Conference Notes 10-8-2014
Cash/Williamson Oral Boards
Case 1. 45yo Male with fever, 105/80, P=123. PMH of DM. Patient is poorly compliant with his insulin. Careful exam shows cellulitis in the genital area. Labs show marked hyperglycemia/DKA. X-ray of pelvis shows subQ air. Critical actions: Emergent surgical consultation, broad spectrum IV antibiotics (Vanc/Zosyn/Flagyl or Clindamycin), IV insulin.
*SubQ air associated with Fournier’s gangrene
Case 2. 2yo female with vomiting and decreased level of consciousness. BP=40. P=180, T=37.5. Baby sitter noted that child had ingested some pills. Patient was vomiting and required intubation to protect airway. Big clue was that mom was pregnant. Efforts at contacting the patient’s mom revealed that she was taking iron supplements. Serum iron level was markedly elevated. Critical actions: Intubation, IV fluids in 20mg/kg boluses, diagnose iron toxicity, check blood glucose level, give deferoxamine. Consider whole bowel irrigation if iron tablets are seen on abdominal imaging. Toxicity is based on the quantity of elemental iron ingested. 325mg of ferrous sulfate=65mg of elemental iron. 50mg/KG or greater ingestions of elemental iron are more likely to cause serious symptoms.
Case 3. 38 yo male fell and injured his right arm. Vital signs are normal. Patient has gross deformity of right forearm. There is an associated laceration of the right forearm. Xray shows galeazzi fracture.

*Galeazzi Fracture (fracture of the distal third of the radius with with associated distal radio-ulnar dislocation)
Critical actions: IV antibiotics for open fracture, urgent orthopedic consultation for washout of open fracture and ORIF .
Board Pearls: Be cautious with how you order fluids for kids. You can’t just say hang a liter of fluid for a 2 yo child. Frequent re-assessment of the patient helps you work through the case and helps you keep the patient updated.
Clinical Pearls: Open fractures should get IV pain medication. Be cautious with any laceration or puncture wound associated with a fracture. You should assume it is an open fracture initially. Fournier’s gangrene mandates rapid surgical debridement. Serum Iron level great than 500 portends serious system toxicity.
Faculty Discussion: Elise comments: Be prepared for the boards and future practice to manage DKA without a protocol. Many places don’t have protocols like our DKA protocol. Be able to say/discuss the key parts of patient management protocols like the DKA protocol or the Sepsis protocol. That way you know it if you practice in another ED and you are able to discuss the management when taking oral boards. There is no need for an insulin bolus when managing DKA. Do an airway assessment first in any unstable patient. Get an EKG right away in any unstable patient. The history that mom is pregnant was a clue that the ingestion was iron. Use every asset to identify the toxin on an oral boards case. Send police to the house if necessary. Everything the examiner says is a clue to the case. Be very specific and direct with consultants when taking the boards. Girzadas comment: Remember two numbers for iron poisoning: (50/500) 50mg/kg ingestions can cause serious toxicity. Serum iron level of 500 is a marker for serious systemic toxicity. You have to get a serum iron level within 4-6 hours after ingestion unless it is slow release. After 8 hours the serum iron level can be deceivingly low.
Negro Morbidity & Mortality
58yo male with HX of CABG, previous repair OF A Type A aortic dissection, aortic valve replacement. Patient is on Coumadin. Patient had presenting complaint of chest pain and sob. Patient is ill appearing. Pulses equal in all extremities. Lungs are clear. Abdomen is benign. Neurologic exam is normal.
EKG showed no acute ST changes.
CTA chest was unremarkable.
TROP and BNP was normal. INR was 1.1.
Confirmation Bias: Tendency to search for and prioritize information that confirms one’s hypothesis or belief. Bret felt he was drawn into confirmation bias based on his concerns about chest pain in the setting of CAD and previous Aortic dissection. Consequently he proceeded with a chest pain work up.
Anchor Bias: You are influenced by the first clue you identify. Bret gave each audience member 1 of two long multiplication problems (see below) and allowed 5 seconds to solve the problem.
1x2x3x4x5x6x7x8
8x7x6x5x4x3x2x1
People who did the first problem estimated on average the answer to be around 250
People who did the second problem estimated on average around 2,250
The actual answer to both problems is 40,320.
It demonstrates the concept that we anchor to the first clue we get.
The chest pain work up that Bret initially anchored on came up with no diagnosis, and the patient was still ill-appearing. Bret goes back to re-evaluate the patient and revise his work up plan. He now identifies that the patient’s primary concern is a severe headache. The ED team proceeds to get a CTA of the head and start BP control.
CTA showed 7mm ACA aneurysm with a grade 1 SAH.
Patient was taken for a craniotomy the next morning.
Mortality for SAH approaches 50%. Survivors have substantial neuro-cognitive disability. Missed diagnosis results in a 4-fold mortality increase at one year.
Important clinical clues include: headache with exertion, headache with actions that increase BP (cough/sneeze/straining), thunderclap headache, family HX of aneurysm or SAH. Smoking is a risk factor.
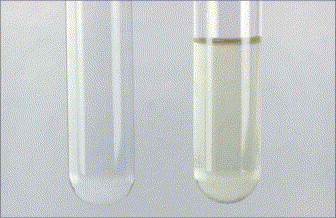
Harwood comment: The lab evaluation for xanthochromia is just a lab tech holding up the CSF in front of a white sheet of paper. They are looking for a yellow tinge to the CSF. In Europe, labs use spectrophotometry to determine if there is xanthochromia. Spectrophotometry is not the standard for identifying xanthochromia in the US.
*xanthochromia on the right
Harwood and Girzadas comments: The diagnostic approach of prioritizing a chest pain work up in a patient with HX of CAD and Aortic dissection is not unreasonable. The ED course was very appropriate. You went back and re-evaluated the patient when the work up was not fruitful and adjusted your diagnostic plan to evaluate the patient’s headache.
Bonder ICU Boarders Project
Unfortunately I missed most of this excellent presentation.
Drs. Bonder/Burt/Iannitelli have worked for months to develop a protocol to better manage ICU patients boarding in the ED. This protocol includes collaboration with our ICU colleagues, ED and ICU nursing staffs and technological support from EICU.
Drs. Bonder/Burt/Iannitelli were awarded the EMRA “Be the Change Grant” for their work.
Ophthalmology Lab