HPI:
An 82 y/o woman with multiple sclerosis, history of DVT on Coumadin and chronic indwelling Foley is sent from nursing home for hypoxia. Patient is not on oxygen at nursing home. Her pulse Ox was low (83) at the nursing home, so they sent her away to Christ hospital. EMS said they put her on 15L oxygen on non-rebreather on the transfer.
Code 44 was called by nurse. On arrival, patient said she was sleeping. She has no clue why she is sent over to the hospital. She denies chest pain or shortness of breath or any symptoms. She has not been sick.
Physical Exam
Vitals: SpO2-92 on 15L oxygen via non-rebreather. RR: 18, BP 146/62, P 77.
Exam:
Gen: NAD. Very comfortable. Bluish skin
CVS: RRR
Pulm: CTAB
Abd: Non-tender, soft. Foley present. Orange urine in Foley bag.
Neuro: Patient can shrug shoulders but strength 1/5. Sensation diminished below shoulders (all are baseline)
Intervention
*Patient has hypoxia on SpO2 but she looks very good. Something does not fit quite right. ABG with panel was ordered on top of Code 44 labs.
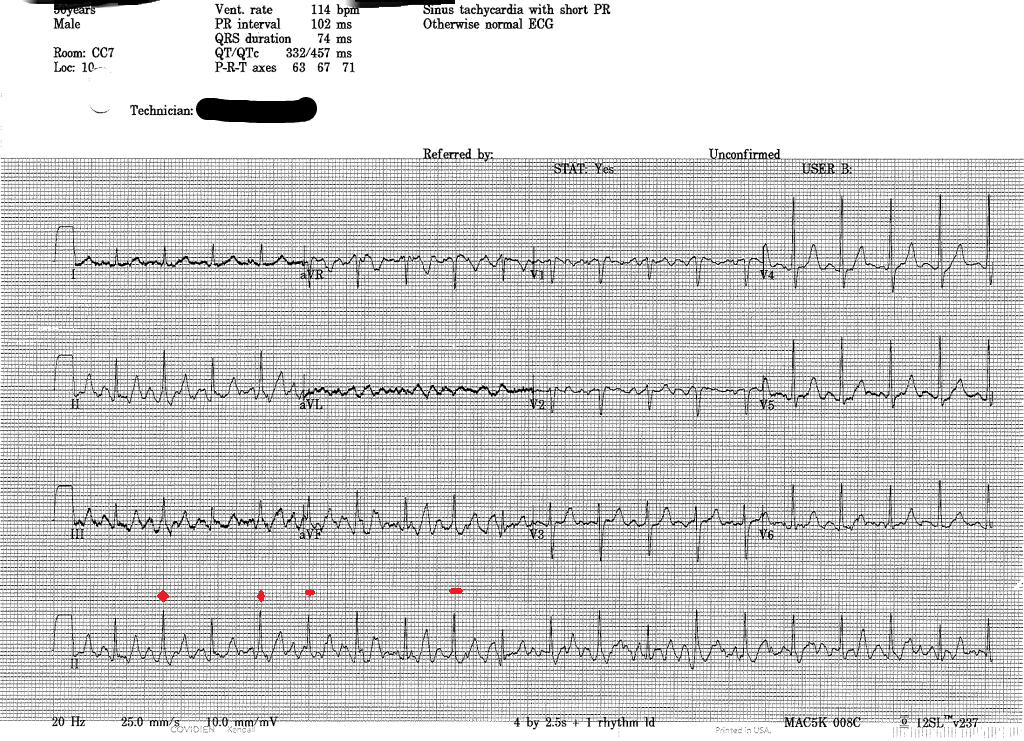
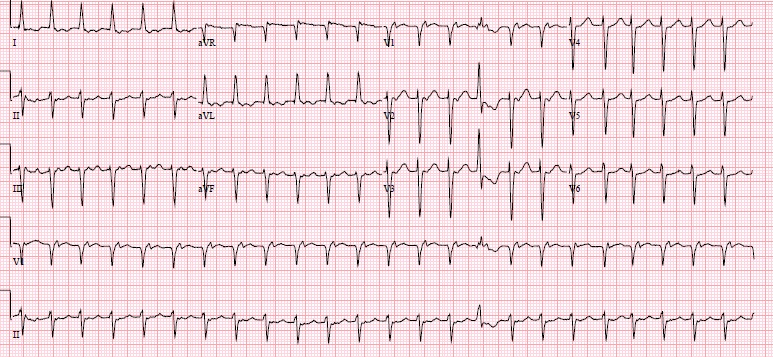
EKG: normal rate, normal sinus rhythm, no ischemia
CXR: normal without consolidation
ABG: pH 7.44, pCO2 44, pO2 461, HCO3 28, O2 sat 98, Carbonmonoxide 3.1, O2 content arterial 10 (Low), OxyHemoglobin 80.8, Methemoglobin 14.9 % (normal <1.2%)
Labs: normal BMP, normal CBC, and therapeutic INR: 2.3. Troponin: <0.02, BNP 30
Patient has methemoglobinemia. Everything now fits: the low pulse Ox, maybe questionable bluish skin and patient’s lack of symptoms.
