Carlson/Kennedy Oral Boards
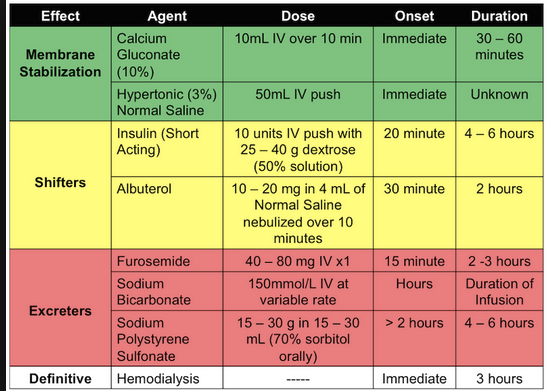
Case 1. 67yo male with back pain and lethargy. He also has lower extremity weakness. ESR was elevated. Imaging showed multiple lytic lesions in the spine. Patient had hypercalcemia secondary to multiple myeloma. Critical actions were to diagnose multiple myeloma with hypercalcemia and treat with IV saline.
*Hypercalcemia symptoms
*Hypercalemia management
*Multiple myeloma
Case 2. 22 month old female presents with parent saying she cannot wake the child up. BP 52/26 HR 162, shallow respirations. Accuchek is 28. History reveals that older sibling is taking phenobarbital. CXR shows non-cardiogenic pulmonary edema. Patient required glucose supplementation and intubation. Hypothermia was also treated. Urine was alkalinized. Multi-dose activated charcoal can be useful with phenobarbital ingestions. Diagnosis was child abuse. Mom was giving phenobarbital to keep child calm and to sleep. Child was placed in protective custody.
*Multi-dose Activate Charcoal MnemonicsABCD for the toxins it works for. PHAILS for the toxins that charcoal does not work for.
Case 3. 30mo male who is vomiting after taking his vitamins. The vitamins contained ferrous fumarate. However, calculations showed the amount the child ingested was not toxic. If child takes less than 60mg/kg the ingestion should be non-toxic. A serum iron level < 500 is non-toxic. You can get vomiting with a non-toxic dose of iron. A toxic dose typically will cause an anion gap acidosis. This patient did not have an elevated anion gap. Andrea made the point to get the numbers 60mg/kg and an iron level of 500 in your head regarding iron poisoning.
C & EKulstad CV Study Guide
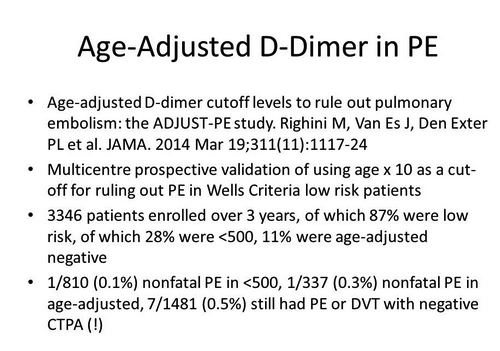
*Age adjusted d-dimer EBM
The test to evaluate for pelvic thrombosis in pregnant patients is MRI. It may be the best study as well for identifying pelvic thrombosis in non-pregnant patients.
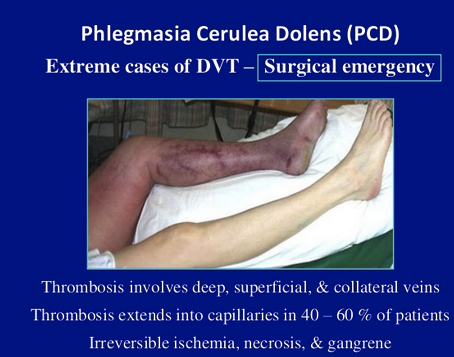
*phlegmasia cerulean dolens
*phlegmasia alba dolens
Wikipedia: The disease presumably begins with a deep vein thrombosis that progresses to total occlusion of the deep venous system. It is at this stage that it is called phlegmasia alba dolens. It is a sudden (acute) process. The leg, then, must rely on the superficial venous system for drainage. The superficial system is not
adequate to handle the large volume of blood being delivered to the leg via the arterial system. The result is edema, pain and a white appearance (alba) of the leg.
