half-life increases as levels rise
6. What is the formula to correct the serum phenytoin level?
- Corrected Phenytoin = Measured phenytoin level/(0.2 x Albumin + 0.1)
- Available on most medical calculators
- This patient's correct levels are 23 and 33 respectively using this formula
7. How is phenytoin toxicity managed?
- Hold offending medication
- Most importantly: protect the patient from self-injury caused by ataxia
- This may require the patient to be admitted to the hospital for fall prevention
- For PO toxicity - do not need to be admitted to a tele floor (common misconception)
- Can also d/c home with reliable family member if close follow up with neurologist or PMD can be arranged, if circumstances are appropriate
- If seizures occur - consider alternative cause, treat with other anticonvulsants (benzodiazepines generally recommended for toxicology-related seizures)
- If hypotension occurs with IV administration - stop infusion, administed IV fluids/vasopressors as necessary
- No antidote, no role for dialysis. May consider activated charcoal if appropriate though most often toxicity is chronic.
- This may require the patient to be admitted to the hospital for fall prevention
Case Conclusion:
- Send-out free phenytoin level was 4 ug/mL (ref range 1-2), % free 21.6% (ref range 8-14%)
- Culprit medication was held and patient recovered clinically after several days
- Was discharged home with a lower medication dose
Pearls to remember:
- Phenytoin toxicity si/sx: ataxia, nystagmus, dysarthria
- High protein binding - level should be corrected for serum albumin
- Treatment is supportive - fall prevention, hold medication, dose adjustment
- Cardiac monitoring not necessary for toxicity due to oral preparations