What’s the culprit? We tried to remember the meds that can induce methemoglobinemia from board exams. Nitrous or Sulfa containing meds!
Well, let’s ask our pharmacist to look at her meds list. Luckily, our patient was a healthy MS patient. Besides warfarin and Baclofen, she was given 1 other medication by nursing home. Phenazopyridine (pyridium)!
Phenazopyridine (pyridium)
Phenazopyridine is a urinary tract analgesic and available over the counter. It is supposed to be used for 3 days in an acute treatment for patients with dysuria. This poor old lady was moved to nursing home 3 months ago. NH put her on a Foley since she has urinary incontinence due to MS, and when she complained of Foley irritating her urethra, they put her on Pyridium for 3 months.
Treatment: We started pushing IV methylene blue 1mg/kg and within minutes, her pulse Ox improved to 98 on room air.
Patient update: Daughters came to thank the ER doctor months later. They moved their mom to a different nursing home. She is doing well.
Methemoglobinemia (UpToDate)
Diagnosis: Methemoglobin level on ABG, normally methemoglobin levels <1%
Pathophys: Ferrous (Fe 2+) in heme group of hemoglobin is oxidized to the ferric state (Fe 3+). This converts hemoglobin into methemoglobin, which CAN’T bind oxygen. In addition, oxygen affinity of any remaining ferrous hemes is increased, shifting the oxygen dissociation curve to the left, so oxygen can’t be delivered to tissues. => The patient has greater functional anemia.
Acquired Causes: oxidizing agents (medications): nitrites, nitroglycerin, nitroprusside, Bactrim, benzocaine, inhaled nitric oxide, aniline and its derivatives etc. Dapsone and topical anesthetics appear to be most common precipitating agents.
Congenital Cause: Congenital methemoglobinemia is characterized by diminished enzymatic reduction of methemoglobin back to functional hemoglobin. Affected patients appear cyanotic but are generally asymptomatic.
There is a family that lived in the hills of Kentucky known as “Blue Fugates.” They have a congenital deficiency in the enzyme causing them to have methemoglobinemia. It is autosomal recessive but this family intermarries, so viola..
http://abcnews.go.com/Health/blue-skinned-people-kentucky-reveal-todays-genetic-lesson/story?id=15759819#.T5sgQnr-mVo
Treatment:
-Asymptomatic: discontinue the offending agent
- Symptomatic or methemoglobin level>20%: IV methylene blue 1-2 mg/kg can be given over 5 minutes. Response is rapid. A second dose may be repeated in one hour but retreatment is often not necessary.
-Blood transfusion or exchange transfusion may be helpful in people who are in shock. Hyperbaric oxygen has been used with anecdotal success in severe cases.
Although ascorbic acid is an answer on board questions, it is a less effective treatment than methylene blue.
Symptoms:
- Methemoglobin>15%: cyanosis, asymptomatic
- >30%, fatigue, headache, dizziness, tachycardia, weakness
- >55%: dyspnea, bradycardia, seizures, coma
- >70%: death
What about pyridium?
- Pyridium has been reported sparingly in medical literature as a cause of methemoglobinemia, either as an acute overdose or in patients with prolonged therapeutic use.
Take Home Points:
- Methemoglobinemia on board questions: pulse Ox 87 no matter how much oxygen is given. Blood itself is chocolate-colored. Get ABG with panel.
- It is often drug induced. Topical anesthetic (patients coming from GI procedure) or TMP-SMX are common meds.
- Treatment: IV methylene blue 1-2mg/kg x 1