The next step in the disease progression is occlusion of the superficial venous system, thereby preventing all venous outflow from the extremity. At this stage it is called phlegmasia cerulea dolens (PAD). The leg becomes more swollen and increasingly more painful. Additionally, the edema and loss of venous outflow impedes the arterial inflow. Ischemia with progression to gangrene are potential consequence. ePhlegmasia alba dolens is distinguished, clinically, from phlegmasia cerulea dolens (PCD) in that there is no ischemia.[1]
Emedicine/Medscape: In PAD, the thrombosis involves only major deep venous channels of the extremity, thus sparing collateral veins. The venous drainage is decreased but still present; the lack of cyanosis differentiates this entity from PCD. In PCD, the thrombosis extends to collateral veins, resulting in severe venous congestion with massive fluid sequestration and more significant edema. Without established gangrene, these phases are reversible if proper measures are taken.
Of PCD cases, 40-60% also have capillary involvement, which results in irreversible venous gangrene that involves the skin, subcutaneous tissue, or muscle.[3] Under these conditions, the hydrostatic pressure in arterial and venous capillaries exceeds the oncotic pressure, causing fluid sequestration in the interstitium. Venous pressure may increase rapidly, as much as 16- to 17-fold within 6 hours.[4
Elise comment: You now need to treat superficial thrombophlebitis with heparin or LMWH or one of the new oral anticoagulants if the thrombophlebitis is large or proximal.
From the ACMCEM website: Thrombosis of superficial veins has long been considered benign, and deemed a separate entity from venous thromboemolism (VTE)
-- However, multiple studies illustrate a significant association with VTE (DVT and PE).
-- When patient with ST (diagnosed clinically, no ultrasound) are thoroughly evaluated, the degree and the extent of clot are underestimated 75% of the time. Further, such patients are found to have co-existent DVT or PE 25% of the time and/or rapidly progress to DVT 10% of the time.
---- Teaching point: get ultrasounds on all clinical superficial thrombophlebitis
-- The risk factors for ST and VTE are the same, and many argue that ST should be treated the same as VTE.
-- In general,
anticoagulate (as you would for DVT) the patient if they have known clotting risk factors, greater than 5 cm of clot, or clot < 5 cm within the sapheno-femoral or sapheno-popliteal junction.
-- Another way to think about it is that a superficial vein thrombosis is a manifestation of a systemic clotting cascade gone awry. To even further simplify things, seems pretty pathologic to have any blood vessel clot; ahh hello, you are clotting off blood vessels.
*Treatment algorithm for superficial thrombophlebitis
The treatment of pulmonary edema is high dose IV NTG or sublingual NTG as the mainstay of therapy. Aggressive use of NTG allows us to avoid intubating pulmonary edema patients.
Morphine has no efficacy in the management of CHF.
*OESIL Rule for syncope is considered better than San Francisco Syncope Rule
*Rose Rule Elise likes the Rose Rule for syncope. She made the point that an elevated BNP is a marker for badness in syncope and can be a surrogate for CHF.
*Hypertrophic Cardiomyopathy Patients have LVH QRS complexes with lateral inverted T waves.
Treat pericarditis with colchicine.
Hart/Regan 2015 ACLS Updates
Social media can be used to summon rescuers.
Christine, Erik and Elise spoke about an app called Pulse Point that will notify you of a nearby cardiac arrest.
*Pulse Point App
Do Chest compressions 100-120 per minute. Compressions at a pace over 120 has a worse outcome.
Avoid leaning on chest to allow full recoil.
Vasopressin is out. It has no advantage over epinephrine.
We discussed automated CPR machines. Faculty present at the meeting have found them more reliable with less interruptions anecdotally, but the research does not show any benefit over human CPR.
Routine use of lidocaine is not recommended.
If ETCO2 is <10 after 20 min of downtime ROSC is unlikely
ECMO can be used in cardiac arrest with a potentially reversible cause (hypothermia, myocarditis, transplant candidate)
Any post-arrest patient not responding to verbal stimuli should be cooled to 32-36C.
Avoid and treat hypotension in a patient who had ROSC.
ACLS Workshop
McGinnis MIDAS Reporting Update
Please place any patient safety concerns in the MIDAS system. We really want you to make a report of any safety issues.
When placing a bed request, please check the special request drop down menu to be sure you make note of suicidal patient needing a sitter, peritoneal dialysis, LVAD, chronic trach, c-diff, andother isolation needs. These requestswill limit the patient to certain floors that can provide that specialized care.