McKean/Schmitz
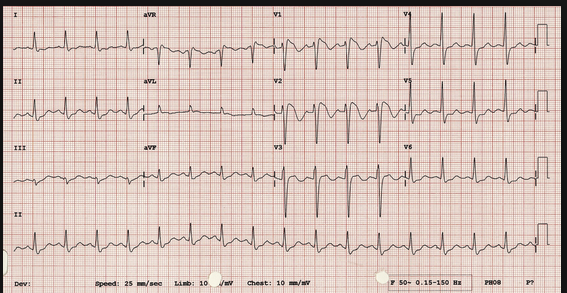
Case 1. Digoxin poisoning from botanical cardiac glycoside. Child was bradycardic and EKG showed bradycardia and heart block.
2nd Degree heart block. 2:1 block. Can't determine whether it is Mobitz I or II based on this ECG.
Andrea comment: For boards, he most common plant that will cause botanical glycoside toxicity is Oleander.
Case 2. Black widow envenomation. 75% of bites are on extremities and are asymptomatic. For patients with significant pain and vital sign abnormalities, antivenom can be a critical treatment modality. Andrea comment: No hospitals have black widow antivenom on site. You will need to call poison control. Poison control will get antivenom from the zoo. Calcium is no benefit for black widow spider envenomation. Benzo's however, can symptomatically improve the muscle spasm.
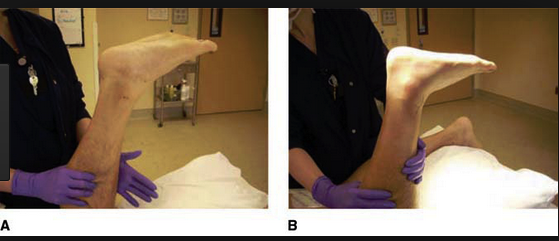
Case 3. Achilles tendon rupture can be diagnosed with Thompson's Test. (96% sensitive, 93% specific).
Picture A shows normal plantar flexion with squeezing the calf=negative Thompson's Test. Picture B shows no plantar flexion with squeezing the calf=positive Thompson's Test. Edtor's note: I can never remember which is positive and which is negative. So in the chart I write Thompson's test showed intact Achilles tendon function. Or, Thompson's test indicated Achilles tendon rupture. For the Thompson's test to be valid you need to have the knee flexed. So either lay the patient on their stomach and flex their knee or have them kneel with one knee on a chair or cart.
Lee M&M
No case details, just some take home lessons.
Hypotension in association with aortic dissection indicates either the patient has an ascending aortic dissection with pericardial tamponade or the patient has a surgical indication for a type B dissection. Either way consult Cardiothoracic surgery.
Cardiothoracic surgery is the service to consult for suspected aortic dissections.
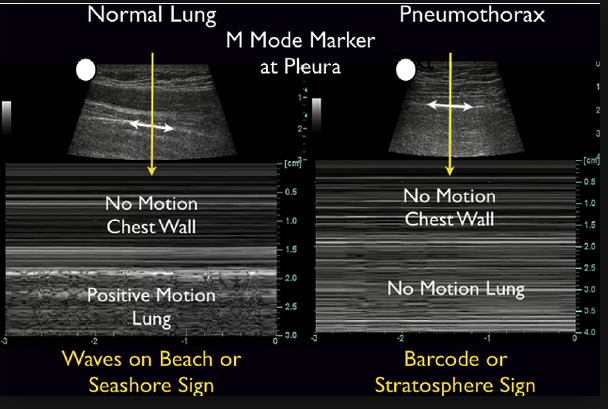
Do a bedside echo on patients on whom you have concern for aortic dissection and all critically ill patients. Elise comment: Do serial bedside echo's to determine if pericardial fluid is accumulating. This can help identify a dissection of the ascending aorta. Elise Hart comment: TEE has high sensitivity for identification of ascending aortic dissection.
