Paquette/Shroff Oral Boards
Case 1. 34yo female with fever. UCG is positive. UA shows signs of UTI. U/S shows SLIUP at 12 weeks. Treatment was initiated with IV fluids and IV Ceftriaxone. Pyelonephritis in the setting of pregnancy needs to be admitted.
Cse 2. 18 yo male brought in from school for feeling lightheaded with hypotension and bradycardia. A few weeks ago, the patient developed a febrile illness with associated rash after going on a camping trip.
Erythema Chronicum Migrans Rash
EKG showing 3rd Degree Heart Block on ED presentation
Diagnosis is Lyme Carditis with 3rd Degree heart block. Patient was admitted for monitoring and possible pacemeaker if needed. Patient was started on doxycycline.
Case 3. 33yo male with fever and cough. Patient notes some hemoptysis. He has had weight loss and night sweats.
CXR showing Left Upper Lobe Cavitary Infiltrate consistent with TB
Rapid HIV test was positive. Treatment initiated with anti-viral medications, antibiotics for CAP and TB. Very important that patient was placed in isolation. Patient was a guard in a prison so state department of public health needs to be notified.
Ohl M&M
I will only note the take-home points to protect the anonymity of the cases.
How we feel toward patients and their families can affect how we evaluate and manage a patient. If the patient or family are demanding or we find them arrogant or annoying or histrionic we can at times not accurately assess and evaluate them. We have to be on guard for these situations, recognize our own internal responses to patients, and do our best to mitigate these biases.
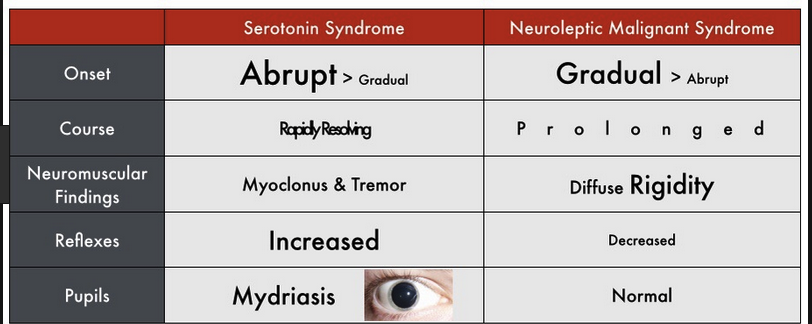
It can be difficult to differentiate NMS from Serotonin Syndrome. Rigid extremities or "lead pipe rigidity" are the common catch phrases on boards to signal NMS.
When you are getting ready to intubate, have a plan for back up. Slow down when doing intubations and think through your plan before starting the procedure. Have multiple options for back up. Assess the airway before you give medications. If you encounter difficulty and are contemplating doing a cric, remember LMA can act as a bridge device to provide oxygenation and ventilation until you can get the airway. If you are headed toward a cric in a difficult airway situation, don't wait too long. Most commonly physicians wait too long to start the cric procedure.
Andrea comment: If there is a study ordered/performed (CXR,EKG, Lab) on a patient, make sure you see it and review it. Thinking anthropomorphically about diagnostic testing, the diagnostic studies are trying to avoid being seen. The tests are trying to elude you or the disease is trying to hide the clue from you. They are hiding on the counter by the sims, or in the patient's file slot, or by the nurse's desk or in the patient's room or it was never done. You gotta find it to make the diagnosis.
Velamati Pediatric Resuscitation
In Pediatric Sepsis give 60ml/kg of fluids in 60 minutes using the pull/push method with a 30ml syringe. Stop at every 20ml/kg infused and re-assess patient to decide if they need more fluids.
The most common rhythm in pediatric arrest is Asystole. PEA is next most common, and VT/VF is third most common.
Use the PediStat App or the Broslow tape to cognitively unload your brain during pediatric codes.
100-120 chest compressions per minute in pediatric patients.
Sites for IO access in pediatric patients. The distal femur although not FDA approved is still a legit site for access especially in very small patients in which the tibia is very small.
The anatomic differences between the Pediatric and Adult airways. The narrowest point in the pediatric airway is the cricoid ring as opposed to the adult airway in which the cords are the narrowest point.
Infants will desat to less than 90% in about 2 minutes after pre-oxygenation. Use passive oxygenation with continuous nasal cannula O2 to prolong the safe apnea time.
Most young children will have improved airway visualization with this type of positioning with elevation of the thorax to accommodate the larger occiput.
This also seems like a great positioning approach but is a bit more complicated to set up.
Ketamine is probably the go-to induction agent for most indications in pediatric patients.
"Code 21" is the Airway Code for pediatric intubations. The PICU attending will respond to the "Code 21". You can also have Anesthesia respond if you want.
Felder/Naik/Schmitz Admin Update
Dragon devices within First Net are not working currently. This has gone up to the corporate level for a fix. A work-around is to use the older Dragon App that is opened outside of FirstNet.
Please continue your outstanding documentation of Face to Face evaluations of patients requiring restraint.
There is a continuous focus on and concern to improve on how slotting is done in the ED.
We discussed other challenges experienced in the ED
Thanks to Nancy Burke and our Nursing Colleagues for providing new refrigerators in the charting rooms!
Stanek Weight Discussions
Providers of health care have concerns about raising issues of body weight with their patients. They are concerned about how patients will react to these conversations.
When bringing up the topic of body weight it is best to be patient oriented.
1. First engage the patient in a non-medical topic to develop rapport
2. Discuss the weight issue upon re-evaluation not on first contact with patient
3. Ask, Has your primary care doctor had any discussion with you about your weight
4. Your weight places you at increased risk of adverse health problems.
5. Did you know that blood pressure, diabetes, and cholesterol problems are affected by your weight.
6. Give some simple suggestions for healthy living. Shop the perimeter of the store. Start an exercise that you like, for example walking 30min per day.
Florek Safety Lecture Glycemic Control in the ED
Type 1 diabetics are more likely to develop DKA. Type 1 diabetics who are spending prolonged time in the ED need to have their blood glucose monitored regularly and managed.
Glucose over 500 will likely be managed with Insulin and OBS/Admit
Glucose over 200 start sliding scale insulin or 0.1 U/kg of insulin
All diabetics boarding in the ED should have low dose sliding scale insulin ordered to prevent development of DKA.
Shroff Safety Lecture
It is important that patients are fully undressed and in a gown when the physician evaluates them. If the patient is in a gown, physicians are less likely to miss an injury or other physical finding.
Always have a chaperone when performing rectal, genital, breast exams.