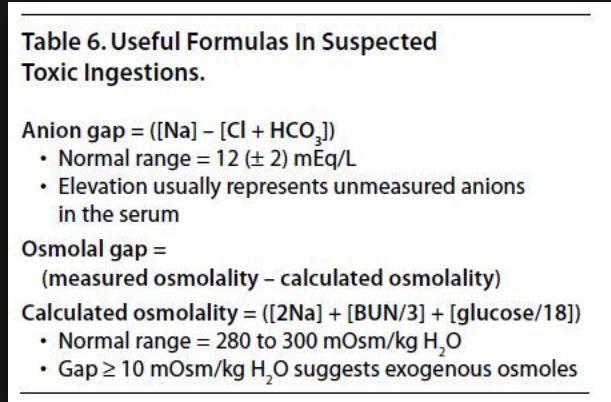
Dr. Lee then lead a fascinating discussion about the clinical situation of very high levels of ethanol intoxication and concern for toxic alcohol ingestion. Very high levels of ethanol can cause death by respiratory depression, and at levels around 600, cardiovascular instability. There are two online osmolar gap calculators when you do a google search, 1. University of Iowa and 2. MD Calc. The University of Iowa calculator uses a different calculation than MD Calc. It uses a conversion factor of 1.2 to account for some invitro studies that showed very high levels of alcohol affect the osmolar gap. Andrea said that this new calculation used by the University of Iowa Calculator has not been fully validated. She feels the MD Calc osmolar gap calculator is safer for patients.
Traditional Osmolar gap calculation used by MD Calc calculator.
To account for ETOH, this formula uses 1.2 x ETOH/4.6
University of Iowa Calculator. Andrea felt this calculator is not ready for prime time. Harwood is going touse this calculator. He feels it cuts down on the number of patients who need to have fomepizole and dialysis.
Serum alcohol level only measures ethanol. Toxic alcohol ingestion has no impact on the blood alcohol level.
Chinwala 5 Slide Follow Up
Diagnostic algorithm forAnaphylaxis
To quote Dr. Chinwala, "EPI is King" when treating anaphylaxis.
Hart/Regan Ortho Updates
Segond Fracture is highly associated with ACL tear and meniscal injuries.
This is one of the most common ankle fractures in snowboarders. It was a rare high-energy type injury prior to the sport of snowboarding.
Quadricep tendon ruptures are more common than patellar tendon ruptures.
Donapudi 5 Slide Follow Up
Treatment priorities for cholangitis: Agressive fluid resuscitation (think sepsis fluids), broad spectrum antibiotics, ERCP, and long term the patient will need cholecystectomy. In patients who are not good surgical candidates acutely, IR can place a percutaneus drain to get source control of an infected gall bladder. It is prudent to consult GI and General Surgery on all cholangitis patients.
Predictors of need for ERCP: High bilirubin, thrombocytopenia, low albumin, and tachycardia.
Friend 5 Slide Follow Up
Vitamin K deficiency affects factors 2,5,7 ,9, 10, C, and S. Vitamin K deficiency acts like a warfarin overdose. It is rare in healthy adults. It can be caused by antibiotics, fat malabsorbtion, high doses of vitamins A and E. Factor 7 is the factor affected most early and severely due to vitamin K deficiency or warfarin overdose.
Erbach 5 Slide Follow Up
Brain AVM's present with bleeding or seizures.
AVM's are a high pressure malformation. When they rupture they have big bleeds. Cavernous Malformations are relatively low pressure malformations and present with seizures and smaller bleeds.
Olfactory hallucinations are associated with temporal lobe seizures.
Denk Safety Lecture How to determine if a patient has fluid responsive septic shock
Fluid responsiveness is defined by increase in stroke volume of 10-15% with a 500ml fluid bolus.
There are new gadgets that can determine fluid responsiveness: The EV-1000 can calculate stroke volume variation based on non-invasive finger probe readings. The problem with this device is that patients have to be in sinus rhythm, not tachycardic, and have to be intubated to get accurate readings.
The other device is the Cheetah NiCom.
There is no Tech fix or fool proof way to measure fluid responsiveness in septic patients. We need to continually re-evaluate our septic patients. Give fluids mindfully and assess the patients' response to fluids.
Elise comment: From our Process Trial experience, most septic shock patients whether or not they have heart disease, CHF or ESRD can tolerate 30ml/kg of fluids. You need to frequently re-evaluate these patients. But in general give 30ml/kg for septic shock.